Performing anterior segment surgery on a patient with a history of herpes flare-ups can be like walking through a minefield—any step could trigger disaster. Some patients need to have surgery, though, and the risk of not having the procedure outweigh those of a herpes recurrence. In this article, corneal specialists share their tips and tactics for managing these patients so you can minimize the chance of a flare-up that could complicate a good surgical outcome.
Herpes’ Risks
Surgeons explain what’s at stake when operating on a patient with a history of herpes.
“One of the worries is more exuberant inflammation right after surgery,” explains Asha Balakrishnan, MD, a corneal specialist in Encino, California, “because these patients are more pro-inflammatory. Also, we worry about them having any sort of reactivation that leads to visual decompensation and scarring in the cornea. Patients with reactivations can also develop keratitis, conjunctivitis or uveitis, each of which has its own sequellae. Also, sometimes, if a patient’s herpes reactivates, it takes much longer to get the eye quiet, if it’s possible. There are also intraocular pressure
Preop Considerations
Physicians say knowing the date of the last herpes flare-up is crucial when planning the surgery.
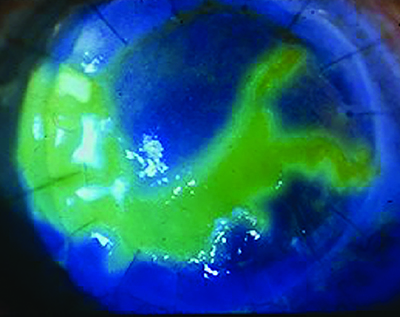 |
| Herpes simplex keratitis. |
“If there’s been no herpes simplex-related anterior segment activity for at least six months, you can consider doing cataract surgery,” says Thomas John, MD,
Some surgeons won’t do excimer laser refractive surgery in these patients at all. “LASIK and PRK are elective,” says Natalie Afshari, MD, chief of cornea and refractive surgery at UC-San Diego’s Shiley Eye Institute. “The epithelium may have a hard time healing with PRK, and with LASIK there can be interface issues, so if a patient has a history of herpes, I won’t do these procedures on him.” She warns to be careful when doing PTK in certain corneal scar cases. “There are some scars that people don’t realize are from herpes, and patients may get PTK to remove them,” Dr. Afshari notes. “But then the problem is the epithelium doesn’t heal afterward because it was a neurotrophic cornea, with decreased sensation, and the patient’s problems can get even bigger. I actually tell my fellows during their exit interview to watch out for those HSV scars—you can’t erase them like other scars because they don’t have
In patients that you suspect may have had herpes flare-ups in the past, surgeons say a corneal sensation test can be helpful. “I like to perform it myself,” says Dr. Balakrishnan. “I approach the eye from the side with a cotton-tipped applicator on which I’ve created a thin wisp of cotton by
Dr. Balakrishnan says she’ll consider refractive surgery, but whether she’ll do it depends on several factors. “If we’re talking about the kind of patient who has had a keratitis as a manifestation of the disease, I’d definitely proceed with caution with an excimer laser, and if someone has a history of recurrent herpetic keratitis, I’d strongly reconsider whether the surgery was a smart idea. But if the patient only had one episode and hasn’t had it again for a long time, and it was never corneal, I’d perform it with antiviral coverage (detailed below). My concern with the excimer is, for someone who’s had a herpes manifestation, we’re really stimulating the tissue with that laser. It seems like the perfect situation for triggering a reactivation.”
Dr. Balakrishnan notes that, since these patients may have had corneal involvement during their herpes outbreak, the effects could still be present. “Take the time to really get to know the course of the patient’s disease,” she says. “Pay attention to the corneal topographies in patients who have had prior herpetic keratitis. If you don’t do a corneal
As with most preop regimens, the ocular surface requires attention. However, due to particular aspects of herpes, the surface may need more attention than usual.
“If a patient has a history of herpes keratitis, the corneal sensation will usually be decreased in that eye, and a decrease in corneal sensation can contribute to dry eyes,” says Dr. John. “So, if the patient also has some other issue such as ocular-surface disease, you’ll have compounding factors at work, all of which can have a deleterious effect on vision even in an otherwise uneventful cataract or refractive surgery. Though you should optimize the ocular surface as you would for any cataract patient, you also have to let them know that the
“The key is getting the patient to understand the potential risk of reactivation and how it could impact his or her daily activities. If their friend had cataract surgery and went back to work quickly, and that’s their expectation, but suddenly they experience a herpes keratitis reactivation and have a prolonged postop treatment phase, they may be less than happy with the overall surgical experience. A well-informed patient is of paramount importance when it comes to patient satisfaction and ultimately a happy patient.”
