When it comes to asking surgeons about tracking their cataract outcomes, the phrase “turning a blind eye” might be tongue-in-cheek, but nevertheless fitting. A fair number of surgeons aren’t in the habit of routinely measuring outcomes, whether they’re simply uninterested in the data or concerned about being judged.
On the other hand, if they feel there’s just no reliable system to help them do this, that’s quickly changing, as some of the field’s most prominent names are rolling out technology that takes your data and then makes recommendations to hone your outcomes. This month, we’re taking a look at the various current and upcoming platforms that surgeons may want to consider.
Five Star Surgeon
Arturo Chayet, MD, founder of Centro Oftalmológico de Tijuana (CODET) Vision Institute in Tijuana, Mexico, has been in the ophthalmology field for three decades. He readily admits, however, that tracking his results wasn’t always a regular practice. “Since I’ve been implanting IOLs, I’ve been just as happy knowing that the surgery went well without complications, and I was comfortable doing adjustments postoperatively in case we missed the target,” he says. But as he attended lectures on newer IOL technology, Dr. Chayet realized his results weren’t as good as he thought.
“Using technology from the previous generation, like the IOL Master 500, my percentage within a 0.5 D SEQ was around 78 to 80 percent, which was the standard worldwide at the time. There were a few surgeons I was hearing about getting 90 to 95 percent, and they claimed it was because they were tracking results on a monthly basis,” he says.
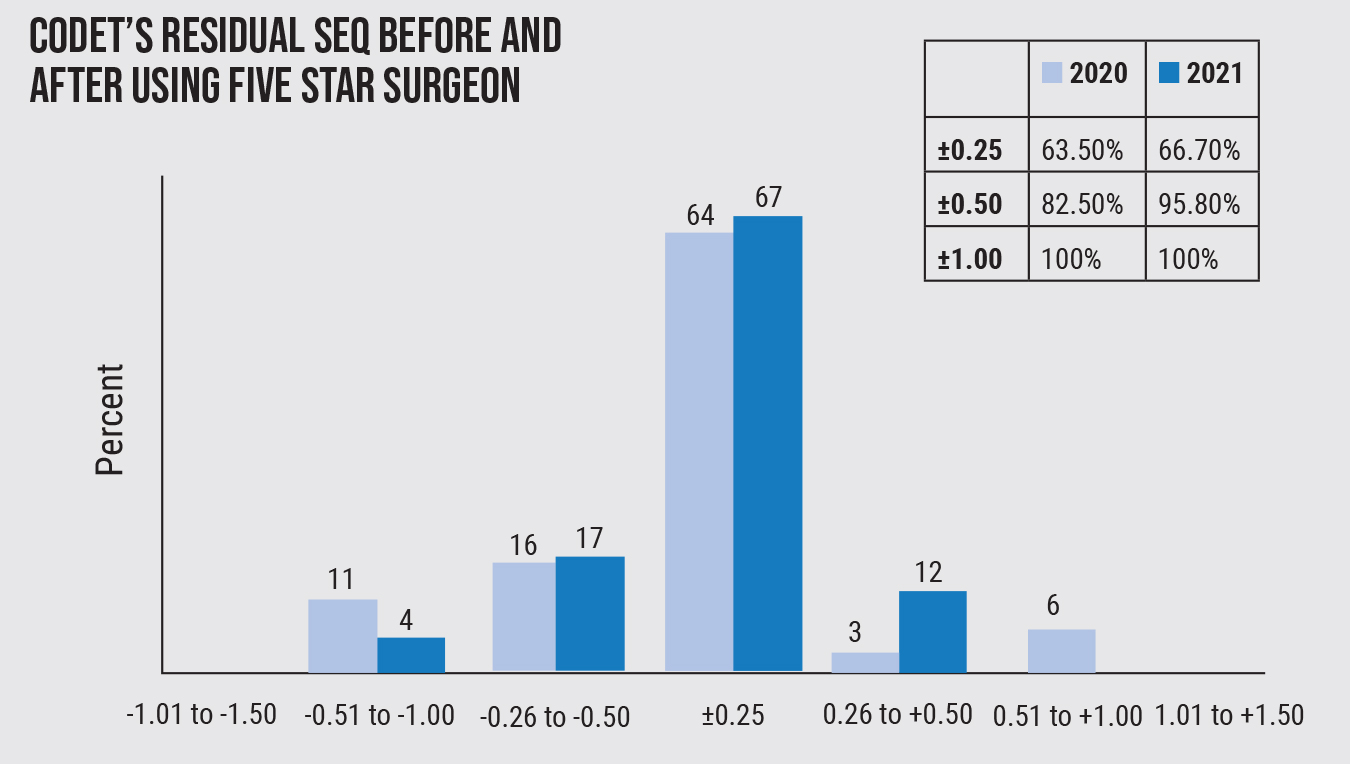 |
| Figure 1. Since implementing the Five Star Surgeon platform, surgeons at CODET Vision Institute have improved residual SEQ outcomes, and gotten closer to intended targets. |
Just before the pandemic, Dr. Chayet started to track his results. He specifically wanted to look at how he could be better in terms of toric astigmatic correction. “When I went to analyze the results, it was really difficult,” he says. “If your spherical equivalent isn’t on-target, your patient won’t see 20/20. So I started to think about how we can analyze the spherical equivalent and astigmatism at the same time. The best results I saw I decided to call ‘five-star.’ These are patients with less than 0.25 D for both cylinder and SEQ, and with uncorrected vision of 20/20.”
