Statement of Need:
Selective Laser Trabeculoplasty is a new technology being introduced into the clinical practice of ophthalmology. Selective laser trabeculoplasty has several potential advantages over argon laser trabeculoplasty. Initial studies suggest a similar efficacy with initial treatment as seen with argon laser trabeculoplasty. SLT intraocular pressure reduction is comparable to what glaucoma medications provide either as adjunctive or primary therapy. Prospective studies are under way to clinically evaluate the role of SLT in the management of open angle glaucoma. Ophthalmologists need to understand the fundamentals of this technology in order to better understand its applications in clinical practice.
Learning Objectives:
1. Explain the concept of SLT including the various mechanisms by which it is thought to affect intraocular pressure.
2. Describe how SLT compares with medication and other existing surgical options for IOP reduction.
3. Review the clinical applications and limitations of SLT.
Estimated Time to Complete the Activity: 1 hour
Faculty/Editorial Board: L. Jay Katz, MD
Accreditation Statement: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of Postgraduate Institute for Medicine and Review of Ophthalmology. The Postgraduate Institute for Medicine is accredited by the ACCME to provide continuing medical education for physicians and takes responsibility for the content, quality, and scientific integrity of this CME activity.
Designation Statement: The Postgraduate Institute for Medicine designates this educational activity for a maximum of one (1) hour in category 1 credit toward the AMA Physician's Recognition Award. Each physician should claim only those hours of credit that he/she actually spent in the activity.
Disclosure Statement: Dr. Katz has disclosed that he has received grant/research support from Lumenis Inc., and is a member of the company's speakers bureau.
Postgraduate Institute for Medicine has a conflict of interest policy that requires course faculty to disclose any real or apparent commercial financial affiliations related to the content of their presentations/materials. It is not assumed that these financial interests or affiliations will have an adverse impact on faculty presentations; they are simply noted here to fully inform participants.
Disclaimer: Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient's conditions and possible contraindications on dangers in use, review of any applicable manufacturer's product information, and comparison with recommendations of other authorities.
Disclosure of Unlabeled Use
This educational activity contains discussion of published and/or investigational uses of agents that are not indicated by FDA. The Postgraduate Institute for Medicine and Review of Ophthalmology do not recommend the use of any agent outside of the labeled indications. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications and warnings.
Selective Laser Trabeculoplasty was introduced by Boston surgeon Mark Latina, MD, in 1995 specifically as treatment for the reduction of intraocular pressure in open-angle glaucoma patients. This advancement and departure from prior laser technologies offers improvements in patient comfort, laser mechanics and laser-tissue interaction, while maintaining the desired pressure reduction seen in other methodologies. This article will discuss the technical and clinical aspects of SLT and how it fits into the glaucoma armamentarium. Please note answer sheets are at the bottom of this page; scroll down to use/view.
Background
Although argon laser trabeculoplasty and SLT are similar in that they both utilize laser technology to treat the trabecular meshwork in order to increase outflow, their design and function differ greatly.
The argon laser, as well as the diode laser, were directed at the trabecular meshwork to photocoagulate and stretch the meshwork, thereby increasing outflow.1 After a period of four to six weeks following treatment, the IOP would drop due to an increase in trabecular outflow of aqueous.
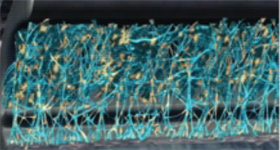 |
| Figure 1. Selective Laser Trabeculoplasty therapy targets the pigmented, melanin-containing cells (yellow), while preventing thermal transfer to the surrounding tissue. |
A number of studies have examined the role of ALT in the therapy of open-angle glaucoma. ALT has been placed in different parts of the treatment paradigm in a number of National Eye Institute-sponsored multicenter trials: the Glaucoma Laser Trial (GLT); the Advanced Glaucoma Intervention Study (AGIS); the Collaborative Initial Glaucoma Treatment Study(CIGTS); and the Early Manifest Glaucoma Trial (EMGT).
