Presentation and Initial Work-up
A 36-year-old female is referred to an otolaryngologist for evaluation of rhinorrhea. The patient reported that for the last month, she had been experiencing continuous drainage of “saline-like” fluid out of her nose. She also endorsed a headache, pressure over her sinuses and symptoms of congestion. She was initially diagnosed with acute sinusitis by her primary care physician and given a seven-day course of oral amoxicillin/clavulanic acid as well as a five-day course of oral prednisone. Due to minimal improvement in her symptoms and history of recurrent sinus infections, she was referred to ENT. The otolaryngologist performed a nasal endoscopy and diagnosed the patient with a CSF leak. Upon further questioning, the patient reported a history of idiopathic intracranial hypertension (IIH) treated with lumbar puncture in the past so she was referred to ophthalmology for further evaluation.
Upon initial assessment, the patient had a visual acuity of 20/20 in both eyes. Intraocular pressure was 20 mmHg in the right eye and 19 mmHg in the left eye. There was no relative afferent pupillary defect (rAPD). Confrontational visual fields and extraocular motility were full. Color plate testing was normal in both eyes. Slit lamp exam was unremarkable. Dilated fundus exam was notable for a gliotic appearance to the optic discs of both eyes but no edema or disc hemorrhage was noted. One week later, the patient was seen by a neuro-ophthalmologist with unchanged symptoms and exam. Optical coherence tomography of the optic nerves and macula were within normal limits. Humphrey visual field testing was normal. At that time, the patient was referred back to otolaryngology for further investigation of the etiology of the CSF leak.
Medical History
Past medical history was notable for obesity, hypothyroidism, bipolar disorder, anxiety and ADHD. Past surgical history was notable for prior Cesarean section and tonsillectomy. Apart from the history mentioned above, the patient didn’t have any other ocular history.
Family history was notable for a mother with breast cancer and a maternal aunt with systemic lupus erythematosus. Social history was significant for past tobacco use (unclear pack-year history). Review of systems was unremarkable.
Current medications included levothyroxine, fluoxetine, lamotrigine, trazodone and the ADHD medications lisdexamfetamine and dextroamphetamine.
What is your diagnosis? What further work-up would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
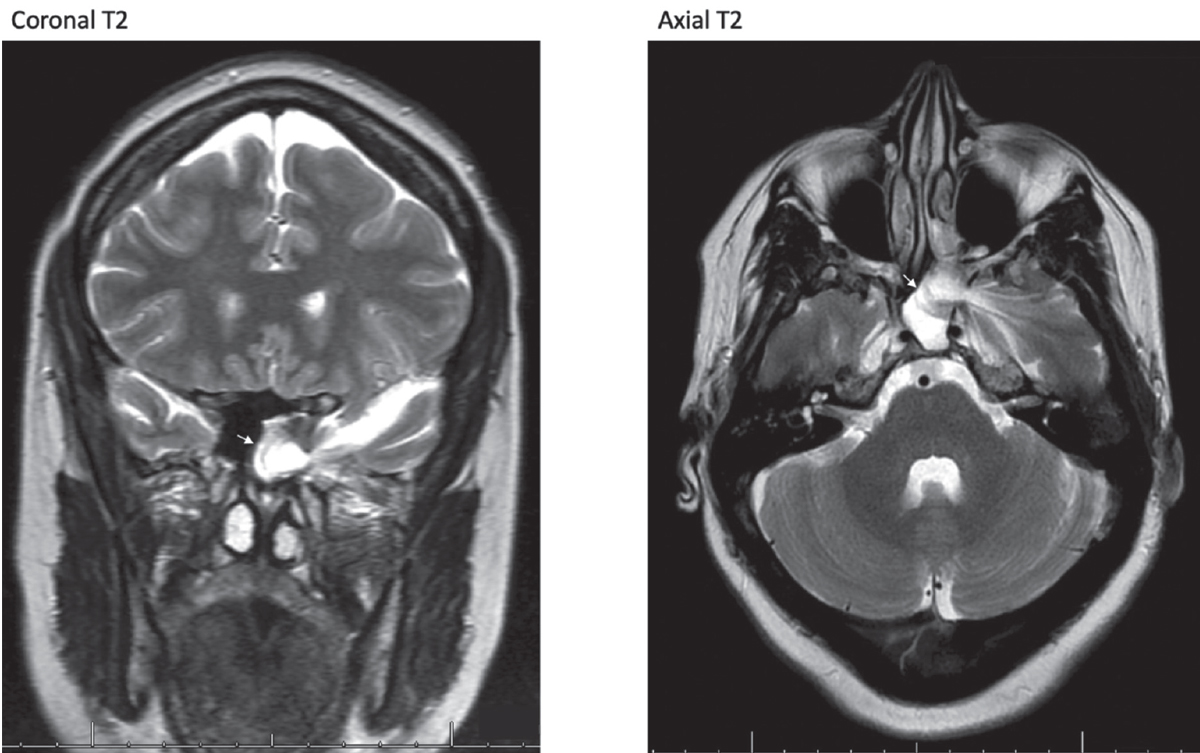 |
| Figure 1. MR imaging. Coronal (left) and axial (right) T2-weighted images showing left lateral sphenoid encephalocele (arrow). |
A computed tomography scan was obtained initially which showed near complete opacification of the left sphenoid sinus with a 6-mm defect in the lateral wall of the left sphenoid sinus. Magnetic resonance imaging was obtained and was notable for herniation of the anterior medial left frontal lobe into the sphenoid sinus with associated extension of the left sylvian fissure, representing encephalocele (Figure 1).