Prior to 2018, Dr. Chayet didn’t mind if the patient had 20/30 uncorrected vision and had minimal complaints. Tracking results helped him discover that the closer he was to emmetropia, not only did it produce five-star results, but complaints went way down. “We immediately noticed that our practice started to be a happier place,” he says.
Dr. Chayet co-created the Five Star Surgeon platform, a tracking system that accounts for SEQ, residual refractive astigmatism, visual acuity and patient satisfaction with Dr. Erik Navas, an anterior segment and refractive surgeon and a cornea and refractive fellow at CODET who helped create the algorithm. Five Star Surgeon also aims to provide insights about making adjustments and improvements in technique.
Daniel Chayet, CEO of CODET, says the platform presents different variables for surgeons to input.
“Imagine a checklist: Which IOLs are you using? Which biometers are you using; which formulas are you using? What toric calculator are you using? Are you using femtosecond lasers for cataract surgery? Are you doing it without a femtosecond laser, etc.? The platform is able to track all of that information,” Mr. Chayet explains.
Results are likely to be improved once a surgeon implements the right technology, and Five Star Surgeon plans to get into even more detail, asking how the patient is marked, how much astigmatism is induced by the incision and whether viscoelastic is being left in the chamber and causing IOL rotation. “This might narrow down if it’s a technique issue that needs to be addressed,” Mr. Chayet says. “But essentially, you’ll be able to go through all of your different results and find out what you did to get the highest or best result, or what you didn’t do that caused the lower results.”
They estimate a minimum of 20 patients with varying data would need to be included to make reliable determinations.
It’s been a little more than a year since Dr. Chayet and CODET started using the Five Star Surgeon platform, and it’s already revealed areas in which they can improve technique.
“Just before ASCRS, we went to analyze 72 cases of trifocal lenses—which really need to land close to zero with emmetropia, otherwise patients really start complaining and results aren’t that good,” Dr. Chayet says. “We found that we actually improved our results to 4.85 stars for SEQ and 4.75 stars for cylinder, an average of 4.79.”
They say the platform also benefits fellows. “If the surgeon leverages the insights provided by the platform, it creates uniformity,” explains Dr. Chayet. “Even though I’ve implanted 15,000 IOLs, my fellows who have only done 200 are capable of getting the same results.”
