The Hyperopic Presbyope
Ottawa surgeon W. Bruce Jackson, one of the investigators in Visx's Canadian multifocal ablation study for hyperopic presbyopes, explains how the ablation is designed.
 |
"This uses Visx's patented ablation that produces a central zone for near vision, with the periphery of the cornea being for distance," he says. "The near zone is pupil-dependent, and it's around 3 mm. The ablation for the distance portion goes out to 9 mm. So, it's like a standard hyperopic treatment, but the central near zone is anywhere between 3 and 3.5 mm, depending on the pupil size." He says the "sweet spot" of the procedure is +2 to +2.5 D, though they've treated as much as +3.5 D of sphere, and up to +1.5 D of cylinder.
The Visx study of hyperopic presbyopic ablations now has 82 eyes of 49 patients, with 46 of them having one year of follow-up. Average preop error was +1.88 D, and average cylinder was 0.43 D.
Using binocular vision, all the patients with one year of follow-up can see 20/25 at distance and J3 (the size of newspaper stock quotes).
One of the issues multifocal treatments have had to deal with is contrast sensitivity and loss of lines of vision. "The contrast sensitivity does drop early on," says Dr. Jackson. "But, by 12 months, it has almost returned to the preop value."
As for how the patients respond to the treatment, Dr. Jackson says they're happy. At one year, 80 percent say they're very satisfied with the sharpness and clarity of their vision without glasses, compared to 77 percent who said so preop with their glasses.
When asked about their distance vision in bright light, which could be an issue because the pupil is small then, he says 92 percent are happy with their vision without their glasses. Seventy-eight percent are satisfied with their uncorrected night vision postop, compared to 68 percent who were satisfied with their night vision with spectacles preop.
"Where we did notice a little drop was their near vision in bright light without their glasses," says Dr. Jackson. "In those conditions, they're not as happy as they were with their glasses preop." He thinks this is partly because, over time, they've lost some of their near vision.
"That's the thing we have to work on," he says. This could be from hyperopic treatment's tendency to regress over time." The researchers weren't allowed to make any nomogram adjustments to address this in the study, however.
"You're looking at regression of effect like you get with hyperopic treatments in general," says Dr. Jackson. "At one month they were overcorrected by -0.23. At 12 months they were at +0.14 , so they changed about 0.33 D over time. So ending up slightly on the positive side does have an effect on their near vision."
The Myopic Presbyope
In Bogotá, Colombia, Gustavo Tamayo, MD, is investigating the Visx laser for the other side of the presbyopic coin, the myope.
In this treatment design, the peripheral zone, which starts at the 5.5-mm zone and goes out to 9 mm, is for near vision. The center is used for distance. Dr. Tamayo is testing the procedure in myopic presbyopes as well as pure presbyopes without a spherical error.
Dr. Tamayo has followed 34 myopic-presbyopic eyes for an average of 26 months. The average preop error was -2.58 D with -1.25 D of cylinder. These patients were done with wavefront-guided treatments.
Preop, without their correction in place, most of the patients read between J1 and J3, because, as myopes, many could take their glasses off to read. But with their correction, all were J8 or worse. After the procedure, 70 percent of the myopia group read J1 and all were J3, without correction. And 70 percent were 20/25 or better for distance. All the myopes could see at least 20/30 and J3.
 |
All of the patients lost some contrast sensitivity, at least initially. "But, after three months, 93 percent returned to the previous contrast sensitivity levels," says Dr. Tamayo. "In fact, I think we are facing the same problems with these ablations as we have with the multifocal intraocular lenses we're using today. That is, they have to lose a little contrast sensitivity visual acuity, but, little by little, most go back to normal."
The results vary in different light conditions. "The far distance vision improves with bright light," says Dr. Tamayo. "In a few patients, for the first month or two, I prescribe miotic agents for use at night so they see better at distance as they get used to the multifocal ablation. The near vision gets worse in dim light."
There was a 15-percent enhancement rate, 6 to improve near vision and 9 for distance vision. "At two months, if we see that the patient is still myopic and the vision isn't 20/25 or better, we'll do an enhancement," says Dr. Tamayo.
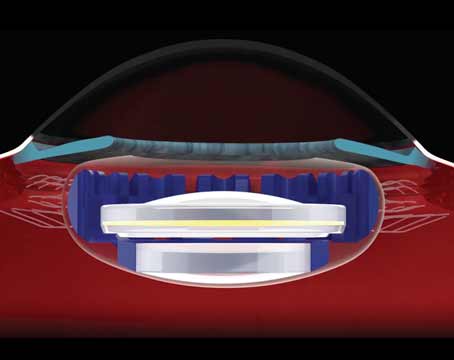
The surgeons think that multifocal ablations will have a place in a world where multifocal intraocular lenses are gaining popularity.
"If you asked, 'What is the best treatment for presbyopia today?' I think we're looking at the multifocal IOLs," says Dr. Jackson. "But there is a group of patients in their mid to late 40s with some accommodation left who don't want an intraocular procedure; for them a multifocal ablation would be the way this group would rather go if they wanted fairly good reading and good distance vision …. I don't think this will have any effect on getting a multifocal IOL later on, because the amount of treatment in the multifocal ablation is small."
"The main concern with any type of corneal ablation has been the future calculation of an IOL if the patient develops cataract eventually," says Dr. Tamayo. "But I think with new biometric devices for IOL calculation, problems of power calculation will be solved in the near future."
Some surgeons, though, think it would be tremendously complicated to get a good IOL calculation in these multifocal ablation patients, and point out that it's unknown whether a multifocal IOL will be compatible with a multifocal cornea. They also doubt a surgeon could easily get rid of the multifocal effect in the cornea to the extent that you could erase it.
Future studies will no doubt aim to address these issues.