Antiviral Prophylaxis
Other than making sure
“If the patient has a history of previous HSV, we often consider giving prophylactic acyclovir or another antiviral preoperatively,” says Dr. Afshari. “This would be in the range of 400 mg b.i.d. preop, because of the chance of recurrence. Though not every surgeon administers an antiviral for their cataract patients with a history of herpes, those that do usually start it a week or two before the surgery—though some start a month before. The timing is similar for preop penetrating keratoplasty patients. There really hasn’t been a clinical trial to let us know how soon to start. People just use the art of medicine.”
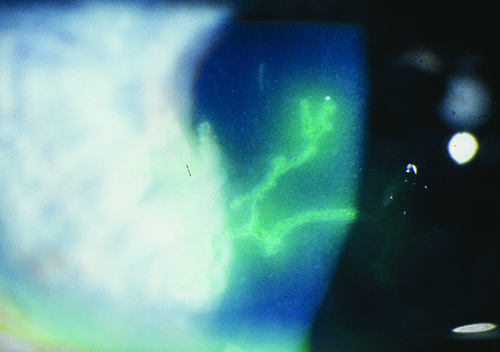 |
| Surgeons say the time elapsed since the last herpes flare-up and antiviral coverage are keys to minimizing complications after anterior segment surgery in herpes patients. (Image courtesy David Hardten, MD.) |
Dr. Balakrishnan also bases the antiviral regimen on the intended surgery. “I’d start three to seven days before the procedure with q.d. Valtrex (valacyclovir) 1 g p.o., q.d.,” she says. “If I’m a bit more concerned about the patient for some reason, I would use a therapeutic dose of t.i.d. maybe three days before, and continue that prophylactic dosing throughout their postop course. So, for a cataract patient, I’d keep them on prophylactic Valtrex for the entire time they’re on topical steroids.
“If the surgery is to be a corneal transplant, because of the risk of herpetic keratitis, I’d probably start the therapeutic Valtrex two or three days before the surgery and continue a 10-day course of it, eventually bringing them down to a preventative dose until I felt comfortable tapering them down to their usual dose of preventative or trying to taper them off of it entirely.” She says you can use a more aggressive regimen for patients who’ve had herpes flare-ups that had devastating visual consequences.
Dr. John describes his approach, which tries to balance the negative and positive effects of the steroids: “With cataract surgery, we use topical corticosteroids to decrease the postop inflammation, but we know steroid drops can contribute to HSV reactivation,” he notes. “So, you want antiviral coverage when you use topical steroids. To accomplish this,
The location and severity of the herpes outbreak also play a role when deciding on the drug regimen. “I think stromal/uveitic manifestations are red flags,” Dr. Balakrishnan says. “They require a more aggressive regimen. If the patient had a peripheral dendrite that’s resolved and has had nothing since, or just had conjunctivitis, to me that’s a little bit lower on the scale of worry, if you will. In those less-serious cases, I wouldn’t necessarily pursue an aggressive preventative regimen.”
Intraoperative Issues
Both the ephemeral threat of a recurrence and the concrete reality of a corneal scar cause surgeons to adjust their intraoperative approach.
“How to proceed intraoperatively depends on what type of herpes manifestation they’ve had,” Dr. Balakrishnan says. “Did they have uveitis? If so, I’d take precautions for the
“In terms of incisions, you want them to be nice and clean,” he continues. “One thing you want to consider is, if they’ve been uveitic in the past, you can’t do subconjunctival injections. However, you could consider intravitreal injections, if necessary, to prevent CME or a recurrence of a more profound uveitis after you’ve been inside the eye.
“Regarding scarring,” Dr. Balakrishnan adds, “
Postop Protocols
Most surgeons will keep the herpes patient on the antiviral medication during his postop
“For someone prone to more inflammation, such as a
“
Dr. Afshari notes there’s a difference between