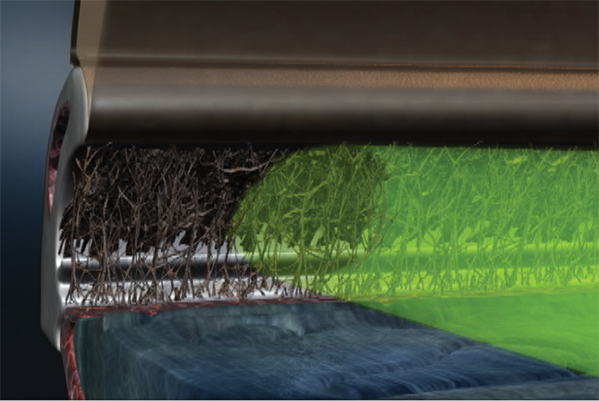
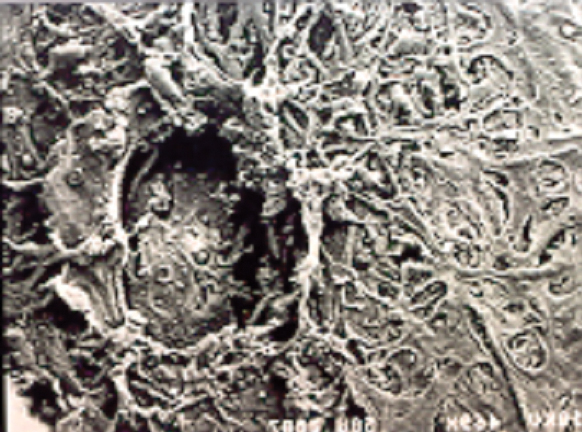 |
| Figure 2. Thermal injury resulting in coagulative damage to the trabecular architecture can be seen using scanning electron microscopy. In time, this would result in scarring in live tissue.3 |
How SLT Works
Selective laser trabeculoplasty was further developed by Coherent Medical (now Lumenis) with work done by Dr. Latina. In 1995 SLT was introduced worldwide, and it was cleared by the Food and Drug Administration in March 2001. The key concept in the design of this laser system was to direct the energy towards only pigment-containing cells in the trabecular meshwork.
Investigations began based on previous studies with ALT in which a strong correlation was found between IOP reduction and the amount of pigmentation in the angle. Patients with characteristically heavy angle pigmentation, pigmentary glaucoma and exfoliation syndrome demonstrated the most favorable response to ALT.
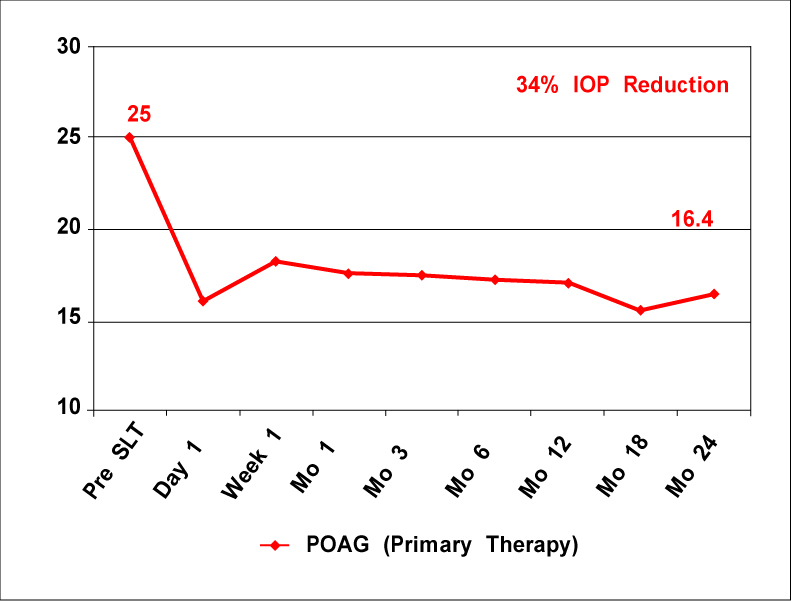 |
| Three-year data illustrating the prolonged effects of Selective Laser Trabeculoplasty when used on a maximum-meds population (n=36 for SLT and 39 for ALT).7 |
Starting in the laboratory setting with in vitro cultures of trabecular meshwork cells, pigmented and non-pigmented, various laser wavelengths were tested for their ability to selectively target pigment-laden cells. The frequency doubled 532-nm Nd:YAG laser was found to be an appropriate wavelength for injuring the pigmented cells while sparing the non-pigmented cells and the surrounding architecture.
