Workup, Diagnosis and Treatment
The differential was broad, and included infectious endogenous endophthalmitis, as well as non-infectious etiologies such as sarcoidosis and lens-induced uveitis. Neoplastic etiologies couldn’t be excluded, either. The main concern in the emergency room setting was infectious endophthalmitis. The patient underwent a vitreous tap and intravitreal injection of vancomycin, ceftazidime and voriconazole. The patient was admitted for an endogenous endophthalmitis work-up.
A comprehensive inpatient work-up was notable for elevated Lyme disease IgG and normal IgM, consistent with remote infection. Bacterial, fungal, mycobacterial cultures, HSV1/2, VZV, CMV and Toxoplasma PCR performed on the vitreous tap were negative. Systemic laboratory studies including blood cultures, galactomannan and fungitell were negative. Serologic studies for treponema pallidum, HIV, Anaplasma, and Ehrlichia were negative. Quantiferon gold was normal. The ESR, ACE and vitamin D levels were within normal limits. Imaging obtained included a transthoracic echocardiogram, which was normal. CT of the facial bones revealed multifocal dental disease.
 |
The patient was treated with intravenous vancomycin. Ocular medications included brimonidine b.i.d. OU, dorzolamide-timolol OU, ofloxacin q.i.d. OD, atropine b.i.d. OD and prednisolone acetate every two hours while awake OD. Although the patient experienced significant relief with topical ophthalmic medications, he continued to have pain in the chronically non-seeing eye and opted for enucleation.
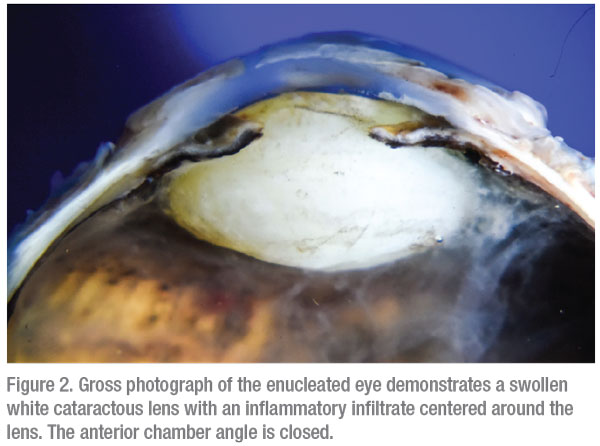
Gross evaluation of the enucleated eye demonstrated a swollen cataractous lens with inflammation centered around the lens. The anterior chamber angle was closed by peripheral anterior synechiae (Figure 2). Microscopic evaluation of the anterior chamber angle demonstrated findings suggestive of chronic post-traumatic angle recession. The lens capsule was ruptured. The lens cortex demonstrated extensive degeneration and liquefaction with Morgagnian globule formation. The lens fibers were infiltrated by neutrophils and focally by the granulomatous inflammation, composed of epithelioid macrophages and rare multinucleated giant cells (Figure 3A). These findings were reminiscent of phacoantigenic uveitis, although a distinct zonal pattern of inflammation was not present.
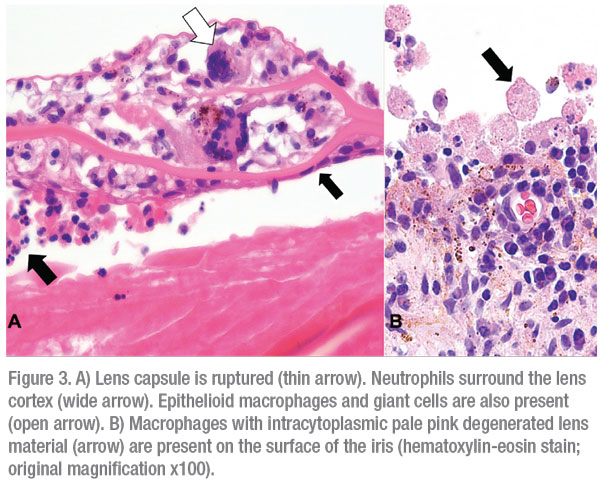 |
Also noted were numerous macrophages with intracytoplasmic degenerated lens protein in the anterior chamber, compatible with a phacolytic uveitis. (Figure 3B). Additional findings included chronic nongranulomatous iritis and vitritis and end-stage glaucomatous retinal and optic nerve atrophy.
