Spinal Pressure and POAG
Two studies conducted at the University of North Carolina, Duke University, the University of South Dakota and the Mayo Clinic are shedding new light on the association between cerebrospinal fluid pressure and primary open-angle glaucoma.
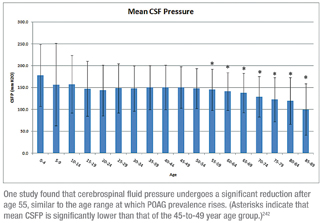 The first study examined the relationship between age and CSFP in a large database of patients who had a lumbar puncture performed at the Mayo Clinic (Rochester, Minn.) between 1996 and 2009. Researchers obtained demographic and clinical information including medical history, lumbar puncture opening pressure and CSF analysis. They compared three age groups; patients between the ages of 45 and 49 had a mean CSFP of 150.3 ±47.7 mmH2O; those between ages 80 and 84 had a mean CSFP of 119.7 ±53.7, a 20.4-percent reduction (p<0.001); those between ages 85 and 89 had a mean CSFP of 100.0 ±58.9, a 33.5-percent reduction from the youngest group (p<0.001). They found no difference between the sexes. (See chart, facing page.)
The first study examined the relationship between age and CSFP in a large database of patients who had a lumbar puncture performed at the Mayo Clinic (Rochester, Minn.) between 1996 and 2009. Researchers obtained demographic and clinical information including medical history, lumbar puncture opening pressure and CSF analysis. They compared three age groups; patients between the ages of 45 and 49 had a mean CSFP of 150.3 ±47.7 mmH2O; those between ages 80 and 84 had a mean CSFP of 119.7 ±53.7, a 20.4-percent reduction (p<0.001); those between ages 85 and 89 had a mean CSFP of 100.0 ±58.9, a 33.5-percent reduction from the youngest group (p<0.001). They found no difference between the sexes. (See chart, facing page.)
The authors conclude that CSFP undergoes a significant and sustained reduction after age 55, and note that the age range at which CSFP declines is similar to that at which the prevalence of POAG rises, supporting the hypothesis that reduced CSFP may be a risk factor for POAG.242
Noting that decreased body mass index is a possible risk factor for POAG, while low CSFP is also a possible risk factor for POAG and elevated CSFP may be protective, the second study sought to determine whether BMI and CSFP are related.
The data showed that at a BMI of 18, mean CSFP was 112.9 ±48.7 mmH2O. At a BMI of 21, there was a sustained, statistically significant increase in mean CSFP to 124.4 ±42.5 (p<0.05). At a BMI of 35, CSFP reaches 165.89 ±54.43; (p<0.0001). The increase in CSFP from a BMI of 18 to a BMI of 35 was 32.4 percent.
 The study authors note that this data suggest that as BMI increases, CSFP increases, which indirectly suggests that an elevated BMI may be protective because of a corresponding increase in CSFP. This is consistent with recent studies.244
The study authors note that this data suggest that as BMI increases, CSFP increases, which indirectly suggests that an elevated BMI may be protective because of a corresponding increase in CSFP. This is consistent with recent studies.244
Trabeculectomy
Two researchers at the University of Toronto conducted a retrospective chart review of 128 glaucoma patients (median age: 72) who had undergone a trabeculectomy between 2004 and 2006 to study how benzalkonium chloride exposure from eye drops im- pacted time to trabeculectomy failure. They recorded the number and type of ophthalmic drops used preoperatively along with relevant demographics. (Patients received between one and eight BAK-containing drops daily, with a median of three.)
