Personalized medicine was born in 1997 when the Food and Drug Administration first approved a molecularly targeted treatment, IDEC Pharmaceutical’s rituximab, a monoclonal antibody against protein CD20 found on B cells, for the treatment of CD20-positive B-cell non-Hodgkin’s lymphoma. The following year marked the first time the FDA would grant simultaneous approval of targeted treatment, Genentech’s Herceptin breast cancer therapy, with its companion diagnostic test, HercepTest, to identify eligible patients with increased human epidermal growth factor receptor 2 (HER2).
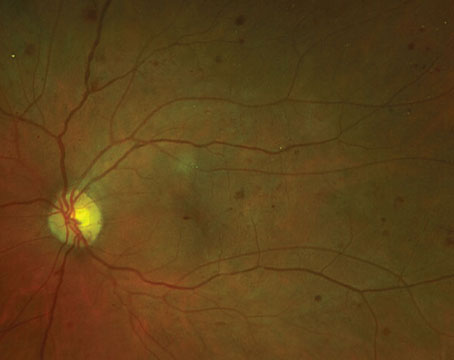
The era of personalized medicine in retinal disease was heralded by a landmark genetic finding. Throughout evolution, millions of mutations have accumulated in the human genome and approximately 12 million of these sites have been identified. These variations, known as Single Nucleotide Polymorphisms (SNPs), are single base changes in a DNA sequence that occur relatively frequently in the human population (>1 percent). Genome-wide association studies (GWAS) compare the entire genome from cases to that of controls to find associations between SNPs or other genetic variations and diseases. This approach differs from the candidate gene approach, in which variation in pre-specified candidate genes are compared to phenotypes. The first successful GWAS occurred in age-related macular degeneration and was published in 2005, assessing 116,204 SNPs in 96 AMD patients and 50 controls. This landmark study noted that a common variant in the complement factor H gene was strongly associated with AMD, with individuals homozygous for the risk allele possessing increased risk of AMD by a factor of 7.42
| Regulatory and Payment Issues Surrounding Personalized Companion Diagnostic Testing |
| There are significant barriers to the development of companion diagnostic tests, which are so crucial to progress in personalized medicine. Although 30 percent of all drugs in Phase III testing rely on a biomarker to determine which patients respond to the drug, traditional payment models are misaligned with personalized medicine diagnostics on several levels. First, existing coding and payment structures, often structured years ago, do not accurately describe novel companion diagnostic tests or their value. For example, if a CPT code already existed for a similar diagnostic test, it may be poorly aligned with the new diagnostic test or reimburse far too low to economically facilitate the test. Second, the regulatory environment is poorly structured for integration of a complex and expensive companion diagnostic test into new treatment paradigms. For example, a diagnostic test must be Food and Drug Administration-approved before a new CPT code application can be completed, which is successful only 70 percent of the time, requiring 18 to 24 months, and oftentimes yielding only modest reimbursement. Consequently, the reimbursement is often not sufficient for the cost of the test. Third, obtaining approval for a new diagnostic test is highly complex. Oversight of diagnostic tests and medications is handled by different agencies, which have historically been poorly integrated and involved a complex approval process. Medications are regulated by the Center for Drug Evaluation and Research, which reviews new drug applications (NDAs), and the Center for Biologics Evaluation and Research (CBER), which regulates biologic agents such as blood products, tissue-based products, therapeutic proteins and vaccines. Diagnostic tests are regulated by the Center for Devices and Radiological Health (CDRH), which is under the FDA, and the Centers for Medicare & Medicaid Services, which is autonomous from the FDA. Fourth, for in vitro diagnostic products, there are two pathways leading to approval: the 510K pathway for class II, lower-risk devices; and the premarket approval pathway for higher-risk, class III devices. Most screening, diagnostic and prognostic diagnostic IVDs are class II, while IVDs to select patients for specific therapeutics are class III. Consequently, given these complex and differing pathways, it is difficult to time approval for a new therapeutic along with its companion diagnostic test. Furthermore, it is unclear who