Amitha Domalpally, MD and Ronald P. Danis, MD, Madison, Wis.
Fluorescein angiography is a powerful imaging modality to identify the presence, location and size of the neovascular complex, which is composed of the choroidal neovascular lesion and its associated components. FA is a useful diagnostic method and also an important clinical research tool, displaying lesion morphology data that is not otherwise available. Many clinical trials of AMD rely on FA characterization for both eligibility and treatment endpoints. Lesion morphology as determined by FA has implications for treatment response to some therapies as well as for natural history outcomes.
Treatment protocols in the Macular Photocoagulation Study were based on angiographic features, with clear benefit of laser treatment only for extrafoveal classic CNV lesions.1 The clinical trials of photodynamic therapy with verteporfin demonstrated a differential effect of treatment with classic lesions receiving the most benefit.2 The realization of this differential treatment effect by lesion appearance has subsequently been factored into many trials of neovascular AMD by specification of inclusion and exclusion of patients based upon FA interpretation. In many trials, eligibility is performed by the site clinical investigator, which makes the investigators' interpretation of FA important for enrollment of a sufficiently standardized patient population to detect a treatment effect with the calculated sample size. Enrollment of too many ineligible eyes may skew the predicted event rate (in regard to both visual and morphology outcomes) in a trial and cause the trial to statistically miss achieving its primary endpoint. Standardized interpretation of FA in AMD, with specific reference to the lesion composition and identification of angiographic subtypes of CNV, is therefore important for both clinical care and clinical research. The guidelines described in this article are adapted from the MPS and ETDRS protocols3 for evaluating fluorescein angiography and are used by the UW Fundus Photograph Reading Center,
Imaging Methods
• Imaging procedure: Stereoscopic FAs are obtained with either a film-based or digital system producing an approximately 30- to 40-degree field of view at approximately 2.5X magnification. Because stereoscopic viewing of digital images is cumbersome and requires more time (compared to film), some clinicians do not emphasize stereoscopic FA for clinical practice. However, stereoscopic photography and viewing is critically important for proper classification and measurement of CNV lesions and is always employed at the reading center.
As shown in Figure 1, the FA documents two fields of the retina, providing stereoscopic views of Field 2 (centered near the center of the macula) and Field 1M (centered on the temporal edge of the optic disc). A red-free stereoscopic pair is taken of Field 2 of each eye prior to the injection of the fluorescein dye. Next, the camera is positioned for Field 2 of the study or "transit" eye and fluorescein is injected rapidly, as a bolus, into the antecubital or other convenient vein according to standard clinic procedures. Stereo pairs of Field 2 are taken during the early transit phase (typically five to eight pairs taken between 15 and 45 seconds), at mid-phase (stereopairs of F2 and F1 at 60 to 90 seconds, and of F2 at two to three minutes) and finally at the late phase (one stereopair each at five and 10 minutes after injection). In the "non-transit" fellow eye, stereopairs are taken at approximately two and 10 minutes after injection (no attempt is made to capture the "transit" phase in the non-study eye).
• Image display: The display modalities are very different for film and digital images. Film-based angiograms are examined on a standardized light box utilizing a Donaldson stereoscopic viewer with 5X magnification or equivalent. Areas and distances of interest are measured by overlaying the images with a set of grids printed on transparency stock. Digital angiograms are evaluated on a calibrated 21-inch, high-resolution monitor using a handheld stereoscopic viewer (Stereo-Vu, PS Manufacturing,
Evaluation Procedure
Evaluation of FA in neovascular AMD involves side-by-side comparison of image pairs in various phases of the study. Quality images with good stereopsis are essential for accurate interpretation. The evaluation procedure may be approached in the following steps:
1. Evaluation of the CNV: angiographic subtypes.
2. Evaluation of the non-CNV lesion components of the neovascular complex.
3. Important measurements: total CNV area, total lesion area and leakage area.
4. Evaluation of abnormalities not considered part of the neovascular lesion complex.
Evaluation of the CNV
CNV is an ingrowth of neovascular tissue through a break in the outer aspect of Bruch's membrane from the choroid. Identification of CNV on FA is based on the leakage pattern in the various phases of the angiogram. Leakage is assessed by comparing early frames of FA to early-mid and late frames, e.g., in the series shown in Figure 2, the pre- injection, red-free, a 40-second frame, the two-minute frame and the 10-minute frame. The earliest frame where leakage starts defines the CNV lesion. Based on the time of appearance of leakage and the intensity of leakage, CNV has been divided into two main categories: classic and occult. Each CNV type is evaluated for presence, proximity to the center of the macula and area involved (estimated by using appropriate grids or digital planimetry tools). Leakage may continue to increase with time, the intensity depending on the subtype. The area of leakage is always assessed in the late phase. 