 Patients receiving higher preoperative daily doses of BAK had a shorter time to surgical failure than patients who had less BAK exposure (p=0.008). Proportional hazard modeling identified uveitic and neovascular glaucoma as significant confounders of the univariate model (p=0.024), although the main effect of BAK exposure was maintained. The number of different medications used to control IOP did not significantly affect survival time (p=0.948).613
Patients receiving higher preoperative daily doses of BAK had a shorter time to surgical failure than patients who had less BAK exposure (p=0.008). Proportional hazard modeling identified uveitic and neovascular glaucoma as significant confounders of the univariate model (p=0.024), although the main effect of BAK exposure was maintained. The number of different medications used to control IOP did not significantly affect survival time (p=0.948).613
Researchers at two hospitals and a research center in Belgium and the Netherlands conducted a prospective, randomized, placebo-controlled, double-blinded study to investigate the effect of perioperative intracameral bevacizumab on clinical outcomes following trabeculectomy in patients with either POAG or normal tension glaucoma. One hundred thirty-four consecutive, medically uncontrolled patients scheduled for first-time trabeculectomy between April 2009 and November 2010 were included.
Patients were divided into POAG and NTG groups. Those were then randomized into two subgroups: one group received 50 µl bevacizumab (25 mg/ml); the other received placebo. (Patients with NTG also received mitomycin C.) By the end of November 2010, 87 patients had reached the six-month follow-up point; of this group, 45 received bevacizumab and 42 received placebo. The data showed:
- Absolute success was 85 percent in the bevacizumab group and 69 percent in the placebo group.
- Qualified success was 13 percent in the bevacizumab group and 21 percent in the placebo group.
- Failure occurred in 2 percent of the bevacizumab group and 10 percent of the placebo group.
- Needlings were performed in 7 percent of the bevacizumab group and 39 percent of the placebo group.
OCT: Seeing the Unseen
Researchers at Bascom Palmer Eye Institute in Miami and Carl Zeiss Meditec in Dublin, Calif., conducted a study (partially funded by Carl Zeiss Meditec) to determine how effectively ganglion cell-internal plexiform (GCIP) layer thickness, measured with Cirrus HD-OCT, can differentiate between normal and glaucomatous eyes. Fifty glaucoma patients and 95 age-matched normal subjects were included in the study.
One randomly selected eye in each patient was scanned using the Macular Cube 200x200 protocol. The study assessed the ability of each of the protocol’s parameters to discriminate between normal eyes and glaucomatous eyes irrespective of disease severity; between normal eyes and eyes with mild glaucoma; and between normal eyes and eyes with moderate to severe glaucoma. The performance of each parameter was assessed by reporting the area under receiver operating characteristics (AUC).
The data showed:
- The best discriminants between normal eyes and glaucomatous eyes irrespective of disease severity were: GCIP thickness of the infero-temporal sector (AUC=0.975); minimum GCIP thickness (0.961); GCIP thickness of the inferior sector (0.956); overall average GCIP thickness (0.937); and GCIP thickness of the supero-temporal sector (0.935).
- To differentiate normal eyes and those with mild glaucoma, GCIP thickness of the infero-temporal (AUC=0.976) sector was the best parameter, followed by GCIP thickness of the inferior sector (0.952), minimum GCIP thickness (0.948), and overall average GCIP thickness (0.916).
- All parameters had excellent ability to differentiate normal eyes from eyes with moderate to severe glaucoma (r: 0.916 to 0.975), except for GCIP thickness for the supero-nasal sector (0.851).185
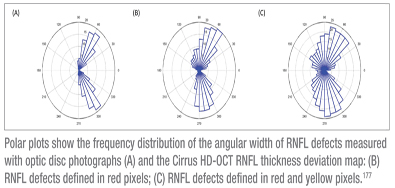
Thirty-nine localized RNFL defects were identified in 30 eyes of 22 glaucoma patients taken from a data-base of 259 color optic disc stereo-photographs. These patients then had RNFL imaging performed with spectral-domain OCT.
The area and angular width of RNFL defects measured with the optic disc photographs were 2.45 ±1.04 mm2 and 28.14 ±12.75 degrees, respectively. This was significantly smaller than those measured by the OCT RNFL thickness deviation map; when the defects were defined as thickness below the lower 95 percent normal distribution, area and angular width were 4.03 ±2.01mm2 and 75.91 ±45.57 degrees (both differences p<0.001).
Overall, the agreement between OCT and optic disc photograph measurements of RNFL defects was poor. Furthermore, larger defects were associated with greater differences between OCT and optic disc photograph measurements.
