Surgeons’ views on new technology are just one aspect of the survey, and respondents also shared their opinions on cataract surgical techniques, as well. This month’s e-mail survey was opened by 902 of the 8,500 subscribers to Review’s e-mail service (an open rate of 11 percent) and, of those, 91 completed the survey. See how your go-to cataract techniques and maneuvers compare with theirs.
Going Easy on Innovation
The survey touched on several new modalities in the cataract realm, including femto cataract and intraoperative pupil dilation injection (Omidria). Though it’s only been a year since surgeons weighed in on a couple of these innovations, their enthusiasm for them seems to have leveled off a bit.
• Femtosecond cataract. In last year’s cataract surgery survey, 31 percent of surgeons said they used the femtosecond laser for at least one aspect of cataract surgery. This year, that number has held steady at 32 percent. The most popular use for the femtosecond during cataract was in correcting astigmatism, chosen by all of the femto-cataract surgeons. Next came the creation of the capsulotomy and nucleus fragmentation, chosen by 97 percent each. Fifty-seven percent also use the laser for the entry wound and 43 percent for the paracentesis. “Despite being very proud of my nearly perfect capsulorhexes done with the Utrata forceps by hand, no human alive can reproduce the precision and accuracy of placement and reproducibility of the femto!” enthuses Robert P. Lehmann, MD, of Nacogdoches, Texas.
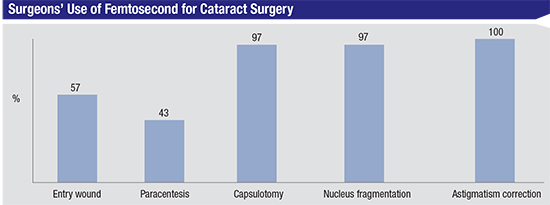 |
A surgeon from Nevada says the femto offers a “consistent rhexis, and it can correct small amounts of astigmatism for patients getting multifocal IOLs.” He adds, however, that it’s “expensive, adds additional time to the case, and the cortex is more difficult to remove.” A Texas surgeon thinks the positives outweigh the negatives, however. “It adds time, but it seems to give better results.” And an ophthalmologist from Maryland has also had a good experience with the technology. “It’s gentler and more accurate,” he says. “It also allows flexibility when customizing it, and is safer in some situations.”
Looking down the road a bit, three-quarters of the respondents who don’t use the femtosecond in cataract surgery say they’re unlikely to start using it within a year. A lot of their reservations about the lasers center on the perceived cost/benefit ratio.
“It involves an unnecessary increase in the cost of the procedure compared to standard phaco,” says Peter Libre, MD, of Norwalk, Conn. “Yet, I perceive no net improvement in the quality of the procedure.” A surgeon from California feels similarly, and is also concerned about having to relearn something that she already does well. “Femtosecond cataract seems as if it’s too costly for such minor advantages,” she says. “Also, I don’t want to go through a difficult learning curve when I’m already happy with my current procedure.”
One physician is among the quarter of respondents who are looking forward to using the femtosecond. “It’s an excellent technology for astigmatism and capsulorhexis,” he says. Richard Wieder, MD, of St. Louis says it’s only a matter of time before he takes the plunge. “I have not used femtosecond laser yet,” he says, “but I’m planning to later this year.”
• Intraoperative aberrometry. Even fewer of the survey respondents (15 percent) use this technology than use femtosecond cataract devices. Sixty-eight percent of the surgeons who don’t use it say they’re not likely to do so in the coming year. Cost and added surgical time are often cited as the main roadblocks. “The advantage is that it provides an intraoperative estimation of the IOL power and astigmatism axis,” says Robert Bullington Jr., MD, of Phoenix. “The disadvantages are that it adds time and expense and doesn’t give a definitive answer.” A Texas physician agrees about the pros and cons involved with using the technology. “It helps with the confirmation of difficult IOL calculations,” he says. “However, you can’t always trust the cylinder adjustment assessments. It also takes time, sometimes requiring multiple attempts at capture.”