• Classic CNV: Typical Classic CNV is characterized by well-demarcated areas of intense hyperfluorescence appearing early and showing progressive leakage. The fluorescein tends to be most intense at the perimeter of the CNV; the center may show hypofluorescence. Leakage progresses into the late phase of the angiogram, and usually obscures the boundaries of the CNV (See Figure 2). Classic description of visible subretinal vascular network (a lacy network) is seen in a minority of eyes with AMD. A variant of classic CNV called atypical classic consists of CNV with leakage that is not as intense as the typical type and starts in the early-mid phase of the FA (See Figure 3). Sometimes atypical classic has a greater component of fibrosis than typical classic and may be an intermediate stage of regression from typical CNV to fibrosis. 
The size (area) of a classic lesion is measured from the earliest frame where the leakage begins, before it becomes intense and the demarcation of the boundaries is lost. For extra- or juxtafoveal lesions, proximity of the CNV from the center of the macula is also identified from the same frame.
• Occult CNV: The appearance of occult CNV varies widely and can be difficult to identify. The MPS identifies two subtypes of the occult category: fibrovascular pigment epithelial detachment (FV-PED) and late leakage of undetermined source (LLUS).
FV-PED is identified by ill-defined areas of irregular elevation of the staining/leaking RPE with "stipples" of hyperfluorescence often intermixed on the surface (See Figure 4). Good stereoscopic effect is essential to determine the presence of FV-PED. The lesion size is usually measured in early-mid phase.
LLUS is a rare type of occult CNV in which poorly demarcated areas of leakage appear at the level of the RPE in the late phase of the angiogram. There are no abnormalities discernible in either the early or mid phase that account for the leakage. Lesion size and leakage area are the same and are both measured from the late phase. A third type of occult CNV, called "occult other," is not identified as part of the MPS protocol and includes CNV that has an appearance similar to that of FV-PED, but without elevation.
Angiographic Subtypes of CNV
In eyes with a combination of CNV, three angiographic subtypes are identified:
1. Classic subtype (See Figure 2) has classic components >50 percent of the total lesion area.
2. Minimally classic has 1 to 50 percent (See Figure 6) of the total lesion area comprising a classic subtype.
3. Occult with no classic has no classic component in it (See Figure 4).
At some reading centers an alternative definition of classic and minimally classic CNV is employed. A lesion is classic if the CNV occupies more than 50 percent of the total CNV area (which may be less than 50 percent of the total lesion area), and minimally classic is also based upon the proportion of the total CNV area occupied by classic. 
Type 3 CNV or RAP
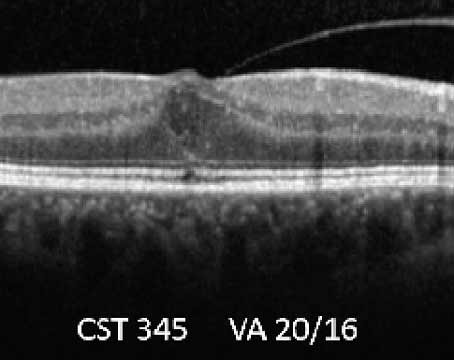
A specific subtype of CNV, Retinal Angiomatous Proliferation or RAP, features abnormal retinal vascular connections to subretinal CNV.4 Current thinking is that the primary origin of the subretinal CNV is from the choroid. A combination of features such as superficial intraretinal hemorrhages, intraretinal leakage (hot spot), cystoid spaces, serous PED and retinal anastamosis guide the diagnosis of RAP. RAP could occur in combination with other angiographic subtypes.
Non-CNV Components
An assortment of components is considered to constitute the neovascular lesion complex. Lesion components obscure the borders of the CNV and interfere with the ability to judge how far CNV extends. These include thick blood, elevated blocked fluorescence, and serous detachments of the RPE. Other lesions that occur during the follow-up of CNV such as fibrous or disciform scar, atrophic scar and RPE rips are also considered lesion components (though the MPS protocol did not include them). Many clinical trial protocols specifically exclude subjects with either too many non-CNV components and with non-CNV components under the fovea.
