Imaging the Drainage System
A fundamental characteristic of ultrasound technology is that the frequency of the sound largely determines both the depth the signal is capable of reaching and the resolution of the resulting image; higher frequencies don't penetrate as deeply into tissue, but they do produce higher-resolution images. Thus, a 2-MHz probe can be used to produce low-res images of internal organs such as the liver; a 10-MHz probe can image the back of the eye; and a 50-MHz probe can produce fine images of tissues at the front of the eye. Use of the highest frequencies constitutes ultrasound biomicroscopy (UBM).
Until recently, commercial ultrasound probes have only offered frequencies up to 50 MHz. But now iScience Interventional (Menlo Park, Calif.), a medical device company focused on the development and commercialization of micro-catheter and imaging systems for ophthalmic surgery, has developed a new ultrasound system, the iUltrasound, that uses a frequency of approximately 80 MHz.
Stan Levy, director of imaging development at iScience, explains that the driving force behind the new instrument was the need for an imaging tool that could help surgeons visualize Schlemm's canal in conjunction with canaloplasty, a new glaucoma treatment procedure. During canaloplasty, a microcatheter (the iTRACK, also available from iScience) is used to produce 360-degree viscodilation of Schlemm's canal; a 10-0 polypropylene suture is attached to the microcatheter and drawn into the dilated canal as the catheter is removed. The suture is then appropriately tensioned, facilitating a significant and sustained reduction in intraocular pressure.
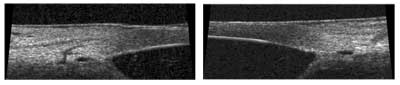
The new 80 MHz ultrasound system from iScience produces very high-resolution images of the eye's outflow system, and can be used in the OR under sterile conditions. Left: Anterior angle of Schlemm's canal and connectors. Right: Secondary angle closure of Schlemm's canal.
"Our goal at iScience is the development of new therapies to treat site-specific ocular disease in the anterior and posterior segments of the eye," says Mr. Levy. "As we worked with canaloplasty, it became clear that the 50-MHz systems simply can't image some of these fine structures—particularly Schlemm's canal and finer details of the trabecular meshwork. So, we created the iUltrasound, a high-resolution imaging system that's optimized for imaging the upper 2 mm of the anterior segment of the eye, where the drainage elements are located. The frequency is nominally centered at 80 MHz, providing axial resolution of 25 µm. Also, the iUltrasound captures seven frames per second, which is enough speed to eliminate motion artifacts caused by hand movements."
Mr. Levy says that another unique design element of the new instrument is that it can be used in a sterile-field environment. "Until now, ultrasound systems have been more oriented to office use," he says. "We found we needed an instrument that could assess the impact of an interventional procedure such as canaloplasty in real time, enabling the surgeon to respond appropriately during the procedure."
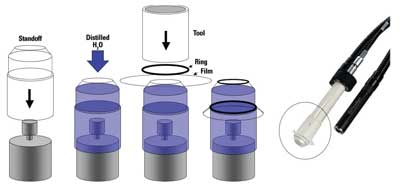
To accomplish this, iScience developed a sterile imaging cap for the instrument, allowing the interface between patient and instrument to remain uncontaminated. "This is a single-use, disposable cap designed and packaged for use in the sterile field," explains Mr. Levy. "We also provide a sterile, disposable sheath which extends over the non-sterile portions of the imaging probe and back onto the cable."
Mr. Levy says that the company's future focus is on continued development of microcatheter-based therapies such as canaloplasty. For that reason, the iUltraSound will be positioned as an enabling technology, rather than a general diagnostic instrument. "Our initial focus with the iUltraSound will be on high-resolution anterior segment work, of most interest to anterior segment ophthalmologists who are looking at disease related to the outflow system of the eye," he says. "However, we view this instrument as a platform that can be adapted to other frequencies and applications, and we are confident those will come in time."
Fine-tuning Glaucoma Diagnosis
Richard A. Lewis, MD, a cataract surgeon and glaucoma specialist practicing in Sacramento, Calif., and past president of the American Glaucoma Society, has worked with iScience on this project for the past three years. "Some ultrasounds measure corneal thickness or IOLs or certain tumors," he notes, "but there's never been one that focused on glaucoma, specifically looking at the outflow system. Because of this instrument's high resolution, it can produce incredibly clear images of parts of the eye that up to now we couldn't see, such as the canal of Schlemm; you can also use it as a gonioscopic tool to diagnose angle closure glaucoma. Plus, it can be used during surgery, and it's portable, easy to use and easy to train others to use."
Dr. Lewis says that it's possible to perform canaloplasty without the ultrasound instrument. However, he notes that it's very helpful to know exactly where the canal is and to be able to see how much tension you're putting on the suture, especially when you're learning the technique.