Some surgeons, however, think it’s been a good addition to their practices. “Poor patient fixation can be an issue,” avers a surgeon from Florida. “However, it’s very helpful with toric IOLs, post-refractive surgery patients, high hyperopes and high myopes.”
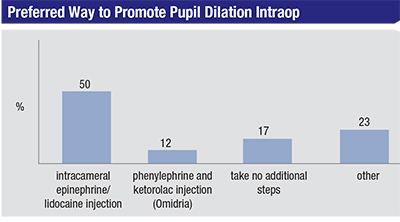
• Pupil dilation strategies. Surgeons say a well-dilated pupil is one of the keys to smooth surgeries and good outcomes, and many are interested to see where the new intraoperative agent from Omeros, Omidria (an injection of phenylephrine and ketorolac), might fit in their practices. On the survey, half of the surgeons use an intracameral injection of a mixture of BSS, epinephrine and lidocaine (the so-called “epi-Shugarcaine” first proposed by the late surgeon Joel Shugar); 17 percent don’t take any extra steps to promote a wide pupil, 12 percent use Omidria and 23 percent say they use some other method to ensure dilation, such as iris hooks or Malyugin rings. “Shugarcaine is adequate for most patients,” says Glenn Sanford, MD, of Washington, Mo. “I manage floppy irises with the Malyugin ring.” Luther Fry, MD, of Garden City, Kan., has begun using Omidria, and likes his results. “Omidria works well in preventing intraoperative miosis—it has markedly reduced my use of the Malyugin ring,” he says. “I don’t use it for adequate pupils, though.”
• Postop inflammation/infection management. Surgeons also weighed in on the new approach to postop management that involves replacing a postop drop regimen with a single postop injection of a combined antibiotic/steroid, such as the TriMoxiVanc combination sold by Imprimis. Though some surgeons see the benefit of this, drops still rule the survey, with 92 percent of surgeons choosing them over the injection. Six percent of surgeons administer the injection and the rest use another method. “I gave the intravitreal 0.2 cc of TriMoxiVanc a trial in over 140 cases and stopped,” recounts Dr. Lehmann. “Now, I will go with either prescription drops or the compounded triple drops. The rising cost of prescriptions is making it hard for many patients—but I won’t get into a discussion of politics right now.” Another surgeon from Texas is sticking with the injections. “The savings are huge with TriMoxi injection, both for the system and for the patient,” he says. “The acceptance by the patient is easy. The biggest hurdle to adoption is surgeons’ fear of the unfamiliar.”
Managing Astigmatism
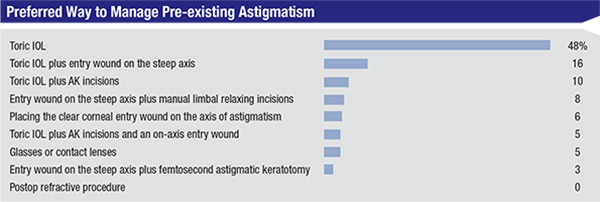
When surgeons approach a patient’s pre-existing astigmatism, the toric IOL remains the single most popular option, chosen by 48 percent of the respondents. The next most popular choice is to combine the toric lens with the placement of the entry wound on the astigmatic axis (16 percent), followed by the toric lens combined with AK incisions (10 percent). The rest of the surgeons’ options appear on the graph on p. 40.
 |
Dr. Lehmann chooses to combine the toric lens with AK incisions, but says he’s flexible based on the patient presentation. “I implant a huge percentage of toric IOLs,” he says. “Yet, I also use femto corneal relaxing incisions. For the non-premium patients I will do limbal relaxing incisions with a blade at no additional cost. It’s always best to put the patient’s outcome over all else.”
