Because prompt recognition of disease progression is the key to vision preservation, a recent study based out of Massachusetts Eye and Ear focused on whether detection of glaucoma progression is usually associated with concordance of structural and functional testing at the same clinic visit or not.1 The researchers’ longitudinal study over a five-year period found that both OCT structural parameters (i.e., RNFL thickness and minimum distance band rim thickness) and Humphrey visual field (HVF) functional parameters rarely progressed at the same time. Notably, the classic tests of structure and function detected disease progression in the same eye at the same visit in only 5 percent of eyes.
“The classic teaching for many residency programs is that tests of structure have to match tests of function,” says study co-author Teresa C. Chen, MD. “For example, a healthy nerve should match a normal visual field test. So, if you have a normal nerve measurement but an abnormal visual field test, then one should suspect that perhaps one of the tests is inaccurate. In the present study, however, there was very little agreement between when tests of structure worsened and when tests of function worsened.”
 |
|
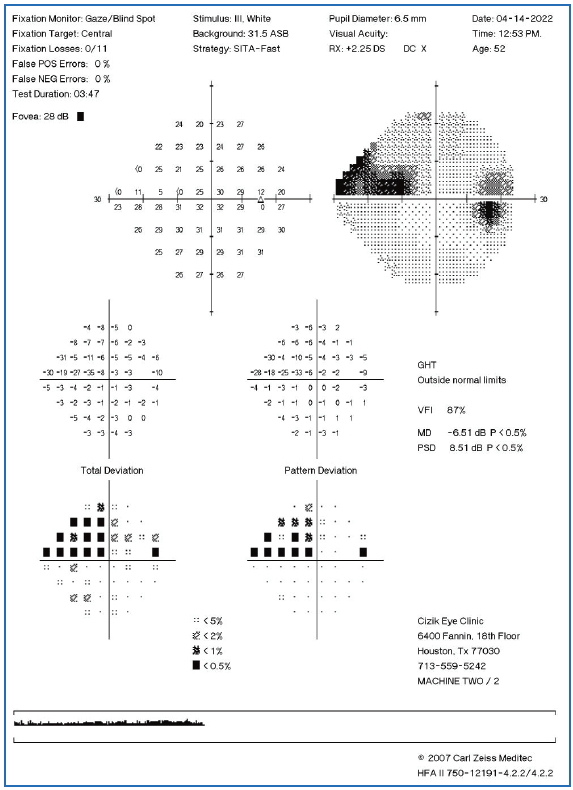
A longitudinal study found that visual field parameters and OCT structural parameters rarely progressed at the same clinical visit. |
In the study of 124 open-angle glaucoma patients, one eye was randomly selected for each patient. Patients were included if they had open-angle glaucoma and if they had at least four yearly study visits. Study visits included a full dilated eye exam, disc photography, Humphrey visual field (24-2) testing, 2D OCT RNFL thickness measurements and a 3D OCT neuroretinal rim measurement called minimum distance band, “the high-density version of the commercially available low-density Bruch’s membrane opening-minimum rim width,” the authors explained in their paper for the American Journal of Ophthalmology. For each test at each study visit, eyes were classified as progressors or non-progressors using event-based analysis.
The study found that 75 percent of eyes showed glaucoma progression by at least one of four tests by the end of the study period. The best overall agreements, including eyes of all glaucoma severities, were observed between minimum distance band thickness and RNFL thickness (17.5 percent of eyes) and between minimum distance band thickness and Humphrey visual field testing (16.1 percent), while the poorest agreements were observed between disc photography and RNFL thickness (5 percent) and between disc photography and Humphrey visual field testing (3.3 percent). Instead, progression is usually detected by just one or two tests (62.9 percent [78/124] of the time).
“This suggests that the higher sensitivity of the minimum distance band compared with traditional disc photography leads to better agreement in detecting progression at the same time as functional Humphrey visual field testing,” the researchers wrote in their paper. “This novel minimum distance band rim thickness OCT parameter measures neuroretinal rim thickness in 3D space and is a high-density version of the commercially available low-density Bruch’s membrane opening-minimum rim width.”
The researchers also explained in their paper that structural tests may better detect progression in pre-perimetric or early-stage glaucoma patients, while functional Humphrey visual field testing may detect progression better in advanced glaucoma patients.
“These are important findings, because if a clinician sees that the structural test is worse, that could really mean disease progression, and we don’t necessarily need to have progressive functional vision loss to confirm that,” Dr. Chen says.
If one test shows progression and the other doesn’t, she advises checking for artifacts and testing accuracy, and if any issues are present, consider repeating the test. In contrast, “if the test demonstrating progression seems accurate, if the reliability indices are good, and/or if there aren’t any testing artifacts, then a repeat test may not be needed. Then one would be more likely to initiate treatment,” she explains.