The authors conclude that analysis of the OCT RNFL thickness deviation map could reveal additional RNFL abnormalities not detectable in optic disc photographs.177
Managing IOP
Researchers at Kowa Co. Ltd, a Japanese pharmacology company, added to their growing research on the ocular hypotensive effect of K-115 ophthalmic solution (a rho-kinase inhibitor) with an animal-model study investigating the effect of K-115 on IOP, alone and in combination with latanoprost. The study also evaluated the ocular distribution of topically instilled K-115 and its expression in the eye. The data showed:
- In cynomolgus monkey eyes, significant IOP reduction (p<0.01) was produced by 0.1%, 0.2%, and 0.4% K-115 (11.7 ±1.2 percent, 16.6 ±1.4 percent, and 22 ±1.4 percent IOP reduction, respectively).
- In monkey eyes, IOP reduction in K-115/latanoprost treatment (28.9 ±1.5 percent) was significantly higher than the reduction produced by latanoprost treatment alone (16.1 ±0.9 percent, p<0.01).
- In Japanese white rabbits, K-115 had no effect on aqueous flow rate: 1.88 ±0.35 µL/min, compared to the pre-treatment 1.97 ±0.23 µL/min.
- Autoradiographic studies showed that topical instillation of K-115 penetrated into the anterior part of rabbit eyes, including the trabecular meshwork; immunohistochemical analysis revealed that ROCK-1 and -2 were co-expressed in the trabecular meshwork of both the rabbits and monkeys.
 The authors conclude that K-115 reduced IOP in a dose-dependent manner and showed a significant additive effect with latanoprost. In addition, results suggest that the effect of K-115 on IOP is due to the increment of aqueous humor outflow via trabecular meshwork route as a result of the inhibition of ROCKs.237
The authors conclude that K-115 reduced IOP in a dose-dependent manner and showed a significant additive effect with latanoprost. In addition, results suggest that the effect of K-115 on IOP is due to the increment of aqueous humor outflow via trabecular meshwork route as a result of the inhibition of ROCKs.237
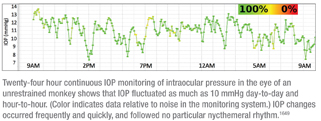
Researchers at Devers Eye Institute in Portland, Ore., adapted a proven implantable telemetric pressure transducer system to monitor IOP continuously in three awake, unrestrained non-human primates to characterize the dynamics of IOP over multiple time scales for multiple 24-hour periods. The implanted transmitter took 500 IOP, ECG and body temperature measurements per second. Data were statistically analyzed for a nycthemeral pattern.
IOP fluctuated as much as 10 mmHg day-to-day and hour-to-hour when measured continuously in these unrestrained, awake primates. (See graph, next page.) Ten-minute time window averaging for a 24-hour period showed that IOP fluctuated from 7 to 14 mmHg during the day, and those changes occurred frequently and quickly. Two-hour time window averages for multiple 24-hour periods in three animals found no particular nycthemeral rhythm.
The authors conclude that these findings agree with the most recent human studies on 24-hour IOP variation, and suggest that snapshot IOP measurements may be inadequate to capture IOP.1649
In response to two studies reporting that sildenafil (Viagra) caused no abnormalities in IOP or change in blood pressure—which contradicted their own earlier studies showing substantial IOP increases in sheep given sildenafil—researchers in New York City and Argentina conducted a study using human volunteers in Corrientes, Argentina, to corroborate the effects of sildenafil on human IOP and systolic blood pressure.
In the first group of nine subjects, IOP before sildenafil was 13.1 ±0.6 mmHg, which increased to 16.5 ±0.8 (p<0.01) 80 minutes later. IOP returned to control values (12.7 ±0.6) three hours later. Systolic BP was 118 ±4.3 and 97 ±4.1 before and 60 to 90 minutes after sildenafil respectively, a 21-mmHg decrease. Systolic BP was no different from control three hours later. In the group of five subjects, IOP significantly increased in those receiving sildenafil but not in those who took the placebo, with similar results for BP.