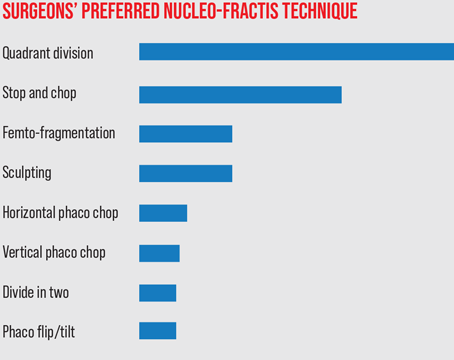
Phaco Techniques
Attacking the nucleus is where the rubber meets the road in the cataract procedure, and 52 percent of surgeons surveyed say they prefer to use a quadrant-division approach. Following quadrant division, 16 percent prefer stop-and-chop, and 15 percent prefer a phaco-chop technique. Phaco flip/tilt, sculpting and dividing the nucleus in two were each chosen by less than 10 percent of the respondents.
Florida’s Dr. Ten Hulzen is in the quadrant-division camp. “I’m a comprehensive ophthalmologist and glaucoma subspecialist,” he says. “I have a lot of patients with pseudoexfoliation, dense cataracts, poorly dilating pupils/IFIS, retinal pathology from AMD and/or diabetes. Maintaining posterior capsular integrity is paramount in these patients as well as in the premium (toric and multifocal) IOL patients. Therefore, I minimize any stress on the capsular bag and zonules. I groove and use a nucleus splitter to achieve a clean split while maintaining equal-and-opposite forces within the capsular bag.” A surgeon from New York also says he likes quadrant division because it keeps him in control. “It gives me full control of the procedure,” he says. “There’s no blind instrument passing.”
Jeffrey Lander, MD, of York, Pa., prefers stop-and-chop. “It’s safe and controlled,” he says. “Much of the phaco is done away from cornea.” Robert B. Taylor III, MD, of Las Vegas agrees, saying, “It’s simple, efficient and works in most types of lens densities.”
A surgeon from Florida, however, says phaco chop is preferable to the other methods. “It’s safer and uses less energy,” he says. “It also offers faster postop recovery.” Phoenix’s Dr. Bullington also prefers it. “In my hands,” he says, “it’s the most efficient technique for emulsifying the lens with minimal phaco time.”
Surgical Pearls
With many decades of combined experience under their belts, the survey’s respondents were happy to share their best surgical pearls.
In terms of discrete techniques, several surgeons offer ideas. Carol Johnston, MD, of Jacksonville, N.C., says, “Preop pledgets and the use of bridal sutures in eyes with difficult exposure are helpful.” Dr. Pode advises: “If you think you may need a Malyugin Ring for a difficult case, always put it in. You’ll never be upset that you used the device. It’ll make your surgery easier, quicker and safer.” A surgeon from Texas says to sweat the small stuff. “Each step builds on the one before it,” he says. “So even things like positioning the patient are of utmost importance.” Dr. Wieder focuses on astigmatism with his advice. “Utilize multiple different testing modalities to manage preoperative astigmatism,” he says. “This will provide the most predictable results postop.”
 |
Several surgeons emphasized the importance of getting things done correctly rather than getting things done quickly. “Don’t hurry,” says a surgeon who preferred to remain anonymous. “Take the time to prevent complications.” Dr. Colombo feels similarly. The clock stops in the OR,” he says. “Work carefully and never rush—no wasted steps. Keep calm.”A surgeon from Massachusetts highlights the importance of preop checks. “Just as there is an in-the-room pre-surgical checklist with lens verification and a time-out, a preop checklist for every patient is useful,” he says. “Make a list of the things that you want to know before surgery and look out for any outliers and plan ahead. For example, you’ll obviously note things like pseudoexfoliation or poor dilation, but note also the white-to-white distance and AC depth. If there are asymmetries, they can direct you toward other steps that can be taken to prevent complications. There are times I have said I wish I had used Trypan Blue or iris hooks, but there’s never been a time when I used them and wished I hadn’t.”
Finally, a surgeon from Texas says that, above all else, make sure you keep your surgical options open. “Always have a plan B available for your technique,” he says. “Be flexible about approaching each case differently. If all you have is a hammer, everything looks like a nail.” REVIEW