What the Data Says
Thousands of SMILE procedures have been performed internationally, and SMILE surgeons have gotten a handle on its predictability and effectiveness. The procedure is currently approved outside of the United States for corrections up to -10 D with up to 5 D of astigmatism.
In SMILE, the surgeon programs the Carl Zeiss Meditec Visumax femtosecond laser to create an intrastromal lenticule, the thickness of which varies based on the amount of correction he wants to achieve. The laser then creates a peripheral corneal incision of 2.5 to 3 mm. The surgeon uses special SMILE forceps to go through the incision and remove the lenticule.
Amsterdam’s Jesper Hjortdal, MD, and his team have performed 2,500 SMILE procedures, and Dr. Hjortdal discussed their results at the 2013 meeting of the American Academy of Ophthalmology. With SMILE, 95 percent of his patients (average preop error of -7.2 D) were within ±1 D of the intended correction and 80 percent were within ±0.5 D. In a paper covering the safety and complications of 1,800 SMILE eyes with a preop refraction of -7.25 D, Dr. Hjortdal reports that at three months 86 percent had unchanged or improved best-corrected vision, with 1.5 percent (27 eyes) losing two or more lines.1 The average postop refraction was -0.28 ±0.52 D, with a mean treatment error of -0.15 ±0.5 D. By 18 months, however, BCVA was within one line of its preop level in all eyes. Intraoperative complications included:
• epithelial abrasions in 108 eyes (6 percent);
• small tears at the incision site in 32 eyes (1.8 percent);
• difficult lenticule extraction in 34 eyes (1.9 percent);
• perforated cap in four eyes (0.2 percent) with no visual symptoms; and
• a major cap tear in one eye (0.05 percent) without visual symptoms.
|
Postop complications included:
• trace haze in 144 patients (8 percent);
• day-one epithelial dryness in 90 patients (5 percent);
• interface inflammation secondary to corneal abrasion in five eyes (0.3 percent); and
• minor interface infiltrates in five eyes (0.3 percent).
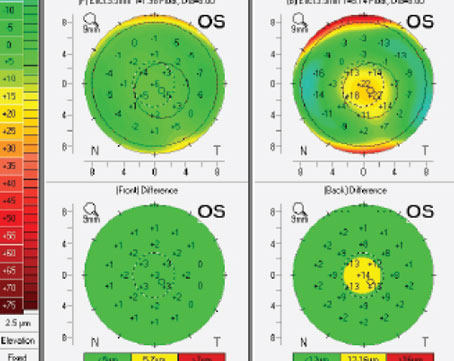
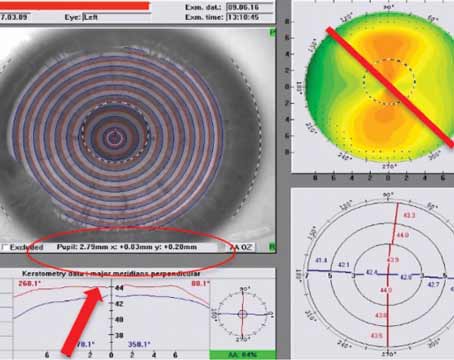
The postop complications affected best-corrected vision at three months in only one case. The researchers add that in 18 eyes (1 percent) the treatment resulted in irregularities on topography that reduced vision at three months (12 eyes) or induced ghost images (six eyes). In the latter, surgeons performed topo-guided PRK in four of the eyes, which improved the vision in three. Two patients expressed dissatisfaction at the latest follow-up due to blurred vision or residual astigmatism, while the rest were satisfied.
The Pros and Cons
After accumulating experience with thousands of SMILE procedures, surgeons say some pros and cons are emerging:
• Precision, and the absence of flap issues. Dr. Hjortdal found that the procedure is more precise for certain levels of myopia than LASIK has been in his hands. “Since the cutting of the lenticule is being done in an intact cornea, I think the precision of SMILE is better than that of LASIK for moderate and high myopia,” he says. “The other advantage is you don’t have a full flap, but instead a small opening. Secondary to this you have, in theory, a more stable cornea afterward. Minor trauma to the cornea months or even years later may have less of a tendency to dislocate the anterior lamellae. You may also have less tendency to develop ectasia. Since the sensitivity of the cornea is less affected after SMILE than it is in LASIK, dry eye may be less.” To this point, Singapore ophthalmologist Jod Mehta says he can always pick up a difference in the tear film between LASIK and SMILE eyes in a contralateral eye study he’s currently engaged in. “It’s an obvious sign that you can see,” he says. “And when you ask the patients—who are masked as to what treatment is in which eye—they almost always tell you that if they have to put drops in, it’s in the eye that turns out to be the one that had LASIK.” Dr. Mehta’s LASIK vs. SMILE study is still ongoing.
On the flipside, however, there are some aspects of the SMILE procedure that could pose more difficulties than in LASIK. “I think suction loss is the surgeon’s biggest fear when doing this procedure,” says Dr. Mehta. “You can’t stop and restart after the movement because the device is actually cutting the cornea, as opposed to ablating it—there are cutting planes that need to line up. Last year, though, Zeiss changed some of the laser programming and decreased the procedure time from 35 to 25 seconds, so patients don’t have to stay still under the laser as long as they had to before.