Although the platform is currently only on Excel, the group wants to get it into the hands of other surgeons, provided they can do so in the best and most efficient manner possible. Daniel Chayet says they have an illustrative prototype that’s essentially a basis for a full-fledged app, which they aim to develop over the next few months.
“We have to start working on the back end to create both a mobile and web version of the platform,” Mr. Chayet says. “But as you can imagine, scaling this out to surgeons, specifically in the U.S., will be another undertaking. We’re looking to potentially partner with a manufacturer, and there’s no question there’s interest.”
Dr. Chayet calls the Five Star Surgeon platform “the missing piece” in the IOL ecosystem. “Surgeons do great surgeries, but every once in a while a patient complains of bad results and you feel like you want to ignore the problem,” he says. “But something as simple as analyzing your results and trying to improve them can make a difference. Results that are consistently within 0.5 D of the intended target for both SEQ and CYL aren’t even in the hands of 5 percent of surgeons worldwide. IOLs are the number-one procedure performed in the body. I think it’s time to deliver better results to people.”
Cataract Boost
Available in a free Android and online app, Cataract BOOST (Better Operative Outcomes Software Tool) captures key cataract outcome data and translates it into reports and feedback for performance improvement.
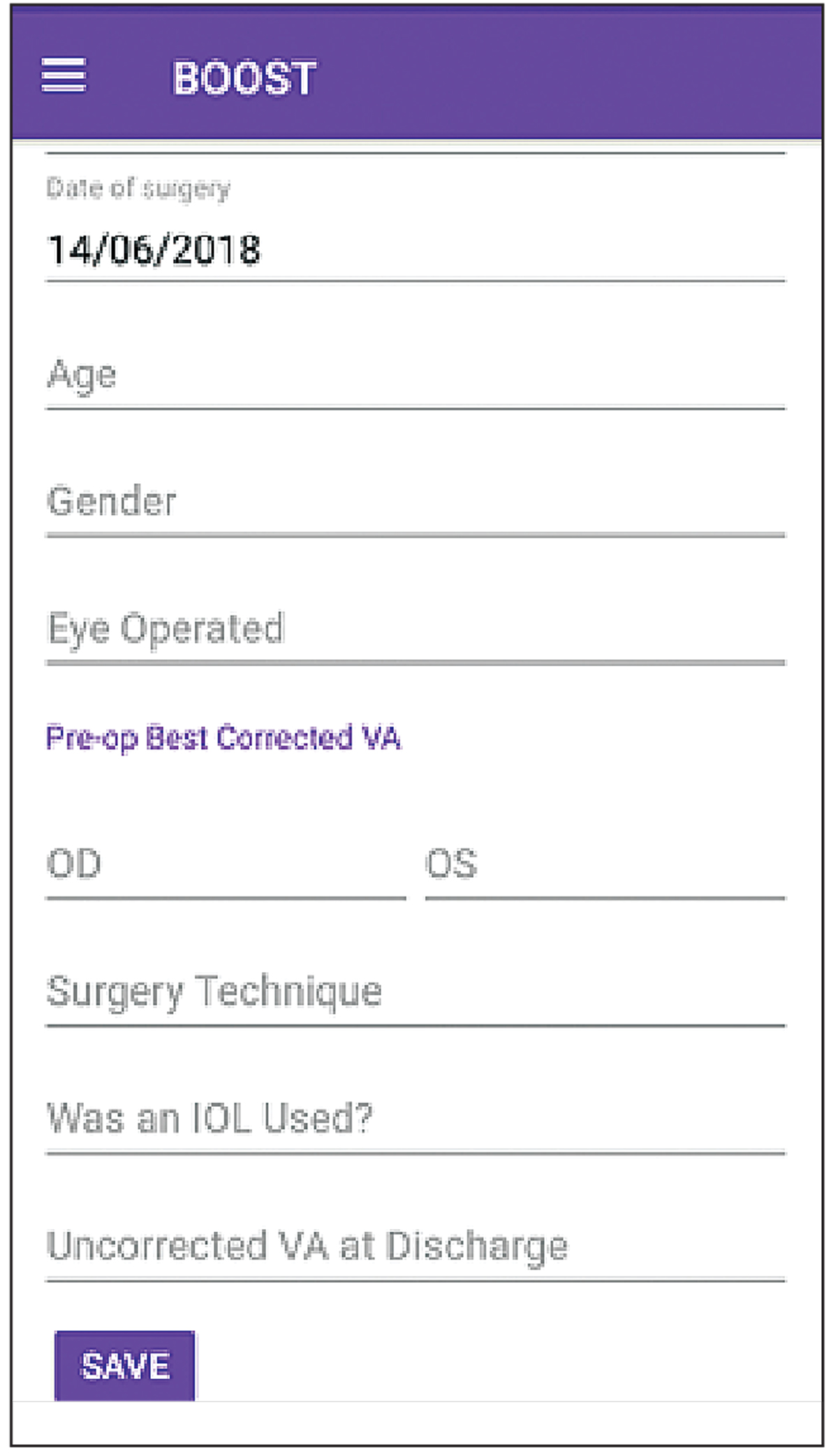 |
| Figure 2. Available for free download, the BOOST app is designed to measure simple and easy-to-gather data, including preop vision in both eyes, postop vision in the operative eye, and the age and sex of the patient. An assessment of surgical quality can be made after 60 consecutive cases have been entered. |
Motivated by the desire to improve the quality of cataract surgical outcomes in low-resource areas, a consortium of eye-health organizations supported BOOST’s development, which included Professor Nathan Congdon, chief investigator and Ulverscroft Chair of Global Eye Health at Queen’s University in Belfast.1 However, the app has value for ophthalmologists worldwide and is available in seven languages.