The authors conclude that sildenafil increased IOP and decreased BP on a time course consistent with its erectile effect. This type of vasodilator could increase IOP in senior patients.1525
Noting that various corticosteroid formulations for both ocular and non-ocular indications may produce elevation of intraocular pressure, researchers at the University of Virginia and the University of Tennessee conducted a prospective study to see what percentage of a group of glaucoma patients were using corticosteroids—perhaps without the knowledge of the doctor treating their glaucoma. (The study authors note that the use of corticosteroids for differing indications may not be identified in glaucoma patients unless specifically solicited.)
Physician examiners in a tertiary referral glaucoma clinic queried 100 patients using a detailed questionnaire requiring documentation of corticosteroid use. (Topical corticosteroids used short-term postoperatively were not included as exposure.)
They found that 53 percent of these patients had been treated with at least one type of corticosteroid modality. This included 29 percent, oral systemic use; 28 percent, local injections; 10 percent, topically (dermatological use); 4 percent, respiratory inhalers, 4 percent, topical ophthalmic drops; and 1 percent, nasal sprays. Seventeen percent documented use of more than one formulation at some time.
The authors note that a targeted history is helpful for identifying various formulations and indications for corticosteroid use in these patients.5047
Researchers at the University of Iceland and Oculus Inc., in Reykjavik, Iceland, have developed a new dorzolamide eye-drop formulation, containing self-assembled drug/cyclodextrin microparticles and hydroxypropylmethylcellulose, that enhances and prolongs drug delivery to the eye. They conducted an in vivo study using rabbits to evaluate drug distribution of a 3% suspension in the eye. Testing showed that the maximum dorzolamide concentration in aqueous humor after topical administration of the 3% formulation was 5.4 ±3.6 µg/ml at tmax of four and two hours; the concentration of commercially available 2% dorzolamide eye-drop solution (Trusopt) was 2.2 ±1.5 µg/ml at tmax of four and two hours (p<0.05). Also, the eye-drop suspension provided sustained high dorzolamide concentrations for up to 24 hours, while the Trusopt dorzolamide concentration in aqueous humor was essentially zero eight hours after its administration.
The authors note that this formulation could be developed into a once-a-day eye drop, potentially leading to improved patient compliance.235
Protecting the Ocular Surface
Researchers at three hospitals in Shanghai, China, conducted an animal-model study to determine whether vitamin A palmitate can protect the ocular surface from damages induced by prolonged use of topical antiglaucomatous eye drops. Sixty eyes of 30 New Zealand white rabbits were randomized to one of five treatment groups: vitamin A palmitate 1% QD (group 1); timolol maleate 0.5% b.i.d. (group 2); brimonidine 0.2% b.i.d. (group 3); vitamin A palmitate 1% q.d. combined with timolol maleate 0.5% b.i.d. (group 4); or vitamin A 1% q.d. combined with brimonidine 0.2% b.i.d. (group 5), for 30 days.
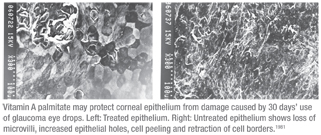
At the end of the 30 days, rabbits in groups 2 and 3 showed significantly fewer normal tear breakup times and basal Schirmer’s tests than before (p<0.05). Also, conjunctival impression cytology showed that the global score in the epithelium in groups 2 and 3 was significantly lower than before (p<0.05). Corneal damage in groups 2 and 3 assessed with scanning electron microscopy showed loss of microvilli, increasing number of epithelial holes, cell peeling, loss of hexagonal shape and retraction of cell borders. (See images, facing page.) The ocular surface did not seem to change obviously in group 1, 4 and 5.
The authors conclude that the long-term use of glaucoma medications combined with vitamin A might help preserve ocular health.1981
Drainage Devices
Ophthalmologists at multiple eye centers and universities in the United States and Canada have released the most recent, two-year results of the Ahmed versus Baerveldt (AVB) Study, comparing the two most frequently implanted aqueous drainage devices. In the study, 238 patients at least 18 years old with uncontrolled glaucoma refractory to medical, laser and surgical therapy were recruited from seven international sites.