“It’s important for clinicians to realize that tests of structure can get worse at different times than tests of function,” Dr. Chen says. “As long as we understand this as our general framework when looking at tests in the clinic, we’re more likely to make the right treatment decisions for our patients. It’s recommended that clinicians use all available structural and functional testing to assess glaucoma progression.”
Dr. Chen has no related financial disclosures.
Teresa C. Chen has received funding from Fidelity Charitable Fund (Harvard University), National Institutes of Health (NIH) R01 EB033321, NIH R44 EY034409, NIH UG1 EY033703, Alcon Laboratories, NIH UL1 RR025758, Massachusetts Lions Eye Research Fund, American Glaucoma Society Mid-Career Award. The sponsors or funding organizations had no role in the design or conduct of this research.
1. Manik D, Ratanawongphaibul K, Kim J, et al. Frequency of agreement between structural and functional glaucoma testing: a longitudinal study of 3D OCT and current clinical tests. Am J Ophthalmol. May 27, 2024. [Epub ahead of print].
Controlling Hypertension May Help Delay DR
Researchers recently investigated the relative impact of hypertension vs. diabetes on the wall-to-lumen ratio (WLR) of retinal arterioles in diabetic retinopathy.1 Their prospective cross-sectional study aimed to address the unresolved question of whether there is a difference in WLR between healthy subjects and those with diabetes mellitus before the onset of clinical retinopathy (DR) and if so, whether the increase in WLR is mainly driven by diabetes or hypertension.
 |
The study compared the retinal arteriolar WLR in 17 healthy eyes, 15 with diabetes but no apparent DR and eight with diabetic macular edema (DME) and either nonproliferative or proliferative DR. Adaptive optics scanning laser ophthalmoscopy (AOSLO) and multiple linear regression were used to quantify the WLR and determine the effects of age, hypertension and diabetes.
The results showed that both subjects with diabetes but no apparent DR and subjects with DME had significantly higher WLR in retinal arterioles compared to healthy subjects. The mean WLR for healthy subjects was 0.29, while for subjects with diabetes and no DR it was 0.36, and for subjects with DME it was 0.42.
When analyzing the correlation between WLR and hypertension, diabetes and age, it was found that in healthy subjects and subjects with diabetes and no DR, hypertension had the strongest effect on WLR. The analysis also showed that hypertension and WLR shared a significant positive correlation, though age and diabetes were not significantly correlated with WLR in these groups.
In the analysis that included all three groups (healthy, diabetes no DR, and DME), diabetes had the strongest effect on WLR, and the two variables were positively correlated. Age and hypertension were not significantly correlated with WLR in this analysis.
While the small sample in this study limits its effect size, its results support the hypothesis that hypertension may be an early driver of retinal arteriolar wall thickening in preclinical DR, independent of age or diabetes. On the other hand, changes specific to DR may drive wall thickening in DME and later stages of DR.
“Our study sheds light on, and begins to address, an important gap in our knowledge regarding the relative contribution of hypertension (early) and diabetes (later) in the course of DR,” the researchers wrote in their study. “Understanding the pathogenesis of preclinical DR is important for the development of treatments to prevent DR onset and progression.” Additionally, “These findings highlight the importance of optimizing blood pressure control in individuals with diabetes mellitus even prior to the onset of DR,” they noted.
1. Huang BB, Fawzi AA. Hypertension likely drives arteriolar wall thickening in preclinical diabetic retinopathy while diabetes drives wall thickness in clinical retinopathy. Transl Vis Sci Technol. 2024;13(6):8.
SLT’s Popularity as a First-line Treatment Grows
A recent survey was conducted to assess the practice preferences of ophthalmologists for the initial management of glaucoma.1 The researchers hypothesized that the multitude of options and accumulated evidence for primary open-angle glaucoma treatment in the past decade will reflect a different preference pattern than reflected in a retrospective claims analysis of data from 2007 to 2014 that selected patients with their first open-angle glaucoma diagnosis in 2010. Their study, which was published in the Journal of Glaucoma, revealed that, for the first-line treatment of primary open-angle glaucoma, selective laser trabeculoplasty was more likely to be preferred over topical drops by U.S. physicians who are relatively new in practice, who have a larger glaucoma patient base and who perform more minimally invasive glaucoma surgeries.
The study determined to characterize primary treatment preferences (topical medication vs. laser trabeculoplasty or intracameral sustained release implants) in primary open-angle glaucoma patients and determine factors related to primary intervention selection. A 33-question survey was distributed to an American Society of Cataract and Refractive Surgery database on treatment choices made by ophthalmologists for POAG. Data collected included country of practice, years of practice, completion of glaucoma fellowship training, type of practice and preference for first-line treatment of POAG. A total of 252/19,246 (1.3 percent) of surveys were returned.
