Glaucoma surgery is always evolving. One of the ways it’s changed in recent years is that more surgeons have begun using glues and sealants instead of sutures to close wounds and cover tubes during surgery. However, it’s become a part of glaucoma surgical dogma that when performing surgery, sutures should be accepted as the standard of care. That may be part of the reason many surgeons have been hesitant to switch to glues and sealants. If suturing works, why switch to a different approach?
Here, I’d like to share some of my experience moving from sutures to glues when performing tube shunt surgery, and explain why I believe it’s an option every glaucoma surgeon should consider.
Pros and Cons
If you take a step back, you’ll see that sutures have some limitations. In fact, in some situations, sutures can be sub-optimal and even dangerous. To take a stitch, you have to pierce the skin, or cornea or sclera, causing a small amount of damage—that’s how sutures maintain purchase. Doing so causes inflammation and often causes bleeding, and it creates a nidus for infection. Sutures can also cause the patient to have a foreign-body sensation postop.
Now that I’ve been performing tube shunt surgery using glue instead of stitches for several years, I can list several advantages to using glue in this situation, beyond just avoiding infection:
• Less time in the OR. In my experience, using glue to complete this type of surgery saves operating room time. In addition to efficiency, that’s important for patient safety because a shorter surgery is often a safer surgery. The longer someone is in surgery, the higher the probability of something unintended happening.
• Patients are more comfortable postoperatively. In addition, their eyes look whiter and quieter sooner.
• Using glue reduces the need for postoperative steroids. I’ve found that eyes that have been glued have a lower requirement for postoperative steroid. The patients are comfortable because there’s no foreign body reaction associated with glue. In contrast, vicryl sutures are pro-inflammatory, which will cause you to use more steroid.
• Complications and reoperation rates are similar to those of sutured surgery. We recently published a retrospective case series study designed to evaluate the safety and efficacy profile of 122 Ahmed glaucoma valve implantations in 99 patients performed using Tisseel fibrin sealant instead of sutures.1 Eighteen eyes received the tube only; 46 also underwent cataract extraction; 35 had adjunctive endoscopic cyclophotocoagulation; and 23 had the valve with cataract surgery and ECP. The rates of re-operation and com-plications in our study were very similar to (if not lower than) those seen in other studies such as the Ahmed Baerveldt Comparison study and the Ahmed vs. Baerveldt study, which involved surgeries done using sutures.
• Glue rarely fails unexpectedly. If all of the construction is done appropriately, you won’t need to be re-operating because of glue failure. I’ve seen that happen once or twice—but I’ve also seen that happen with sutured wounds. I don’t think there’s a big difference in this respect, especially if you follow all of the suggestions I’ve outlined below.
Limitations of this approach would include:
• Cost. Sutures are sometimes (but not always) less expensive than glue. Ultimately, the cost will depend on which suture material is being used and how your facility handles the purchase of glue.
It’s definitely important for the surgeon to have a sense of how much the ASC or OR is paying and getting reimbursed for glue—as well as any other surgical tools being used. You should work within those parameters and do whatever makes the most sense in that situation.
• Applying glue requires work-ing quickly. Because glue will hard-en, timing matters. That’s not an issue when using stitches.
• Glue may not work in every situation. For example, it won’t work if the wound is under tension; sutures may have a greater tensile strength. If you do use glue and it doesn’t work, you’ll have to add a stitch or two, making twice the work.
• The patient may be able to feel the presence of the glue on the ocular surface. This is possible; however, sutures will always be more irritating than glue.
• There’s a small learning curve. The doctor and technician both need to become accustomed to mixing and applying the glue during surgery. However, there are only a few basic rules for application and appropriate wound design, so any surgeon should be able to switch from stitches to glue with minimal trial and error.
Some surgeons may feel more comfortable using sutures for certain parts of drainage implant surgery—e.g., attachment of the plate to sclera—while readily adopting glue for other parts of the procedure. (This may be especially true while they’re transitioning to the use of glue.) A “hybrid approach” combining glue and sutures is certainly acceptable.
 |
My Technique
About seven years ago I began converting my Ahmed valve surgeries, and to some extent my Baerveldt surgeries, into sutureless surgeries. (The reason I use this approach more with my Ahmed valve surgeries is that implanting a Baerveldt shunt—as well as the new Ahmed ClearPath device—requires a 7-0 vicryl suture to ligate the tube, so you’re already using one stitch.)
