The Symfony
This IOL, a toric version of which was also approved, is the first in a new category of implants dubbed extended depth of focus lenses. Here's how to get the most from it:
• Best candidates. Sioux City, Iowa, surgeon Jason Jones, who participated in the Symfony’s FDA trial, says the best candidate “is someone who desires reduced spectacle dependence but is also willing to pay for that privilege,” he says. “He also wants to enjoy a high quality of vision and, lastly, he has to accept the use of glasses for occasional needs, specifically for reading, or for reading for long periods of time, for fine print, et cetera.” In the FDA study, 85 percent of the Symfony patients reported wearing correction a “little or none of the time” vs. 60 percent of monofocal IOL controls.
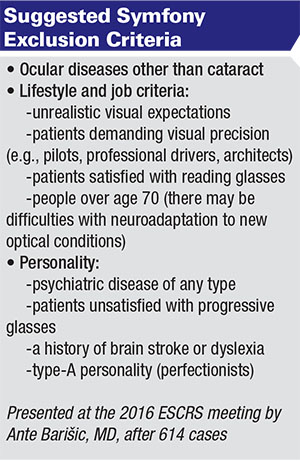 |
Surgeons say the preop discussion with Symfony candidates is also a good time to manage their expectations in terms of qualitative vision issues. “The other thing patients should be made aware of is that there will be some halo formation and perhaps some glare symptoms,” Dr. Jones says. “It’s a very low rate, much lower than what has been reported in FDA trials for multifocal lenses, but it’s still present. And, if your patient has such an experience and wasn’t prepared for it preop, sometimes he’ll find that his experience isn’t very acceptable. It’s one of those things that, if you make them aware of it but they don’t have it, all is good. But if they do, it’s often manageable with encouragement. My patients from the study, some of whom I have more than a year of follow-up on, actually report to me that they rarely notice glare and halo issues anymore.”
Dean Corbett, BSc, MBChB, FRANZCO, who has extensive experience with the Symfony, says the halos and starbursts are there, but “the amount of trouble people have with them is vastly less.” He says he equates them to more of a “soft” dysphotopsia, as opposed to a “hard” one, meaning they’re better tolerated as a group. “In my experience,” he says, “between 30 and 50 percent of patients have no more symptoms than they’d have with a monofocal, but the remaining group will see night-vision disturbances. However, it’s much less common to get a patient who is bothered by them.”
• Choose a refractive target. Adjusting the eye’s final refractive target can help the lens work with patients’ needs, surgeons say. “That’s the fun thing about the use of this lens,” says Dr. Corbett. “It opens up a new approach for a surgeon trying to deliver a visual outcome to patients. One decides with the patient what the emphasis of visual performance is going to be. For instance, if the patient hunts, shoots or is a golfer and is passionate about having distance focus and isn’t overly discerning about his near vision, I would put a Symfony lens in and target the ‘first or second plus’ on the IOLMaster or Lenstar [referring to the first and second IOL options in the hyperopic range when these devices are programmed to target emmetropia]. Then, on the basis of the refractive outcome of the first eye, we determine what he wants for the second eye. In another patient, say an office worker who doesn’t undertake any leisure activities that require distance acuity, we’d be inclined to choose the ‘first minus’ [on a biometry device]—or even the ‘second minus’ if it’s a low myope, because low myopes have traditionally been in glasses that have often undercorrected their distance vision. The patient’s two lenses will overlap at 90 percent of the range of vision, but we can just give one eye some extra power over the other, at either end of the spectrum. When we see the patients after a week, one in five will say, ‘It’s perfect,’ and I’ll put the same refractive-targeted lens in the other eye. But, more often than not, I’ll be choosing a lens either on the plus side or the minus side, depending on what the patient wants.” Investigators say this targeting is possible because vision doesn’t drop off as fast with defocus as a monofocal IOL does.
Dr. Jones says that, in addition to the technique of targeting the non-dominant Symfony eye for some minus in patients with strong reading needs—he says the general consensus is that -0.5 is the most surgeons will target in this way—some Symfony surgeons are also doing a “mix-and-match” approach to get certain patients the near point they want. “Some surgeons have tried to boost the reading range of this lens by pairing it with a multifocal lens, specifically the Tecnis ZLB00, though I’ve heard of the ZKB00 being used, as well,” he says. “Those lenses deliver a definitive near focusing point, as multifocal lenses do. In my experience, however, even using the low-add multifocals from Abbott, there are some halo issues. However, from the reports I’ve heard, the halos are different than the Symfony’s; multifocal lenses have a more distinct ring structure, and the Symfony's tends to be softer, less intrusive. With appropriate counseling, a mix between the two technologies is reasonable.”
In terms of refraction, one thing surgeons say to be aware of with the Symfony is that, after implantation, auto-refractors will give unusual results. “The auto-refractor will always come up with minus,” Dr. Corbett notes. “You can either ask the patient what his vision’s like or, if you’re more scientific, you can do a refraction and push the plus.”