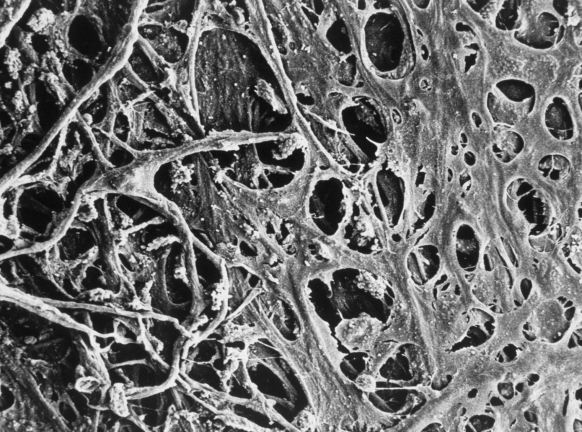 |
| Figure 3. No thermal or coagulative effects are noted using Selective Laser Trabeculoplasty.3 |
If applied to the angle structures, SLT would selectively target the pigmented cells and not cause any collateral thermal injury. In vivo animal eye studies confirmed the nonthermal property of SLT contrasted to the thermal melting of the trabecular meshwork beams using an argon laser.2 Further studies were performed on cadaver eyes, illustrating the non-thermal properties of SLT.3
Finally, living patients were tested to investigate the pressure-lowering properties of SLT.5 The importance of this non-thermal property may be connected to the lack of repeatability with the ALT. If repeated applications of ALT are delivered in a normal primate eye, experimental secondary open-angle glaucoma is created.
With the SLT, repeated applications may potentially lower the IOP in eyes where the IOP has drifted back up to pretreatment levels without altering the structural integrity of the outflow system.
Interestingly, the mechanism by which laser treatment to the human angle results in IOP lowering is still not clearly established. Three mechanisms have been proposed: mechanical; cellular; and biochemical. These explanations are not mutually exclusive and may even be complementary.
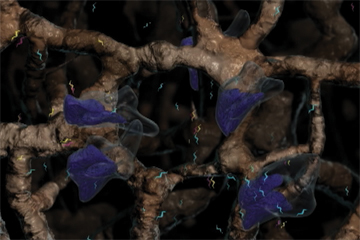 |
| Figure 4. Studies by Jorge Alvarado, MD, suggest the recruitment of macrophages (large, blue) that remove cellular debris and extracellular melanin from the meshwork. Macrophages stimulate the release of cytokines (small, blue/yellow) which induce cell division; upregulate synthetic metalloproteinases; increase the porosity of the endothelial layers of the trabecular meshwork and Schlemm's canal; and stimulate resynthesis of the extracellular matrix. |
The mechanical theory proposes that a thermal burn contracts tissue and stretches open adjacent, untreated regions of the meshwork to increase outflow. Since SLT does not cause this thermal injury, this first theory may only apply to ALT. The cellular model suggests that laser application stimulates the replication of trabecular endothelial cells that normally do not divide. The last hypothesis pinpoints the release of biochemical mediators (cytokines) and macrophage recruitment into the laser treatment zone as instrumental in the reduction of IOP.
The commercially available SLT lasers are the Selecta II and Selecta Duet made by Lumenis, Inc. The lasers have been clinically used worldwide since 1997, receiving FDA clearance in the United States in early 2001. The laser pulse duration is fixed at 3 nanoseconds. The spot size is fixed at 400 µm, which encompasses the entire meshwork from Schwalbe's line to the ciliary body band. The laser energy is uniformly distributed to evenly treat the meshwork. Fifty confluent applications over 180 degrees or 100 per 360 degrees are typically delivered in a sitting.
 |
| Figure 5. Approximately 100 confluent spots are applied during the procedure in order to treat the entire angle. |
Since transient IOP spikes may occur in some patients, a topical alpha-agonist may be given before and after the laser session. If, despite that prophylaxis, the IOP still spikes then other glaucoma medications are given until the IOP falls back to pretreatment levels or lower.