Eligible patients were randomized to receive either an Ahmed-FP7 valve (n=124) or a Baerveldt-350 implant (n=114) using standardized surgical technique. At two years:
- Mean IOP was 16.1 ±6.4 mmHg in the AGV group and 14.5 ±6.6 mmHg in the BGI group (p=0.12).
- Mean number of glaucoma medications required was 1.8 ±1.4 in the AGV group and 1.0 ±1.2 in the BGI group (p<0.001).
- Complications occurred in 61 AGV patients (49 percent) and 69 BGI patients (61 percent) (p=0.08).
- Treatments were required in 40 AGV patients (32 percent) and 54 BGI patients (47 percent) (p=0.02).
- The cumulative probability of failure was 48 in the AGV group and 31 percent in the BGI group (p=0.02).
Researchers at the University of Pittsburgh Medical Center conducted a study to see whether a new technique for glaucoma drainage device surgery using 25-ga. microsurgical forceps and fibrin glue could achieve faster surgical time and lower costs than standard methods. They reviewed 24 videos of glaucoma drainage device surgery; 16 used standard toothless Hoskins forceps to insert the glaucoma drainage device tube; eight used 25-ga. microsurgical forceps (DORC). Also, 22 of the surgeries performed conjunctival closure using fibrin glue; two used sutures.
The average total time for surgery using 25-ga. microsurgical forceps was 16 ±4.8 minutes; using standard forceps the total time was 22.4 ±8.0 minutes. Using 25-ga. microsurgical forceps shortened total case time by 28.3 percent (p=0.032). Average time for insertion of the tube using 25-ga. microsurgical forceps was 0.6 ±0.3 minutes; using standard forceps it was 3.2 ±2.3 minutes. Using 25-ga. forceps shortened the time of tube insertion by 80.1 percent (p=0.002).2641
Visual Fields and Imaging
Researchers at the University of Michigan conducted a study to determine whether the location of visual field loss at diagnosis is associated with progression in VF loss over time. They inspected baseline Humphrey 24-2 full threshold VF tests of 607 subjects with newly diagnosed open-angle glaucoma, taken from the Collaborative Initial Glaucoma Treatment Study, to determine the location of VF loss.
The data showed that of all locations and combinations that were evaluated, paracentral VF loss at baseline was consistently most predictive of subsequent VF loss. Every one-unit increase in paracentral loss was associated with a decrease in mean deviation (MD) of 1.7dB (p<0.0001). Also, VF loss in several peripheral regions was found to be associated with moderate improvement or less worsening of MD, although this may have resulted from artifactual change in the baseline VF tests.
The authors conclude that assessing the location of VF loss at diagnosis could help determine how aggressively a patient should be treated.5027
Researchers in two hospitals in São Paulo, Brazil, conducted a study to investigate the effect of age, gender, and time of day on standard automated perimetry reliability indices, among 344 glaucoma patients and glaucoma suspects with no perimetry experience.
Logistic regression showed a significant association between time of testing and the occurrence of an unreliable visual field. Subjects tested before 9:00 a.m. and after 4:00 p.m. had worse reliability indices (β=0.8060, p=0.03). Fixation loss was the most common reliability problem, and the data showed a statistically significant relationship between fixation loss in the right eye and time of testing; fixation loss was more frequent at the beginning and end of the day (p=0.03). The data also showed a significant association between fixation loss and age in both eyes.5522
Researchers in four countries pooled confocal scanning laser ophthalmoscopy data from the CSLO ancillary study to the Ocular Hypertension Treatment Study and the European Glaucoma Prevention Study, in an attempt to improve ophthalmologists’ ability to predict the development of POAG in ocular hypertensive subjects. They included data from 222 subjects with good quality Heidelberg Retina Tomograph images from the observation group of the CSLO Ancillary Study and 229 subjects from the EGPS placebo group. Twenty-seven of the OHTS subjects and 31 of the EGPS subjects developed POAG; median time to POAG was 3.9 years.