is responsible for paying for the tests; the significant costs of these diagnostic tests can be borne by traditional payers, by patient advocacy or disease-state groups, as in the case of cystic fibrosis, or by the pharmaceutical companies who benefit from the successful use of their drug. Finally, coverage decisions differ somewhat between CMS and private payers. For CMS, coding and payment processes are influenced by subspecialty societies, which often protect the interest of their constituents. For private payers, committees, familiar with therapeutics but not familiar with companion diagnostic tests, influence these decisions. In the future, the simplest payment strategy for companion diagnostics is a bundled payment to the pharmaceutical company. Companion diagnostic tests influenced more than 60 percent of critical health-care treatment decisions in 2011, but accounted for only 2 percent of health-care spending worldwide. Since patient-specific chemotherapies, or similar agents that are often given over periods of time, can cost many multiples of the one-time companion diagnostic test, the pharmaceutical company may be in the best position to administrate the bundle payments and to address the appropriateness of competing companion diagnostic tests. A payment bundle solves the misaligned payment model for companion diagnostic testing in several ways. First, the bundle itself creates value by directly linking the companion diagnostic test with the treatment, circumventing all of the time and labor-consuming issues surrounding billing, collection and payment. Second, by streamlining the reimbursement process, the bundle promotes testing and subsequent prompt and appropriate treatment, in the patient-specific manner of personalized medicine, enhancing the quality of care for patients. Third, the bundle would benefit both the pharmaceutical and companion diagnostic companies, as their products would be more readily adopted into clinical practice, enhancing the appropriate use of their products. Finally, this would further stimulate the companion diagnostic testing industry, enhancing personalized medicine systematically. —T.A.C. |
AMD has an exceedingly strong genetic contribution with about 15 SNPs accounting for most of the disease risk.8-12 Commercially available tests assess a cheek swab for SNPs within the four major metabolic pathways involved in AMD pathogenesis: the complement cascade (CFH, CFI, CFB, C2, C3); oxygen metabolism (ARMS2); cholesterol metabolism (LIPC, APOE, CETP, ABCA1); and extracellular matrix (TIMP3, COL8A1). Algorithms incorporating these SNPs, along with non-genetic factors, such as age, smoking, fellow-eye status and body mass index, can assess a patient’s risk for progression to advanced AMD.13
Using this approach, Carl Awh, MD, and associates recently reanalyzed data from the Age-Related Eye Disease Study to derive a personalized medicine approach to nutritional supplementation in AMD.14,15 In the AREDS study, participants were randomly assigned to placebo or dietary supplementation with antioxidants (β-carotene, 15 mg; vitamin C, 500 mg; and vitamin E, 400 IU), zinc (80 mg as zinc oxide and copper 2 mg), and antioxidants and zinc combined. Of the 2,258 subjects with category 3 disease, 995 subjects had genetic information available, and both CFH and ARMS2 were assessed. The authors concluded, “In this analysis, patients with no CFH risk alleles and with one or two ARMS2 risk alleles derived maximum benefit from zinc-only supplementation. Patients with one or two CFH risk alleles and no ARMS2 risk alleles derived maximum benefit from antioxidant-only supplementation; treatment with zinc was associated with increased progression to advanced AMD. These recommendations could lead to improved outcomes through genotype-directed therapy.”14 This genotype-guided approach to nutritional supplementation generated some controversy, as other experts have pointed out that AREDS was not designed to assess this issue, and that this secondary statistical analysis may not be appropriate to warrant a change in current guidelines.16,17 Nevertheless, this personalized medicine approach to nutritional supplementation represents an intriguing beginning, with more research to follow.