One of the primary factors BOOST tries to address is the low postoperative follow-up rates in low- and middle-income countries. “BOOST is based on a study called PRECOG, published in Lancet Global Health, which showed that measuring vision about one to two days after cataract surgery could be an accurate predictor of final outcomes, and that 50 percent or more of patients don’t return for later visits,” Prof. Congdon says. “Thus, BOOST is designed to measure outcomes in the first days after surgery, when patient follow-up adherence is best.”
BOOST is designed to measure very simple and easy-to-gather data, he continues. This includes the vision in both eyes before surgery, vision in the operative eye after surgery, and the age and sex of the patient. Assessment of surgical quality can be made after 60 consecutive cases have been entered.
“Additionally, many users also want recommendations on how to improve their outcomes—not just an assessment of how good they are,” says Prof. Congdon. “To give recommendations to improve quality, data for 20 consecutive patients with bad outcomes must be entered, such as a missed diagnosis of another eye problem during the preop exam, problems that occurred during the surgery or problems that can be corrected with glasses.”
Should a surgeon find that the presence of other diseases is the most common cause of a bad outcome, BOOST will make specific recommendations to address the issue, such as a more thorough preoperative eye exam “with dilation of the pupil after checking for an afferent pupillary defect.”1
Both technique- and technology-based recommendations are made, depending on the specific reason for poor outcomes. Data are password-protected, and no patient identifiers such as names or addresses are ever entered. A surgeon can share their results by sharing their password, says Prof. Congdon.
The consortium believes BOOST can change the monitoring paradigm in cataract surgery, leading to the creation of a standard, global cloud-based database.
“There’s no doubt that smartphone apps have enormous potential to improve human health, as long as potential users have access to a smartphone and adequate vision to use it (not always the case, as our studies have shown),” Prof. Congdon says. “Apps like BOOST have the potential to drastically increase use of health care in low-resource settings, as long as we resolve barriers to their access. That means free or low-cost apps, and adequate vision care to be able to see to use them.”
