If you're an ophthalmologist who dispenses contact lenses, you know how difficult it can be to get patients to comply with proper lens care, and to educate them about what to do, and not to do, with their lenses. Pending legislation, however, threatens to cross over from the realm of convenient contact lens purchasing into that of corneal health, and may make your job as a "learned intermediary" more difficult. In this month's column, we'll discuss the role the learned intermediary plays with regard to the ocular health and safety of contact lens wearers, and will consider the potential implications of the current contact lens bill.
The Intermediary's Role
As we all know, contact lenses are not risk-free: They are medical devices requiring proper patient screening, education and follow-up, and can induce complications with results as severe as vision loss. This potential outcome alone makes it clear that interaction with a professional before, during and after contact lens use is crucial. The learned intermediary properly screens patients, selects appropriate lenses, monitors the ocular health of the patient and continues to respond to his changing needs.
In screening patients, the intermediary needs to assess any preexisting conditions to determine any risks that would contraindicate contact lens use. These risks may include dry eye, allergic conjunctivitis, blepharitis, recurrent infections, anterior membrane dystrophy, neovascularization, marginal infiltrate or giant papillary conjunctivitis.
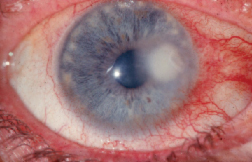 |
| Continuous monitoring of contact lens wearers' corneal health by a learned intermediary can help avoid the development of corneal ulcers such as this. |
In selecting lenses, the dispensing physician matches patients to lenses. Each individual patient has specific ocular characteristics and needs (i.e., wearing schedule, base curve, lens polymer type), and, as time goes by, these patient characteristics can change, thus changing the patient's contact lens needs.
Instruction on proper use, as well as appropriate duration and situations of wear for the specific lenses, are also crucial pieces of information provided to the patient by the intermediary. Lastly, continued monitoring of each contact lens wearing patient's ocular health is necessary to avoid any potentially sight-threatening complications or the development of any conditions that would preclude lens wear. This involves monitoring patients' ability to maintain adequate compliance, hygiene and insertion and removal techniques.
Recent studies have shown that poorly fitted lenses can lead to corneal abrasions or serious infections.1 Other studies have been reported to the U.S. Food and Drug Administration stating that patient non-compliance with proper contact lens maintenance procedures is a significant source of corneal ulcers. Giant papillary conjunctivitis, microbial keratitis and infections can also stem from improper adherence to lens cleaning and replacement procedures. If left undiagnosed, ulcers or other complications can lead to infection and corneal scarring. If not appropriately addressed, severe ulcer cases can lead to blindness or enucleation.
Despite the apparently important role of the learned intermediary in maintaining contact lens wearers' corneal health, federal legislation has recently been proposed that would decrease his involvement in the process of purchasing lenses. The goal of the legislation is to help patients save money. The bill is called the "Fairness to Contact Lens Consumers Act."
The Bill's Ramifications
The contact-lens bill was introduced to the U.S. House of Representatives' Committee on Energy and Commerce, and it covers many of the issues that have arisen due to increasing sales by third-party contact lens vendors. Two of the main issues that the bill covers, and that directly affect the physician who prescribes lenses, are the dispensing and verification of contact lens prescriptions. Though many state laws currently mandate that the doctor give the patient a copy of his prescription to take with him, this bill would make it a nationwide requirement. It would also require the seller of the contact lenses to contact the patient's doctor directly to verify:
• the patient's name and address;
• the lens's manufacturer, base curve, power and diameter;
• the quantity of lenses ordered;
• the dates of the patient's request and verification of the request;
• the name and phone number of a contact at the seller's company.
The bill is in response to recent controversy surrounding third-party companies selling contact lenses to consumers without verifying their prescriptions. These companies are generally volume discounters, offering patients a variety of contact lenses that may be at lower cost and are primarily chosen by patients for convenience. On the surface, this movement toward discounters seems to be a positive economic trend, as it increases competition in the contact- lens market. Also, since contact lenses can be expensive, patients could save a significant amount of money by acquiring them through third-party vendors.
The supporters of this bill have argued that it will parallel the 1978 act that mandated the release of spectacle prescriptions to patients. The proponents point out that this 1978 law brought a significant growth of alternative eyeglass providers over the past 25 years and that increased competition brought higher quality products and lower prices. Economic consultants and government organizations such as the Federal Trade Commission have predicted the same kind of growth in the contact lens industry and have put their support behind the bill.
What may be getting lost in the move toward third-party contact lens vendors is the understanding that contact lenses aren't the same as spectacles. Contact lenses are medical devices that require the lens fitter's expertise to properly match a patient with a lens and his guidance to help the patient avoid potentially serious complications.