Genotype information involving complement risk alleles has been shown in one study to correlate with treatment response in geographic atrophy. In 129 subjects with geographic atrophy, Genentech/Roche’s MAHALO study assessed lampalizumab, a monoclonal antibody fragment that inhibits the alternative complement pathway by binding to complement factor D. At month 18, a 20.4-percent reduction in geographic atrophy area progression was reported in the all-comer, lampalizumab monthly arm relative to the pooled, sham arm. However, in the complement factor I (CFI) positive subpopulation, there was an even greater, 44-percent reduction. Based on these positive Phase II results, Genentech/Roche has commenced Phase III Chroma/Spectri studies of lampalizumab in geographic atrophy and will incorporate genotype testing. Someday, treatment of geographic atrophy may involve a personalized medicine companion test for genotype-testing in order to select subpopulations of positive responders.
The ultimate form of personalized medicine in retinal disease involves genetically altering retinal cells. Gene therapy in the retina involves injecting viral vectors that transfect target cells with DNA to produce desired proteins. A common viral vector is the adeno-associated virus, which does not cause disease. Gene replacement has been studied most extensively in Leber’s congenital amaurosis, an autosomal recessive retinal dystrophy characterized by severely decreased vision, nystagmus and severely extinguished electroretinogram within six months of birth. One group has extensively studied subretinal gene therapy in the RPE65 form of LCA using recombinant adeno-associated virus 2 (rAAV2) carrying the RPE65 gene. Visual function improved in all patients to different degrees, and cone and rod sensitivities increased significantly in the study eyes but not in the control eyes; however, photoreceptor degeneration continued to progress over the ensuing years, despite the improved visual acuity.18-21
In wet AMD, two approaches are currently being studied, an intravitreal injection and a subretinal injection of an AAV containing genes encoding anti-vascular endothelial growth factor therapies. The secreted extracellular domain of sFlt-1, a soluble isoform of the VEGF receptor 1, is a naturally occurring protein antagonist of VEGF. Genzyme is studying an intravitreal AAV2-sFlt-1 injection gene therapy for the treatment of wet AMD. Avalanche Biotech is studying single subretinal injection gene therapy for the treatment of wet AMD. AAV2-sFlt-1 consists of the AAV2 vector, which contains a gene encoding sFlt-1, to eliminate or limit the need for anti-VEGF injection therapy. Its recent 12-month Phase IIa study in wet AMD included 21 subjects in the treatment group and 11 subjects in the control group, all of whom received two initial monthly ranibizumab injections, followed by rescue ranibizumab injections based on pre-specified criteria. Treated subjects showed better results compared to control subjects in multiple criteria, including change in best corrected visual acuity, change in retinal thickness and number of rescue injections.
Currently, there are numerous trials assessing gene therapy in retinal disease including Leber’s hereditary optic neuropathy; gyrate atrophy; choroidemia; X-linked retinoschisis; and Stargardt’s disease. In the future, it is clear that personalized medicine will dramatically alter the treatment of retinal disorders. Eric Topol’s prediction of the creative destruction of medicine may very well be realized in the retina specialist’s clinic, in which genetic information will determine how best to treat the right patient, at the right time, with the right therapy, sometimes even altering the genetic makeup of the retina to obviate the need for repeated injection therapy. This approach may dramatically increase the quality of care while potentially lowering costs. REVIEW
Dr. Ciulla practices in the retina section of Midwest Eye Institute, 200 West 103rd St. Indianapolis, IN 46290. Phone: (317) 817 1822; fax: (317) 817 1898. He is a member of the volunteer clinical faculty at Indiana University Department of Ophthalmology. He can be reached at thomasciulla@gmail.com.
1. Topol EJ. The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care. 2012, New York: Basic Books, 2012:303.
2. Klein R, Zeiss C, Chew E, Tsai J, et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005;308(5720):385-9.
3. Nozaki M, Raisler B, Sakurai E, Sarma J, et al. Drusen complement components C3a and C5a promote choroidal neovascularization. Proc Natl Acad Sci U S A 2006 Feb 14;103(7):2328-33. Epub 2006 Feb 1.
4. Mullins R, Aptsiauri N, Hageman G. Structure and composition of drusen associated with glomerulonephritis: implications for the role of complement activation in drusen biogenesis. Eye (Lond) 2001;15(Pt 3):390-5.