The use of topical steroids or nonsteroidal anti-inflammatory agents post-laser is controversial. Some argue that the mild inflammation that attracts macrophages into the treatment area is important for the therapeutic response, and therefore anti-inflammatory drugs should be avoided. Conversely, one to two days of anti-inflammatory use has not been shown to jeopardize the outcome of SLT and certainly helps keep patients from developing symptomatic uveitis.
The time course for IOP reduction following SLT has been highly variable, but a significant response is seen at postop day one. Most clinicians wait at least four to six weeks before deciding whether the treatment had been beneficial; in some patients the response may occur even later.
In the initial published studies, SLT was used as adjunctive therapy to medical treatment. In a large case series, Dr. Latina noted an average IOP reduction of 6 mmHg with SLT.5 In another trial in Korea, researchers achieved a mean IOP reduction with SLT of 20 percent below baseline pretreatment levels.6
In a prospective, randomized clinical trial that compared ALT and SLT, the two-year year data shows equivalent 5- to 6-mmHg reduction in both groups.6 From this same population, three-year follow-up data has been presented confirming equivalent long-term results with ALT and SLT.
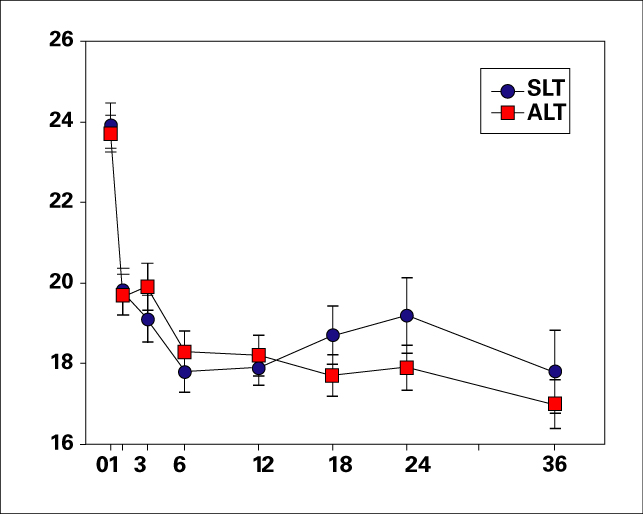 |
| Three-year data illustrating the prolonged effects of Selective Laser Trabeculoplasty when used on a maximum-meds population (n=36 for SLT and 39 for ALT).7 |
An intriguing question has been whether eyes failing ALT could have a favorable response to SLT. In a limited number of patients in several of the series the preliminary answer suggests that SLT may provide a meaningful IOP reduction in eyes unresponsive to ALT.
Primary Therapy?
An important conceptual challenge to our current approach to the management of open-angle glaucoma is to position SLT as primary monotherapy instead of medical therapy.
There are several serious concerns with medical therapy for a chronic, asymptomatic (early-moderate stages) condition such as open-angle glaucoma. Side effects with drugs, whether ocular or systemic, range from bothersome to serious. Compliance with medical therapy is a significant concern that has been detailed through questionnaires and electronic monitoring in glaucoma patients. Clearly, using the fewest medications with the simplest regimen that is free of side effects offers the best chance of adherence to the prescribed medical therapy. Appropriately, quality-of-life issues are being measured to assess different treatment approaches in comparative studies.
The increasing cost of medical therapy has an impact on patients and society as a whole. Going directly to filtering surgery has been one approach in studies in the United Kingdom and, more recently, in the United States as a part of the Collaborative Initial Glaucoma Treatment Study (CIGTS). However, the concern over intraoperative and postoperative complications has tempered any thoughts about this approach in clinical practice.
The Glaucoma Laser Trial (GLT) utilized ALT as first-line treatment compared with medical treatment.8 The 271 patients had their eyes randomized so that one eye underwent ALT first and the contralateral eye was given medical therapy. Barring criticisms, the GLT asked an important question regarding the placement and use of laser therapy in the sequence of glaucoma management.
Small case series in Europe and Israel, presented at this year's International Glaucoma Society meeting have applied SLT as an initial therapy for open-angle glaucoma with an IOP reduction from 22 to 34 percent below pretreatment levels. Considered in the context of similar IOP lowering with topical prostaglandin analogues and beta blockers, the usual first line choices for glaucoma therapy, SLT may be a viable first line choice in certain patients.8
It is known that there are non-responders to SLT, as there are with medical therapy. Research has shown that up to 34 percent of patients do not respond to medical therapy depending on the type of medication and time of day.