The Raindrop
The Raindrop corneal inlay has no refractive power of its own, but when placed beneath a flap in a patient’s non-dominant eye, it changes the cornea’s refractive power to boost near vision. Here are surgeons’ tips for using it:
• Preop considerations. Jeffrey Whitman, MD, a Dallas surgeon who participated in the FDA trial of the inlay, says the contraindications are similar to those for LASIK. “The topography should be good, the tear film acceptable—dry eye is a problem for this just as it’s a problem for LASIK,” he says. “Unrealistic expectations are a contraindication, too. In terms of baseline refractive error, within the FDA parameters we’re looking for patients who are +1 to -0.5 D spherical equivalent, with 0.75 D or less of cylinder. This is because the procedure treats a little hyperopia. In Europe, though, where they usually do LASIK on these patients as well, they usually shoot for an endpoint of +0.25 to +0.5 D before they put the inlay in.” Also, there should be 300 µm of stroma remaining below the flap, notes Dr. Whitman.
• The surgery. Dr. Whitman says the flap for the Raindrop is made at 30 percent corneal depth. Flaps are usually thicker than those used in LASIK, about 150 µm on average. “Disregarding this and going for a thin flap will result in failure and removal of the inlay due to a high rate of inflammatory response,” he says. Review’s Refractive Surgery editor, Arturo Chayet, MD, of Tijuana, Mexico, errs on the side of thicker flaps. “I recommend using at least 150-µm flaps,” he says. “You don’t want to be close to the surface because you may get corneal haze.”
Dr. Chayet implants the Raindrop under the Allegretto excimer laser’s microscope. “I activate the HeNe beam, which allows the pupil to dilate a little more and provides retro-illumination to center the lens better,” he says.
Once the flap is made, the surgeon reflects it back and loads the inlay onto its delivery instrument. “It has to be just wet enough—not too wet,” notes Dr. Whitman. “You then lay the tip of the delivery instrument just beyond the center of the light-constricted pupil. There are a number of instruments you can use to manipulate the Raindrop, but I use the elbow of a Sinskey hook. I push down on the inlay as I pull away the delivery device. The trick is doing this so you leave it as close to the center of the pupil as possible. While the inlay is still wet, you can use your instrument to slightly tap it in one direction or another and get it centered.”
Hydration now becomes crucial, says Dr. Whitman. “At this point, when you’ve placed the inlay, wait a minute to a minute-and-a-half to allow the Raindrop to dry,” he explains. “The endothelial pump pulls fluid through the cornea and the inlay—and you’ll see the Raindrop start to dimple like the skin of an orange as it dries. You know that it’s stuck down properly when it’s fairly dimpled. While that’s occurring, since we are leaving the flap open longer than we typically do for LASIK, it’s important to keep the stromal side of the flap and the area around the inlay moist. This is for striae avoidance. I re-wet the stromal side of the flap every 20 seconds or so, and I also gently re-wet the cut stromal side but take care not to rewet the inlay itself. If you re-wet the inlay, it can float, requiring you to restart the drying period.”
Dr. Whitman says that once you’ve achieved dimpling of the inlay, you replace the flap. “Again, unlike LASIK, you can’t go back under the flap and irrigate back and forth because you’ll perhaps irrigate off the inlay,” he warns. “Once it’s laid back, just irrigate and smooth the epithelial surface of the flap, then wait a minute or two for it to dry. Once the area’s dry, let the patient sit for 10 to 15 minutes, and then look at the eye at the slit lamp to ensure the inlay looks well-centered. Fortunately, the inlay can tolerate about 0.7 mm of decentration and still function fine.”
• Postop notes. The postop period is focused on catching any immune response. “We place the patient on a Durezol tapering dose for a month,” says Dr. Whitman. “Then, once that month has passed, we put him on Lotemax for a two-month taper. We’ve found that cutting the steroid dose short can lead to an inflammatory response, fibrosis and possible removal of the inlay down the line. That full three months of steroids postop is very important. We also put him on an antibiotic drop for a week.”
The patients are seen at a day, a week, a month and then every three months for the first year, looking for signs of inflammation or fibrosis. “Inflammation will often cause a decrease in distance vision, an increase in near vision and a steepening of the cornea,” Dr. Whitman explains. “If we see either inflammation or fibrosis, we immediately start a one-month course of tapering Durezol, and we may do a taper of Lotemax after that. This got rid of it in a majority of cases in the study. We were allowed to do this regimen three times in the study before having to remove the inlay, which we’ll probably do in commercial practice, too. As part of the preop discussion, we tell patients that if removal is indicated, their vision will go back to close to where it was preop—we never say the term ‘reversible.’ ” REVIEW
Drs. Jones and Corbett have received compensation/speaker’s fees from AMO. Drs. Whitman and Chayet are clinical investigators for ReVision Optics.