Many concerned eye-care professionals see the lens bill as an effort to cut out the role of a learned intermediary, significantly reducing the ability of the dispensing ophthalmologist's ability to maintain the lens wearer's ocular health. Unfortunately, the convenience and savings on the lenses often entice patients to overlook the potential health risks. This type of law, in the long run, could have a negative impact on both ophthalmology and contact-lens manufacturers if patients are allowed to wear these products at their own risk until a problem reaches a severe stage.
• How sharp are the vendors? A recent study examined the top five mail order and Internet companies based in the United States that dispense contact lenses. The researchers contracted an independent company specializing in product investigations to organize purchase of lenses from third-party vendors, which currently comprise 90 percent of the mail-order and Internet industry for contact lensese2 Even though the buyers in the study attempted to use these vendors to purchase lenses using invalid prescriptions, lenses were dispensed for 90 percent of the prescriptions for most products, indicating a flaw in prescription verification procedures.
The study also examined the lens prescription verification processes of several different contact lens manufacturers, and revealed inadequate procedures in almost all cases. The one company that was the exception was Vistakon, whose verification procedures weeded out all but 8 percent of invalid or expired prescriptions, showing an exceptional control over the distribution of their lenses. Third-party companies followed Vistakon's prescription verification process more often. Verification primarily via fax, rather than automated phone calls, helped. Overall, however, the study showed a disturbing trend among the mail-order contact lens companies that suggested that, in most cases, a valid prescription isn't necessary in order to obtain lenses. Unfortunately, there's no legislation currently in place to ensure proper verification of lens prescriptions. The hope of the pending legislation is to enforce regulations on manufacturers and distributors to make them mimic Vistakon's policies regarding the sale and dispensation of their contact lenses.
• A loophole. Even if thorough requirements for the verification of prescriptions were strictly enforced, however, the integrity of the process may be compromised by a single clause within the bill. It states that if a "prescriber fails to communicate with the seller within eight business hours after the seller achieves direct communication,"3 the prescription in question is considered valid and may be filled.
The ambiguity of this statement leaves a hole in the verification process, the crux of this bill in terms of patient safety. Essentially, the burden of responsibility would be placed on the shoulders of the manufacturers and the distributors to make a genuine effort to verify prescriptions. Unlike the process a physician goes through in his office when he starts a patient on contact lenses, there would be no initial instruction regarding how long lenses should be worn, under which conditions they should or shouldn't be worn and the warning signs of contact-lens related ocular diseases.
Relevant to the issues of compliance and avoiding complications is the increasing prevalence of extended-wear contact lenses, which can lead to an increased susceptibility to infectious keratitis secondary to corneal hypoxia1 and corneal ulcers generally attributable to patient non-compliance.4 Studies have revealed that patient compliance with proper contact-lens care may be as low as 20 percent,5 and this could possibly drop lower if the physician is cut out of the picture.
It's unclear how the issues around mail-order contact lenses are going to be resolved. This is not the first bill of its kind to approach the legislature, and many of its predecessors made no definitive progress. It will be interesting to see what happens in the coming year. Beyond that, the issues surrounding compliance with proper contact lens wear will continue to be a challenge for eye-care professionals. How should doctors deal with the powerlessness of a situation in which patients get a prescription for a device then disappear out the door? How can you maintain a relationship with patients who rely on a third-party vendor for their contact lenses?
Until any laws actually pass, the unregulated sale of contact lenses will continue to allow people access to medical devices without valid prescriptions. However, even if the current proposed legislation makes it through Congress, the "passive verification" loophole doesn't ensure that prescriptions will be verified. In the end, the detailed ocular exams and diagnoses that a learned intermediary has the ability to make aren't things that the patient can determine on his own or by calling an 800 number. Eye disease is part of the human condition, not something that can be legislated.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Mr. Schindelar is a research associate at Ophthalmic Research Associates in North Andover.
1. Brennan NA, Coles ML. Extended wear in perspective. Optom Vis Sci 1997;74:8:609-23.
2. Teague R, Arima FM, Briggs J, et al. Finding the right prescription for mail-order sales. Contact Lens Spectrum 2003; 18;9:Pgs: 36-40.
3. H.R. 3130 108th Congress, 1st session
4. Smith SK. Patient noncompliance with wearing and replacement schedules of disposable contact lenses. J Am Optom Assoc 1996;67:3:160-4.
5. Ky W, Scherick K, Stenson S. Clinical survey of lens care in contact lens patients. CLAO J 1998;24:4:216-219.