In multivariable models:
- Larger baseline rim area (HR: 0.68 per 0.2 mm2), rim volume (HR: 0.73 per 0.1 mm3), and RNFL thickness (HR: 0.57 per 0.1 mm) significantly decreased the probability of developing POAG.
- Larger baseline cup area (HR: 1.8 per 0.3 mm2), cup volume (1.2 per 0.1 mm3) and cup/disc area ratio (HR: 1.5 per 0.1 mm), and baseline outside normal limits results for Moorfields Regression Analysis (HR: 2.3) and Glaucoma Probability Score (HR: 2.0) significantly increased the probability of developing POAG.
- The predictive ability of baseline HRT rim and cup area were similar to that of models that include stereo-photo-based cup/disc ratio.
Ethnicity and Glaucoma
Researchers at three American universities conducted an observational cohort study to evaluate and compare rates of progressive visual field loss in a cohort of African descent (AD) and European descent (ED) patients diagnosed with glaucoma or suspected of having the disease. (The study was supported in part by Alcon, Allergan, Pfizer and Merck.) The study included 895 eyes of 520 patients (222 AD and 298 ED) with glaucoma, or suspected of disease, recruited from the Diagnostic Innovations in Glaucoma Study and the African Descent and Glaucoma Study.
The data showed no significant difference between mean rates of visual field progression in AD and ED eyes (-0.06dB/year vs. -0.04dB/year; p=0.626). However, the AD group had a significantly higher proportion of eyes with fast progression; the 5th quantile of rates of change in AD eyes was -0.62dB/year, compared to -0.35dB/year in ED eyes (p<0.001). For the 1st quantile, the corresponding numbers were -1.33dB/year vs. -0.65dB/year (p=0.021). Differences between the two racial groups remained significant after adjustment for age, baseline disease severity, mean IOP during follow-up and central corneal thickness. Similar results were obtained when rates of VFI change were analyzed.
The authors note that this data suggests that the AD population may be at significantly higher risk for development of functional impairment from glaucoma.2117
Researchers at Stanford University and the University of California conducted a prospective study to identify glaucoma patients at particularly high risk for poor disease outcomes in a county hospital population at the San Francisco General Hospital. They recruited 152 individuals with established glaucoma, creating one-to-one match-ups of subjects with poor follow-up and subjects with good follow-up (controls). Oral questionnaires were used to collect data regarding ethnicity and barriers to follow-up.
The data showed:
- Individuals of Latino ethnicity with limited English proficiency and those of black race with a family history of glaucoma were at greatest risk for poor follow-up and noncompliance with medications (adjusted OR 8.38, 95% CI 3.39 to 12.31; and 7.21, 95% CI 2.16 to 15.47, respectively).
- The most prevalent reasons reported for noncompliance with medications were a subjective perception of stable vision between follow-up exams without adverse symptoms (62 percent); unfamiliarity with treatment duration (39 percent); and the permanency of glaucomatous vision loss (32 percent).
- Notably, travel time to clinic and cost of medications were not significantly associated with follow-up patterns and medication compliance.
Researchers at the University of Michigan surveyed data from 149,018 individuals age 40 or older with open-angle glaucoma who were enrolled in a large U.S. managed-care network from 2001 to 2009 to determine whe-ther racial and sex disparities existed in the use of diagnostic procedures.
The surveyed group included 15,905 blacks, 118,062 whites, 9,376 Latinos and 4,350 Asian Americans. At the end of the covered period, in 2009, the probability of receiving imaging was highest in black males (54 percent) and black females (54 percent) and lowest in Latino males (41 percent) and Latino females (41 percent). The authors note that Latinos are the fastest growing racial minority, so efforts need to be made to better understand why they’re receiving less OAG monitoring than other ethnic groups.5316
Dr. Netland is a professor and chairman of the department of ophthalmology at the University of Virginia; Dr. Singh is a professor of ophthalmology and director of the Glaucoma Service at Stanford University School of Medicine.