“Our suction loss rate was about 3.2 percent in the first 340 cases we studied,” Dr. Mehta continues. “However, if you handle suction loss correctly the patients do very well. Eighty-two percent of the suction-loss patients were able to finish their procedure on that day with a successful outcome. Two of them had to be converted to LASIK, one to LASEK.”
To help avoid suction loss from patient movement, Vadodara, India’s Rupal Shah, MD, says she tries to keep the patient calm. “It’s important to keep the patient steady, as the laser will be operating for 20 to 25 seconds,” she says. “To keep the patient from being anxious, so he can focus, keep reassuring him with such phrases as, “Very little time left now.”
• Low myopia/working with the lenticule. Paradoxically, some surgeons have reported anecdotally that, while LASIK is easier in lower levels of myopia, SMILE may get more difficult since the lenticule is thinner and more challenging to manipulate with forceps. Dr. Mehta, however, says it’s not the manipulation that’s difficult in low myopia, it’s finding the proper tissue to manipulate. “When we teach surgeons SMILE, we start with higher myopes as patients,” he says. “They are usually between -5 and -9 D. This is because the lenticule is thicker in these patients. But when you’re doing a lower-level treatment, such as -3 D as in one of our groups in our current study, the difference isn’t in the thickness in the lenticule because the edge of any SMILE lenticule is always 15 µm. Instead, it’s the center thickness of the lenticule that differs between low and high myopia. So, in a -1 myope the center might be 15 µm thick, but in a -9 patient it would be around 100 µm. It’s easier to see the center thickness in the higher myopes. It’s just the identification of the edge, and the edges above and below the lenticule, that the surgeon must be able to do. With more experience, you are able to identify the edges a lot more easily.”
Dr. Hjortdal says SMILE can also involve some variation in the quality of the lenticule cut, causing issues in about 0.5 percent or less of patients. “This is probably related to the early stage the SMILE technique is in, but there can be a little variation in the completeness of the femtosecond laser cut,” he says. “This means that sometimes you may have a slightly difficult lenticule removal and you might induce traces of hazy tissue in the interface. This may result in day-one acuity not being as good after SMILE when compared to LASIK, and you can run into problems related to the completeness of lenticule removal and smoothness. Specifically, you may have a little scar-like tissue in the interface that results from you having to be more aggressive in breaking these small tissue bridges.
“However, even though we’ve experienced such problems in some of our 1,800 eyes, when we have a second look at the patients in whom we noted significant problems during surgery, their condition seems to improve with time,” Dr. Hjortdal adds. So, this doesn’t end up in a situation of poor vision for the patients.”
• Early vs. late postop vision. Surgeons who have done both LASIK and SMILE say they’ve noticed a difference in the procedures’ patterns of visual recovery. “At least in the beginning, we felt there was a difference between LASIK and this type of surgery in terms of the uncorrected visual acuity on day one being a little lower with SMILE than what we’ve seen with LASIK,” says Dr. Hjortdal. “However, it would improve during the first week. Today, though, I think this has improved, due to the experience of the surgeons and the adjustments we’ve made to the laser algorithm.”
Dr. Mehta has noted some differences too, but in favor of SMILE. “Often LASIK patients get immediately good vision to start and then, over the first year, they get a slight deterioration in vision,” he says. “But with SMILE, they get good vision and then it seems to get better over that first year.”
• Retreatments. Surgeons have been grappling with the question of the best way to perform a retreatment on a previous SMILE patient since the procedure was introduced. “I don’t think surgeons completely agree on how to perform retreatments,” says Dr. Hjortdal. “If you want to adjust a diopter or so, it’s probably not wise to do a new SMILE surgery, because you’d need to do that SMILE in a layer of cornea where you wouldn’t interfere with the first cut. So, you’d have to go deeper or more superficial. Many surgeons—myself included—perform a PRK with the excimer to make minor corrections, if necessary.”
|
• Hyperopia. The other arena in which SMILE can’t compete with LASIK, yet, is in hyperopia. SMILE is currently only approved outside the United States for myopic corrections. The main challenge is the transition zone on the edge of the lenticule. “I know the company is studying how to optimize the lenticule’s shape in order to treat hyperopia,” says Dr. Hjortdal. “This is because, when you treat hyperopia with SMILE, you need to remove a sort of doughnut-shaped piece of cornea, and you need smoothing at the periphery of the doughnut so as not to have an abrupt change in corneal thickness.” Dr. Mehta says regression has been the main negative effect. “Walter Sekundo’s group in Germany has done some hyperopic treatments,” Dr. Mehta says. “And they’ve found they’re not as stable as myopic treatments. There’s been regression in the hyperopia. They’ve currently changed some of the nomogram, so I hope to be testing that out for them soon.”
Though SMILE has some areas that could be improved, Dr. Mehta says it’s moving in the right direction. “I think LASIK is technically easier to do: You just make a flap and the excimer does the treatment for you,” he says. “With SMILE, there is definitely a learning curve with the technique in order to recognize the planes of the lenticule, visualization and the like. However, instruments make a huge difference, and the instrumentation for SMILE is a lot better than it was when I started three years ago. That’s been a big improvement.” REVIEW
1. Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1,500 SMILE procedures. Ophthalmology 2013 Dec 20 pii: S0161-6420(13)01064-6. doi: 10.1016/j.ophtha.2013.11.006. [Epub ahead of print].