Presentation
A 54-year-old Caucasian male presented to the Wills Emergency Room with a four-day history of severe, throbbing right eye pain and redness. He noted that he had been blind in this eye for two years with intermittent pain over the past six months and an acute exacerbation four days prior to presentation. He denied recent eye trauma or surgery. Review of systems was negative for fever, chills, weight loss, chest pain, shortness of breath, abdominal pain, headache or arthralgias.
 |
Medical History
Past medical history was notable for a dental surgery three months prior to presentation, for which the patient took post-procedure oral antibiotics. Ocular history was remarkable for glaucoma of unknown type diagnosed at an outside hospital about two-and-a-half years prior, which was managed by bimatoprost in both eyes. He reportedly lost vision in the right eye six months later. Approximately one year prior to presentation to the Wills Eye Hospital Emergency Room, the practice caring for him closed and the patient stopped taking his glaucoma medications.
Examination
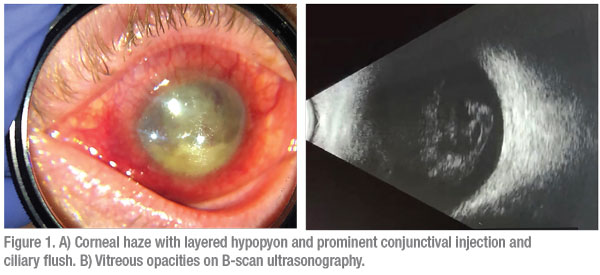
The patient’s vital signs were stable and normal. Ocular examination showed visual acuity of NLP in the right eye and 20/20 in the left eye. IOP by applanation was 36 mmHg OD and 34 mmHg OS. Pupillary examination revealed an afferent pupillary defect OD. Extraocular motility was full. Exam of the right eye (Figure 1A) revealed an edematous and erythematous upper lid. The conjunctiva and sclera had 3+ ciliary flush, 2+ injection and no bleb was seen. The cornea was hazy and edematous with microcystic edema and scattered bullae. No epithelial defect, distinct infiltrate or ulceration was noted; however granulomatous keratic precipitates were present. The anterior chamber was shallow with a 3.3-mm, layered hypopyon. The pupil was round and without evidence of sphincter tear. A white cataract was present. There was no view of the fundus. B-scan ultrasonography revealed vitreous debris (Figure 1B). Examination of the left eye was normal, with the exception of trace nuclear sclerotic cataract. The left optic nerve appeared healthy, without notching, hemorrhage or thinning, and had a vertical cup:disc ratio of 0.15. Gonioscopy couldn’t be performed OD due to corneal haze. Gonioscopy OS demonstrated an open angle (Spaeth classification D40f).
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.