The patient underwent endoscopic endonasal repair of left sphenoid encephalocele, cranial base and CSF leak. Prior to surgery, a lumbar puncture was performed and the patient was found to have an elevated opening pressure of 41 cm H2O. A lumbar drain was unable to be placed at the time of surgery. On postoperative day one, the patient endorsed binocular horizontal diplopia. Ophthalmology was consulted in the inpatient setting. Evaluation at that time was notable for a visual acuity of 20/25 in both eyes, no rAPD, and IOPs of 12 in the right and 11 in the left eye. Color plates were full in both eyes as were the confrontational visual fields. The patient had a limitation in abduction of both eyes (90 percent abduction OD, 70 percent abduction OS). Anterior and posterior segment exams were unremarkable, with no disc edema or disc hemorrhage noted.
The suspected diagnosis at the time was exacerbation of idiopathic intracranial hypertension symptoms following repair of the encephalocele and skull base defect. Repeat MR imaging was notable for surgical changes related to endoscopic surgical repair of left sphenoid encephalocele with no evidence of residual encephalocele. The patient underwent neurosurgical VP shunt placement and was subsequently discharged on oral acetazolamide 500 mg twice daily. On one month outpatient follow-up with neuro-ophthalmology, the patient reported improvement in symptoms of horizontal diplopia. Her exam at that time was notable for full extraocular movements OD and a minor limitation in abduction OS (90 percent). Dilated fundus exam showed mild optic disc edema OD and OS which was corroborated on optical coherence tomography. Humphrey visual field testing was normal. On subsequent evaluation four months following encephalocele repair and VP shunt placement, the patient had complete resolution of diplopia and the PO acetazolamide was discontinued without issue.
Discussion
CSF leaks occur due to traumatic or non-traumatic causes. Causes of non-traumatic CSF leaks may be further subdivided by etiology including skull base abnormalities, bone erosion as a result of malignancy or hydrocephalus, or due to elevated intracranial pressure (ICP).1,2 Similar to the traditional demographics of IIH, patients that develop spontaneous CSF leaks and spontaneous encephaloceles are often young or middle-aged women with BMI greater than 30 kg/m2.3 In addition, radiographic features associated with IIH such as a partially empty sella turcica, arachnoid pits and dural ectasias are often observed in patients with spontaneous CSF leaks.4,5 As such, IIH has been associated with the development of spontaneous CSF leaks.6
The presence of a CSF leak may mask signs and symptoms of IIH due to the existence of an alternative outlet to CSF. This diversion of CSF prevents a large increase in intracranial pressure and thus may preclude the development of classic signs and symptoms of increased ICP such as headache, transient visual obscurations, pulsatile tinnitus and papilledema. Although our patient was previously diagnosed with IIH, a new diagnosis of IIH may be made following surgical repair of the CSF leak due to the emergence of IIH signs and symptoms.3, 4
Endoscopic repair is regarded as the preferred surgical intervention for spontaneous CSF leaks. Studies have shown that intervention for elevated ICP ahead of primary endoscopic repair for spontaneous CSF leaks reduces rates of recurrence and other complications following repair.7 Thus, intervention with acetazolamide, CSF shunt systems, and/or weight loss for intracranial hypertension should be considered prior to primary repair of a spontaneous CSF leak.
In conclusion, prompt evaluation for and diagnosis of IIH in a patient with a spontaneous CSF leak is critical. If IIH and ICP are identified, treatment with ventriculoperitoneal shunting, acetazolamide, and other measures such as weight loss should be undertaken prior to surgical management. Furthermore, patients should be followed closely in the postoperative period, as ICP symptoms may initially worsen.
1. Ommaya AK. Cerebrospinal fluid rhinorrhea. Neurology 1964;14:106-13.
2. Clark D, et al. Benign intracranial hypertension: A cause of CSF rhinorrhoea. J Neurol Neurosurg Psychiatry 1994;57:7:847-9.
3. Perez MA, et al. Primary spontaneous cerebrospinal fluid leaks and idiopathic intracranial hypertension. J Neuroophthalmol 2013;33:4:330-7.
4. Silver RI, et al. Radiographic signs of elevated intracranial pressure in idiopathic cerebrospinal fluid leaks: A possible presentation of idiopathic intracranial hypertension. Am J Rhinol 2007;21:3:257-61.
5. Schlosser RJ, et al. Elevated intracranial pressures in spontaneous cerebrospinal fluid leaks. Am J Rhinol 2003;17:4:191-5.
6. Brainard L, et al. Association of benign intracranial hypertension and spontaneous encephalocele with cerebrospinal fluid leak. Otol Neurotol 2012;33:9:1621-4.
7. Teachey W, et al. Intervention for elevated intracranial pressure improves success rate after repair of spontaneous cerebrospinal fluid leaks. Laryngoscope 2017;127:9:2011-2016.