In traditional tube shunt surgery we place a significant number of sutures—usually two stitches to hold the plate to the sclera; two more stitches to hold the tube to the sclera; in many cases four stitches to anchor a patch graft around the tube entry site; and then several more stitches to close the conjunctiva. This is time-consuming, and as noted, the material used for stitching is a foreign body; that creates additional inflammation beyond what’s caused by the surgery itself.
In my sutureless surgery I primarily use two types of glue, which work similarly: Tisseel fibrin glue (Baxter Healthcare) and ReSure ocular sealant (Ocular Therapeutix), a polyethylene glycol hydrogel. Using either one involves mixing two solutions that interact to form the glue. This is generally done right on the tissue that needs to be glued, and right at the time of application to the tissue. In my experience, both products work equally well; cost concerns and/or surgeon preference may influence which one is used in a given practice or situation.
 |
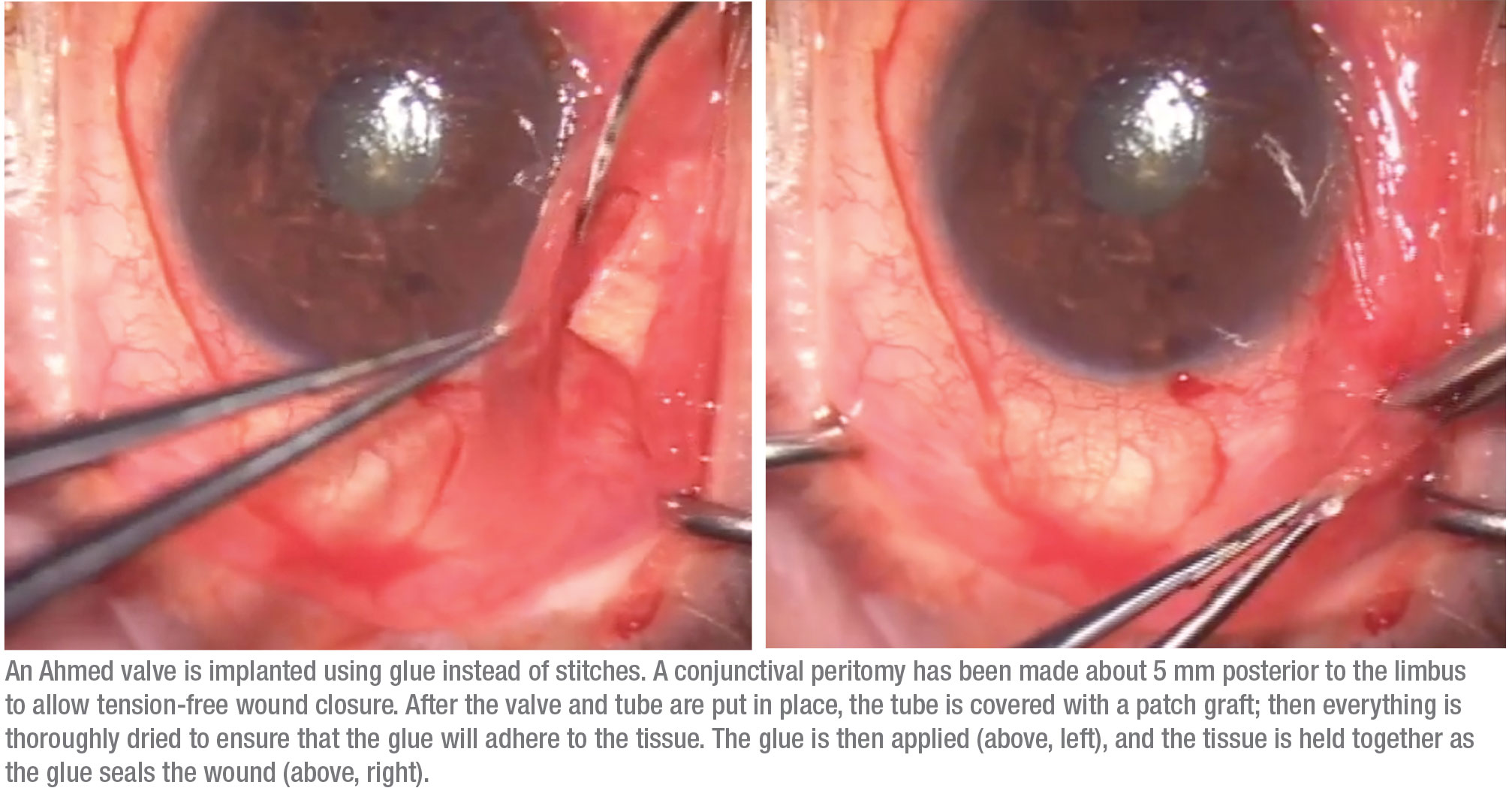
Part of a successful sutureless surgery involves using a different wound construction to allow the ocular tissue to retain these implants. When implanting the Ahmed shunt I first make a conjunctival peritomy about 5 mm posterior to the limbus. That positioning allows tension-free wound closure. (Glue may fail to hold the tissues together if they’re under significant tension that’s trying to pull them apart.)
Second, I place the valve very posteriorly; then I gently tug on the tube to make sure that the plate is sitting comfortably behind the equator.
Third, I get the tube to stay put against the sclera by making a long, 4- to 5-mm scleral tunnel using the 23-ga. needle. This holds the tube in place, keeping the tube tip from sliding or moving.
Fourth, I lay a patch graft over the tube, where it will be glued in place. I position it so it sits below the conjunctival incision, which will help with closure. I then glue all of that together in one pass. The glue dissolves without incident over the first postoperative week.
You can see me using this technique on YouTube at youtube.com/watch?v=rTr5QhBZMMc.
| Glues do a nice job of holding tissues together, but they can’t withstand a tremendous amount of pulling on the tissue. If you still end up with tension on the wound, you may need to |