Dr. Lewis believes the new instrument is a potential breakthrough for the study of glaucoma. "The whole theory of glaucoma has centered around a problem with outflow based on data from the 1960s," he points out. "However, no one's been able to look at the canal in vivo. The whole process of glaucoma has been very generalized; we define it as open-angle or closed-angle. The fact is, in this century we should be able to do a better job of defining it. Is it a problem in the trabecular meshwork? Is it a problem in the canal? Is it a problem in the outflow system? This instrument is the first step in that process. Hopefully, we can come up with a more modern, sophisticated, site-specific diagnosis of glaucoma. Also, it would be great to do long-term studies. What happens to the outflow system from your mid teens to your seventh or eighth decade? Now we have the tool to do the work."
Mr. Levy says iScience hopes to have a version of the iUltrasound on the market within the next few months and plans to make a presentation about it at the American Academy of Ophthalmology meeting in November.
Enclosing a High-Frequency Probe
As ultrasound has become more popular, the inconvenience of using a water bath has become more of an issue for clinicians. Manufacturers have responded by offering the option of self-contained probes. However, this is widely seen as a trade-off, especially when used in conjunction with high-frequency UBM, because it requires placing some sort of membrane between the probe and the eye, which can affect image quality.
Barry Durante, executive vice president of Sonomed, in Lake Success, N.Y., says that Sonomed's Vumax system, which functions both as a standard B-scan and a high-frequency system, comes with the option of a self-contained probe. (He notes that most of Sonomed's lower-frequency probes—less affected by adding the membrane—are now self-contained.)
Mr. Durante believes the trade-off is primarily for the benefit of the user. "The technician or doctor has one hand holding the scleral shell and the other hand holding the probe," he notes. "If you have to make an adjustment to the unit, both hands are busy. That means you need someone else to make adjustments for you, or a multifunction footpedal. In contrast, if you use a self-contained probe, you have one hand to hold the probe and the other hand free to make adjustments.
Paradigm's high-frequency P60 UBM includes the option of a self-contained probe. Placing self-contained probes directly against the eye seems to compensate for the interference caused by the extra membrane.
"However, it is a trade-off," he continues. "If you have nothing between the probe and the eye except fluid, you get exceptionally good resolution and image quality. Putting a membrane between the transducer and the object of interest usually undermines that quality. Plus, the sound waves pass through it twice—once to get to the object, and once coming back. And since higher frequencies don't penetrate as far, UBM quality is more affected than low-frequency scans.
"So, if you want to use a self-contained UBM probe, you have to select your materials very carefully or you'll lose too much of the ultrasound energy. We're currently looking for materials that can be used to enclose the high-frequency probe without any deterioration of the image, and we're testing possibilities. Other companies have come out with alternatives, but the proof of the pudding is in the image. If you have an image that's as good as with the water bath, then you have something. Right now, there's room for improvement."
Mr. Durante says Sonomed would like to have something new along these lines for the Academy meeting in November, but can't say for sure whether they'll be ready by then. "We want to be user-friendly," he says, but it's a compromise. We prefer to err on the side of image quality."
Richard Weitz, president of Ophthalmic Technologies, Toronto, says that OTI does offer an enclosure for its UBM probe, but doesn't list the option on its website. "An enclosed probe has several disadvantages, primarily that the membrane absorbs sound," he notes. "Also, the membrane must fit nicely around the cornea or limbal interface. If the technician has to fill the enclosure, you can get bubbles or leakage. And an inexperienced person can scratch the cornea. In fact, I wouldn't sell this probe tip to an inexperienced person." He notes that OTI is working on finding a material for the membrane that absorbs less sound than water, but so far, that goal remains elusive.
Directly on the Eye
Mike Austin, vice president of sales and marketing at Paradigm Medical Industries in Salt Lake City, says that Paradigm's high-frequency P60 UBM, which includes the option of a self-contained probe, produces great anterior images in spite of the membrane—as long as the probe is placed directly against the eye, not the eyelid. "We're using the same film we've always used," he says. "It's durable, but it's very thin. In the scans you can see the membrane, but we've had no complaints because the doctors know what it is. They expect it. And the anterior images are great.
"One good thing about the contained probe is that it's comfortable for the patient," he continues, "assuming that you use a non-stinging gel. Of course, if you could get a strong enough probe to work through the eyelid, it would be even more comfortable for the patient, but I've seen this done directly on the eye on a number of patients and no one has complained at all. In contrast, the water bath can be very uncomfortable." Asked if it's a problem that the film starts out flat while the eye is round, he says the probe produces excellent images, even on small eyes.
Mr. Levy at iScience Surgical says the new iUltrasound UBM probe is self-contained and the membrane does not cause a problem. "We had to find a material that had acceptable acoustic properties, was biocompatible and had reasonable physical properties in terms of strength, and we did," he says. "Also, the fact that it's disposable means we can use a very thin membrane, which helps—it doesn't have to have a long life in terms of mechanical durability." Like the Paradigm probe, it's intended to be placed directly on the eye.
Mr. Levy admits that the risk of corneal abrasion is always conceivable. "However, with our thorough testing and evaluation, plus the input we've gathered from ophthalmologists, we feel confident in our product's safety and performance" he says. "The cap design is supplemented with the use of a viscous lubricating fluid during eye contact to ensure patient safety and comfort. Our studies haven't found anyone with any noticeable abrasions or discomfort."