Eyetelligence
First introduced in 2018, Eyetelligence from Bausch + Lomb is a cloud-based data management platform that endeavors to improve clinical performance and efficiency in surgical facilities. Eyetelligence is connected to the manufacturer’s Stellaris Elite vision enhancement system; it eliminates the time-consuming nature of manual data entry.
Mitchell Shultz, MD, co-founder and chief medical officer of Shultz Chang Vision in California, was involved in the initial beta testing of Eyetelligence. “Before using Eyetelligence, we had to do things manually, which was tedious, to basically record the data and create Excel spreadsheets. Now, the system can do that for you,” he says.
The Eyetelligence app syncs information from surgeries that Dr. Shultz performs and stores it on the cloud. Any modifications made on one machine are transposed to all other machines, no matter what operating room or location.
“As we’ve made modifications, we’ve been able to look at their effectiveness, as far as whether or not they have an impact on day-one postoperative corneal clarity, and it’s shown that reducing energy does in general translate to clearer corneas postop day one,” he says. “We do know the more energy we use, the more chance there is of having delayed healing.”
This technology will soon be taking things a step further, Dr. Shultz explains, as Bausch + Lomb is expected to launch the next generation Eyetelligence platform this fall, which will help surgeons track outcomes and influence treatment planning for future patients. The company announced last year2 that it’s partnering with Lochan, a software development company founded by Dr. Mark Lobanoff.
“Now, in addition to having the capacity for getting better information out of the Stellaris Elite, there will be cataract surgery planning tools that will take information from our topographers and optical biometers and start to use artificial intelligence to help fine tune our IOL planning and calculations,” Dr. Shultz says. “It will also help postoperatively, looking at surgeon-specific results and helping to improve those results.”
One thing he’s looking forward to in particular with Eyetelligence is that it’s open source. “There are some rigidities in the existing systems that make it challenging when you’re planning, if there’s a slight error between your EMR and your devices, such as if the name is put in wrong; it can be challenging to fix those things,” says Dr. Shultz. “That’s something we’ve discussed with this platform to make it more user-friendly, so a surgeon or technician can make those adjustments quickly, as opposed to having to contact a support person at the manufacturer, which slows things down.”
IBRA Digital Health Suite
Zubisoft launched its Ibra system in 2004 and has continued to improve upon it. Ibra is available in several specialties, including cataract services. The standalone application cataract suite offers A-constant optimization, SIA calculation, IOL matching and outcomes, among others. Zubisoft says Ibra’s benefits include more accurate IOL matching, improved productivity with shorter consultation times and optimized integration of subjective and objective data.
Karl Stonecipher, MD, medical director at TLC Laser Eye Center in Greensboro, North Carolina, clinical professor of ophthalmology at UNC and clinical adjunct professor at
Tulane University, says Ibra is useful for both new and veteran surgeons.
“Ibra is helpful to fellows, new cataract and refractive surgeons and older cataract and refractive surgeons who are looking to improve their outcomes,” Dr. Stonecipher says. “You’ve got to start somewhere, as a young resident or a more experienced surgeon who’s never collected data at all. Many surgeons will say, ‘All my patients end up 20/20.’ But when you look at the data, it’s a completely different story.
“This helps me improve my outcomes,” he continues. “For example, you can determine if your technique is inducing astigmatism, or if your A-constant is up to date, after you’ve done as few as 50 lenses. It lets you look at how you’re doing, whether that’s refractive-wise post-cataract surgery or for uncorrected visual acuity after laser vision correction,” he says. “Maybe I want to look at my attempted versus achieved, or I want to look at my R2 values—if mine is a 0.99, I’m doing great. If it’s a 0.5, though, I’m not doing too well.”