Multiple logistic regression determined that about 73.6 percent of respondents used topical medication as first-line of treatment for POAG, while 26.4 percent preferred to start with laser treatment. Significant variables associated with the selection of laser (vs. drops) are practicing in the US (odds ratio [OR]: 2.85), more recent completion of ophthalmology residency (OR: 1.95), greater volume of MIGS (OR: 1.68) and a glaucoma patient base greater than 25 percent (OR: 2.21).
For doctors preferring laser treatment as the first-line of treatment, the leading indications for using Durysta (bimatoprost SR, Allergan), a prostaglandin analog, are for patients that show intolerance to drops (about 19 percent), are non-responsive to selective laser trabeculoplasty (17 percent) or wish to reduce medication dependence (17 percent). For doctors preferring drops/topical treatment as the first-line of treatment for primary open-angle glaucoma, the leading indications for using bimatoprost SR are for drop intolerance (about 25 percent), noncompliance (about 26 percent) or as an alternative to medication dependence (17.5 percent).
“It was also observed that the majority of either group, laser or topical drops first, preferred a trabecular meshwork bypass stent in cases of moderate primary open-angle glaucoma and visually significant cataract,” the study authors wrote in their paper. “Although this questionnaire was not designed to ascertain the reason for this finding, it is likely reflective of a shift in preferred practice and community standards based on the relative safety and efficacy of this combined approach.”
“The results of this survey demonstrate a continuing unmet need to educate our colleagues on evidence-based treatment results for primary open-angle glaucoma,” they concluded.
1. Rhee DJ, Sancheti H, Rothman AL, et al. Primary practice patterns for the initial management of open angle glaucoma. J Glaucoma. June 17, 2024. [Epub ahead of print].
Surgery for Adult-onset Strabismus Proven Effective
Recent studies have shown that the incidence of strabismus in adults is on the rise, possibly attributable to factors such as age-related anatomical changes, increased use of digital devices, certain neurologic conditions or systemic diseases and improved diagnostic techniques and awareness among healthcare professionals. The estimated lifetime risk of developing adult-onset strabismus currently hovers around 4 percent, with esotropia accounting for about a quarter of these cases.
Most previous studies on esotropia grouped all adults together, which complicates surgical outcome analysis considering the pathophysiology of esotropia may differ in younger and older individuals. One type of esotropia occurring almost exclusively in younger adults is acute acquired comitant esotropia, associated with a moderate to large angle, diplopia, full ocular motility and lack of neurologic or anatomic etiology. In a new study, researchers attempted to analyze how certain characteristics, such as age, affect surgical outcomes in this patient population.1
The retrospective case series analyzed medical records of adults aged 18 to 60 who underwent strabismus surgery at a tertiary care hospital for comitant non-accommodative esotropia. The majority of patients were female (64 percent) and the mean age was 36.7 years. Nearly three-quarters (72 percent) of the cohort were myopic and 80.3 percent had diplopia. To distinguish between etiologies, patients were classified into three groups based on the disparity between near-distance angles of deviation: basic esotropia (ETBA), esotropia divergence insufficiency pattern (ETDI) and esotropia convergence excess pattern (ETCE).
The study found that the ETCE group had the largest mean deviations at both distance and near, while the ETBA group had the largest ranges at both distances. The two most popular surgical procedures, performed at equal frequency (both 48 percent of the cohort), were bilateral medial rectus recession (BMR) and unilateral recess-resect (R&R). The surgical outcome analysis showed that the latter procedure had higher motor and sensory success rates than BMR. However, all groups achieved excellent surgical success, regardless of surgical approach or esotropia pattern.
Though the pathophysiology of different patterns of esotropia remains largely unclear, one unique finding the researchers highlighted in their paper, published in the American Journal of Ophthalmology, “was the presence of anisometropia in approximately 13 percent of the cases. It is possible the disparate accommodative effort may be an unrecognized or underrecognized contributor to the development of esotropia.”
By analyzing demographic and clinical information from patients’ medical records, the researchers were able to characterize the typical patient with acute comitant esotropia undergoing surgery. “These patients tend to be younger adults, female and have moderate myopia,” as well as present with moderate angle basic type esodeviations, the researchers summarized in their paper. They added, “Surgical success in this group of patients is high regarding both motor and sensory outcomes,” which agrees with prior literature.
1. Cavuoto KM, Tibi C, Rosa PR, Capo H. Characteristics and surgical outcomes of comitant esotropia in an adult population between 18 and 60 years old. Am J Ophthalmol. 2024. [Epub ahead of print].