New Study Launched
A clinical trial is under way in the United States and Canada that will compare SLT with current medical therapy as primary therapy. Called SLT/MED, the study is a multicenter, prospective, randomized and controlled study designed to investigate SLT as initial treatment for open-angle glaucoma compared with topical medical therapy. The study is sponsored and funded by Lumenis Inc. and is being coordinated through Wills Eye Hospital in Philadelphia and Tulane University Center for Clinical Effectiveness and Prevention in New Orleans, La.
Outcome measures include: IOP reduction, quality of life assessment, cost analysis, perimetry and optic nerve/nerve fiber layer analysis. Another important issue to be evaluated is the response to repeat SLT treatment if there is an inadequate response or if there is a waning effect from the initial SLT treatment.
Since SLT offers the chance of significant pressure reduction without the thermal injury to the angle structures and the theoretical promise of repeat application being helpful, there has been increasing worldwide clinical acceptance of SLT. Further clinical and laboratory investigations are underway, and are important to validate the role proposed for SLT in the treatment of open-angle glaucoma.
To appreciate the application of SLT in an ophthalmic practice, see the Case History included as reference, illustrating the author's clinical use of the Selecta laser systems.
Dr. Katz is co-director of the Glaucoma Service at Wills Eye Hospital/Thomas Jefferson Medical School.
1. Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma: A pilot study. Arch Ophthalmol 1979;197:319-22 Exam: Vision 20/20 OU Points to consider:
2. Latina MA, Park C. Selective targeting of trabecular meshwork cells: In vitro studies of pulsed and CW laser interactions. Exp Eye Res 1995;60:359-372.
3. Noecker RJ, Kramer TR. Comparison of the acute morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology 2001;108(4):773-9.
5. Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G. Q-switched 532-nm Nd:YAG laser trabeculoplasty (Selective Laser Trabeculoplasty). Ophthalmology 1998;105:2082-2090
6. Kim YC, Moon CS. One-year follow-up of laser trabeculoplasty using Q-switched Nd:YAG laser of 532nm wavelength. Ophthalmic Surg and Lasers 2000 Sept-Oct;31(5):394-96.
7.Damji KF, Bovell AM, Hodge WG. Selective Laser Trabeculoplasty: A Review and Comparison to Argon Laser Trabeculoplasty. Ophthalmic Practice 2003;21:54-58
8. Glaucoma Laser Trial Research Group. The Glaucoma Laser Trial, II: Results of argon laser trabeculoplasty versus topical medicines. Ophthalmology 1990;97:1403-1413
9. Noecker RS, Dirks MS, Choplin NT, Bernstein P, Batoosingh AL, Whitcup SM. A six-month randomized clinical trial comparing the intraocular pressure-lowering efficacy of bimatoprost and latanoprost in patients with ocular hypertension or glaucoma. AJO 2003;135:55-63.
Case History
A 70-year-old woman with primary open-angle glaucoma has been treated for two years. The highest recorded intraocular pressure was OD 32 mmHg and OS 30 mmHg. She had been placed on latanoprost, brimonidine and dorzolamide without an apparent effect. The patient hinted that taking medications was difficult to remember especially those used more than once a day. She has been using timolol 0.5% each morning in both eyes. Past medical history is notable for recent onset of intermittent lightheadedness.
Tonometry: OD 25 mmHg OS 23 mmHg
Gonioscopy: open (D30r OU Spaeth classification) with 2+ moderate
pigmentation
Fundus: inferior notch in optic disc OU
Perimetry: small nasal step OU
Resting Pulse = 42
Patient was asked to stop timolol OU and underwent SLT OD and then OS two months later.
The lightheadedness disappeared and the IOP has been stable at 17-18 mmHg OD and 18-20 mmHg OS. Optic nerve appearance and perimetry remains unchanged for two years.
• Non-compliance with medication.
• Sustained, marked IOP reduction after SLT.
• Alternative choice to medication in certain patients.
• Side effect concerns with medication past two weeks OS.