The data on Ibra is anonymous but allows surgeons to benchmark their results against thousands of surgeons using the specific technology. For instance, this can be helpful for a cataract surgeon’s A-constants, Dr. Stonecipher says. “If the Europeans get the PanOptix lens before the Americans do,” he explains, “I can look at all the A-constants from the Europeans and then I can develop my own after 50 patients; or my Haigis constants or my astigmatic results—I can look at all those outcomes from other surgeons and benchmark myself compared to somebody else. Maybe my marking of the cornea isn’t working as well as using intraoperative aberrometry works. This might make me say, ‘Well, maybe I’d better go get intraoperative aberrometry.’ ”
Any software presents its own set of challenges, he continues. “If the surgeon isn’t entering the data, they’ve got to find the detail-oriented staff member in their office to do it. I’ve picked the wrong person in the past,” he says. “If you assign someone the task of putting data in for 100 people, and it’s all wrong because they didn’t know the difference between minus cylinder or plus cylinder, it’s all useless. Ibra will flag it if it doesn’t make sense when you’re entering the data, so there are checks and balances in the system.”
Early adoption of outcome tracking is going to be key for patient satisfaction, Dr. Stonecipher posits. “I’m encouraging all of my students because making patients happier needs to start when you’re a resident,” he avers. “If you can institute it in the residence clinics, that’s going to get their practice patterns moving forward. If you have a surgeon who’s starting to use a new intraocular lens, new laser, new technology or new techniques, I think they all should adopt something to look at their outcomes. But that needs to start early, because once that horse is out of the barn, it’s kind of hard to rein it back in.”
Veracity
Florian Kretz, MD, FEBO, medical director of the Augentagesklinik Rheine & Greven, in Greven, Germany, says tracking outcomes has always been part of his practice. “We’re not controlling every single patient, but we always perform internal studies where we look at the quality of our outcomes.”
However, the tediousness of entering data into Excel sheets was time-consuming, and there was no connection with the patients’ electronic health records. A key component in Zeiss Medical Technology’s Veracity Surgical platform is its ability to pull data from EHRs. The web-based software brings together patient data and diagnostics to build personalized preferences for its users and optimize future outcomes using postop data and analytics.
Although Veracity is awaiting CE approval in Europe, Dr. Kretz is currently using a different platform from Zeiss called EQ Workplace to track data and save time in the OR. Veracity would allow Dr. Kretz to enter much more postop data to optimize his outcomes and make his own constants.
“If the technology is working properly and you can basically transfer data wirelessly without any risk of data loss or incorrect input, then it can really change outcomes of patients,” he says. “Everybody has their own surgical technique, and that influences the A-constants, the induced astigmatism and the change of axis that you implement. Being able to implement a system that takes all the data preop, intraop and postop, enables you to become even more precise, especially for the premium cases, and you can also make your own nomograms for the latest lasers.”
Dr. Kretz says the accuracy of seamless connectivity to EHRs remains to be seen. “I’ve heard Veracity will have seamless connection, but connectivity can be quite low and there’s no seamless connection to any other devices—you can just import PDFs, not the raw data. When you can work with the raw data on one platform from different devices, that’s what’s really going to push the quality of our surgery forward even further,” he concludes.
Dr. Schultz is a consultant and investigator for Bausch + Lomb. Dr. Stonecipher is a consultant for Zubisoft. Dr. Kretz is a consultant for Carl Zeiss Meditec. Dr. Chayet, Dr. Navas and Mr. Chayet report no financial disclosures associated with the topic at this time.
1. BOOST Consortia 2022. Better Operative Outcomes Software Tool (BOOST). Accessed May 30, 2022. https://boostcataract.org/about.html.
2. Bausch + Lomb and Lochan enter into agreement to develop the next-generation of eyetelligence clinical decision support software. Accessed May 25, 2022. https://www.prnewswire.com/news-releases/bausch--lomb-and-lochan-enter-into-agreement-to-develop-the-next-generation-of-eyetelligence-clinical-decision-support-software-301307293.html.