Discussion
Lens-induced uveitis includes a group of intraocular inflammatory diseases characterized by an inflammatory response to lens proteins.
 |
Phacoantigenic uveitis (formerly known as phacoanaphylaxis) is a rare autoimmune condition that occurs when there’s an altered immune response to undenatured lens protein, precipitated by disruption of the lens capsule. Phacoantigenic uveitis is a type-3 immune-complex (antigen-antibody) mediated response that results in activation of the complement cascade and a zonal granulomatous response surrounding the lens fibers. Although previously the lens was thought to be immune-privileged, it’s now believed to be under immune surveillance. Notably, lens proteins are found in the aqueous humor of normal eyes, and antibodies to lens proteins are found in some individuals who don’t have a lens-induced uveitis.1 The loss of immunologic tolerance to lens proteins has been proposed to lead to phacoantigenic uveitis. In a clinical-pathologic review of 144 patients with phacoantigenic uveitis, the average patient age was 53.2 The majority were males (61 percent), who presented with NLP vision (78 percent) and low intraocular pressure (58 percent < 9 mmHg).2 Most cases were associated with trauma (80 percent); however, history of trauma wasn’t elicited in 20 percent of patients. The time from trauma ranged from a few days to nearly sixty years. Only 4 percent of patients were diagnosed accurately prior to histopathologic review of an enucleated eye. The five leading clinical diagnoses were phthisis, glaucoma, iritis, endophthalmitis and sympathetic ophthalmia.2
Phacolytic glaucoma occurs as a result of leakage of lens proteins from liquified cortex through an intact lens capsule. The lens proteins are then phagocytosed by macrophages, which block the trabecular meshwork, leading to a secondary open-angle glaucoma.
The treatment of lens-induced uveitis is to remove the inciting lens material. The therapy is tailored to the patient, and can include cataract surgery, anterior chamber washout, pars plana vitrectomy or enucleation.1
It’s important to note that remote trauma in our patient induced angle recession and contributed to the asymmetric glaucoma. It’s been documented that 60 percent of eyes with non-penetrating trauma will have some degree of angle recession; however, less than 10 percent of these will develop glaucoma.3 Interestingly, in those patients who develop traumatic glaucoma, the fellow eye that didn’t experience trauma has a 50-percent chance of developing glaucoma, suggesting that patients who develop traumatic glaucoma have an underlying predisposition to it.3 This observation appears to hold true for our patient in this particular case, who had ocular hypertension in the fellow eye.
In summary, our patient had a remote history of ocular trauma, which led to chronic angle recession and asymmetric cataracts. Histopathology of the enucleated eye showed a lens-induced uveitis, characterized by a mixed forme fruste phacoantigenic zonal granulomatous response and phacolytic macrophagic response. We speculate that lens-induced uveitis in our patient occurred as a result of lens capsular rupture of hypermature cataract, possibly precipitated by pre-existing traumatic lens capsular weakness or microscopic dehiscence. This case highlights the importance of eliciting a history of trauma, even if it’s from the distant past, in a patient with asymmetric glaucoma. REVIEW
1. Nche EN, Amer R. Lens-induced uveitis: An update. Graefes Arch Clin Exp Ophthalmol 2020;258:7:1359-1365.
2. Thach AB, Marak GE Jr, McLean IW, Green WR. Phacoanaphylactic endophthalmitis: A clinicopathologic review. Int Ophthalmol 1991;15:4:271-9.
3. Tumbocon JA, Latina MA. Angle recession glaucoma. Int Ophthalmol Clin 2002;42:3:69-78.