• Elevated blocked fluorescence. (See Figure 6) This is hypofluorescence that is contiguous with and blocks the border of the CNV. Hyperplastic pigment or fibrous tissue can present with blocked fluorescence that is usually elevated above the RPE. Very proteinaceous, turbid fluid may be a cause. Often, a correlation to blocked fluorescence on FA with clinical examination or color photos shows no visible lesion.
• Blood. Contiguous subretinal or sub-RPE blood that is thick enough to obscure a boundary of the CNV is considered part of the complex (See Figure 7).
• Serous pigment epithelial detachment. S-PED appears as a uniform and often circular elevation of the RPE that has uniform pooling of fluorescein dye in the late phase (See Figure 8). S-PEDs tend to start pooling in very early phase and have a smooth contour surface with a semi-circular dome-shape. Pooling of dye and staining due to S-PEDs is not included as part of leakage.
• Other lesion components. Fibrous tissue, disciform scars (See Figure 9) and atrophic scars (See Figure 10) and RPE rips or tears (See Figure 11) are lesions seen on follow-up of CNV and are considered to be part of the lesion if they obscure the borders of the CNV.
Important Measurements on FA
There are three main efficacy measurements derived from FA that are used for clinical trials of neovascular AMD: total lesion area, total CNV area and leakage area. Clinical trials may specify a range of total lesion area for eligibility. The change in total lesion area, total CNV area, and leakage area over time are important morphology endpoints in clinical trials.
• Total lesion area is the sum of total CNV area and the areas of each of the non-CNV lesion components. The total CNV area is calculated by defining the boundaries of the CNV and is measured from the image where the CNV first appears. For classic lesions, this is the early phase and for occult, the early-mid phase. The greatest linear dimension (GLD) of the lesion is derived from the total CNV area and not the total lesion area.
• Fluorescein leakage area is a key feature of CNV and thus detection of its onset and evaluation of its course across the phases of an angiogram are important.
• Total area of leakage (for all CNV combined, if there is more than one type) is measured from the late frames of the angiogram. Fluorescein staining of the RPE, CNV or other structures is hyperfluorescence that may change in intensity but does not lose its sharp outlines. The distinction between mild leakage and staining is highly subjective and may be quite variable between clinicians. Leakage area does not always match total lesion area or total CNV area. Inactive, fibrotic lesions may have staining but little leakage, yielding a leakage area much smaller than the total lesion area. Conversely, an aggressive classic CNV lesion may have leakage area extending beyond the margins of the lesion with a greater measurement than that of the total lesion.
Figure 12 demonstrates an active classic CNV with an area of blocked fluorescence around it. The CNV area alone is delineated with green to obtain the total CNV area and the greatest linear dimension is obtained from this area. The area of blocked fluorescence (lesion component) is included to assess the total lesion area. Both of these measurements are obtained in early phase of the FA. Leakage area is assessed in the late phase of the FA.
To summarize, angiographic evaluation is important to determine eligibility and to follow patients in clinical trials of neovascular AMD. A neovascular complex can be differentiated on FA into CNV and non-CNV components. CNV is identified as classic or occult based on the time of appearance and intensity of leakage from the CNV; classic lesions appear early, are well-defined and leak intensely, while occult CNV lesions appear in early-mid phase, leak less intensely and are ill-defined. Non-CNV components include elevated blocked fluorescence, thick blood and serous PEDs, all contiguous to the CNV. The sum of the total CNV area and the area of the non-CNV lesion components gives the total lesion area.
Dr. Domalpally is co-director of the
1. Macular Photocoagulation Study Group.Subfoveal neovascular lesions in age-related macular degeneration. Guidelines for evaluation and treatment in the macular photocoagulation study. Arch Ophthalmol 1991;109:1242-57.
2. Bressler NM, Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: Two-year results of 2 randomized clinical trials--TAP report 2. Arch Ophthalmol 2001;119:198-207.
3. Group ETDRSR. Classification of diabetic retinopathy from fluorescein angiograms. ETDRS report number 11. Ophthalmology 1991;98:807-22.
4. Yannuzzi LA, Freund KB, Takahashi BS. Review of retinal angiomatous proliferation or type 3 neovascularization. Retina 2008;28:375-84.