5. Johnson L, Leitner W, Staples M, Anderson D, et al. Complement activation and inflammatory processes in Drusen formation and age related macular degeneration. Exp Eye Res 2001 Dec;73(6):887-96.
6. Johnson L, Forest D, Banna C, Radeke C, et al. Cell culture model that mimics drusen formation and triggers complement activation associated with age-related macular degeneration. Proc Natl Acad Sci U S A 2011;108(45):18277-82.
7. Francis P, Schultz D, Hamon S, Ott J, et al., Haplotypes in the complement factor H (CFH) gene: associations with drusen and advanced age-related macular degeneration. PLoS One 2007 Nov 28;2(11):e1197.
8. Maller J, George S, Purcell S, Fagerness J, et al. Common variation in three genes, including a noncoding variant in CFH, strongly influences risk of age-related macular degeneration. Nat Genet 2006 Sep;38(9):1055-9. Epub 2006 Aug 27.
9. Seddon J, Francis P, George S, Schultz D, et al. Association of CFH Y402H and LOC387715 A69S with progression of age-related macular degeneration. JAMA 2007;297(16):1793-800.
10. Neale B, Fagerness J, Reynolds R, Sobrin L, et al. Genome-wide association study of advanced age-related macular degeneration identifies a role of the hepatic lipase gene (LIPC). Proc Natl Acad Sci U S A 2010;107(16):7395-400.
11. Seddon J, Reynolds R, Maller J, Fagerness J, et al. Prediction model for prevalence and incidence of advanced age-related macular degeneration based on genetic, demographic, and environmental variables. Invest Ophthalmol Vis Sci 2009;50(5):2044-53.
12. Chen W, Stambolian D, Edwards A, Branham K, et al. Genetic variants near TIMP3 and high-density lipoprotein-associated loci influence susceptibility to age-related macular degeneration. Proc Natl Acad Sci U S A 2010;107(16):7401-6.
13. Yu Y, Reynolds R, Rosner B, Daly M, et al. Prospective assessment of genetic effects on progression to different stages of age-related macular degeneration using multistate Markov models. Invest Ophthalmol Vis Sci 2012;53(3):1548-56.
14. Awh C, Lane A, Hawken S, Zanke B, et al. CFH and ARMS2 genetic polymorphisms predict response to antioxidants and zinc in patients with age-related macular degeneration. Ophthalmology 2013;120:2317-23.
15. Awh C, Hawken S, Zanke B. Treatment response to antioxidants and zinc based on CFH and ARMS2 genetic risk allele number in the Age-Related Eye Disease Study. Ophthalmology, 2015. 122(1): p. 162-9.
16. Chew E, Klein M, Clemons T, Agrón E, et al., No clinically significant association between CFH and ARMS2 genotypes and response to nutritional supplements: AREDS report number 38. Ophthalmology 2014;121:2173-80.
17. Chew E, Klein M, Clemons T, Agrón E, et al. Genetic testing in persons with age-related macular degeneration and the use of the AREDS supplements: To test or not to test? Ophthalmology 2015;122:212-5.
18. Jacobson S, Cideciyan A, Ratnakaram R, Heon E, et al. Gene therapy for leber congenital amaurosis caused by RPE65 mutations: safety and efficacy in 15 children and adults followed up to 3 years. Arch Ophthalmol 2012;130:9-24.
19. Hufnagel R, Ahmed Z, Corrêa Z, Sisk RA. Gene therapy for Leber congenital amaurosis: Advances and future directions. Graefe’s Arch Clin Exp Ophthalmol 2012;250(8):1117-28.
20. Cideciyan A, Jacobson S, Beltran W, Sumaroka A, et al. Human retinal gene therapy for Leber congenital amaurosis shows advancing retinal degeneration despite enduring visual improvement. Proc Natl Acad Sci U S A 2013;110(6):E517-25.
21. Cideciyan A. Leber congenital amaurosis due to RPE65 mutations and its treatment with gene therapy. Prog Retin Eye Res 2010;29(5):398-427.