Strategies for Success
To help prevent any missteps when adopting this approach to tube shunt implantation, keep these strategies in mind:
• Glues work best on dry tissue. Glue will fail if the tissue is very wet. So, if you have a patient who is bleeding a lot, or a surgical wound that’s leaking aqueous, you’ll need to temporarily stop the flow of aqueous or blood. If you can dry the tissue and apply the glue in a controlled setting, it should work well.
• Avoid wound construction that will leave the wound under a lot of tension. As noted, glues do a nice job of holding tissues together, but they can’t withstand a tremendous amount of pulling on the tissue. To reduce tension on the wound, I don’t make the incision at the limbus. Instead, I make the incision about 5 mm posterior to the limbus, where my patch graft will be placed. If you still end up with tension on the wound, you may need to add a stitch.
• If you have concerns, err on the conservative side and add a stitch. Generally, it’s OK to be cautious and suture if you have any doubts about the security of the glued tissues (well-founded or otherwise). If you apply too much glue, you can trim the glue with a Westcott scissor.
• Eye rubbing may not be a contraindication. If the patient is a known eye-rubber, you might think it would be a bad idea to use glue. However, I’m not sure that’s true, because patients tend to rub the eye more when there’s a stitch, thanks to the foreign body sensation. Performing the surgery in a way that reduces the foreign body sensation may actually cause less postoperative eye rubbing. Use your judgment, and try to understand why the patient is rubbing the eye.
Taking advantage of the benefits of working with glue, I’ve personally done more than 1,000 sutureless Ahmed valves, and I continue to do them to this day. REVIEW
Dr. Radcliffe is a clinical associate professor at NY Eye and Ear Infir-mary, and practices at the New York Eye Surgery Center. He is a consultant to Ocular Therapeutix and New World Medical.
1. Pham CN, Radcliffe NM, Vu DM. Surgical outcomes associated with a sutureless drainage valve implantation procedure in patients with refractory glaucoma. Clin Ophthalmol 2018;12:2607-2615.



