LASIK Xtra Protocol
Since LASIK slightly weakens even normal corneas, surgeons wondered if they could enhance the procedure’s safety and stability by combining it with a brief corneal cross-linking treatment, and the technique called LASIK Xtra was born. Initial studies were performed by Athens, Greece, surgeon John Kanellopoulos, but other surgeons around the world soon followed suit.
Dr. Kanellopoulos describes his approach to myopic eyes: “I add cross-linking in myopic eyes that are at higher risk for ectasia,” he says. “These are patients younger than 30, have myopia greater than -6 D, high astigmatism or astigmatism that’s asymmetric between the two eyes—but not forme fruste keratoconus—or who will have a residual stromal bed under 300 µm after the LASIK.” He uses the technique in all hyperopic LASIK cases.
 |
| Surgeons continue to work with new applications for corneal cross-linking. |
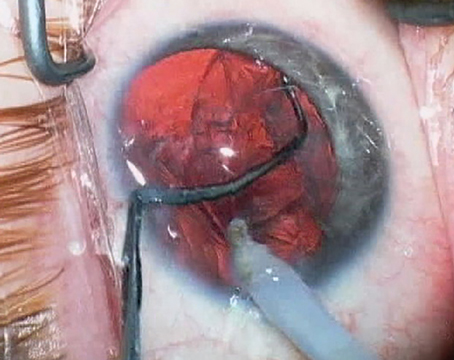
The typical protocol involves performing the LASIK procedure and then, with the flap still reflected back, applying a certain amount of riboflavin (which varies by surgeon) onto the stromal bed and letting it soak in. Then, the surgeon washes away the riboflavin, replaces the flap and irradiates the cornea with UV light (the duration and intensity of which also varies by practitioner). Dr. Kanellopoulos explains that he soaks the bed with Avedro’s VibeX Rapid (saline-based, 0.1% riboflavin) for 60 seconds, “taking special care not to expose the folded flap to riboflavin,” then wipes away the excess riboflavin with a dry sponge before repositioning the flap and exposing the eye to 30 mW/cm2 of UV light for 80 seconds. For hyperopic LASIK Xtra, the soak is the same, but he irradiates the eye for one minute rather than 80 seconds.
Singapore’s Jerry Tan, MD, was one of the first surgeons to embrace LASIK Xtra after Dr. Kanellopoulos described it. Dr. Tan started off slowly but now uses LASIK Xtra on all patients who are candidates for LASIK. Dr. Tan says the first stumbling block in his learning curve is also the reason doctors in the United States can’t—or shouldn’t—do LASIK Xtra at the moment. “When I started doing LASIK Xtra, I used riboflavin with Dextran, and it caused a lot of diffuse lamellar keratitis,” he warns. “You mustn’t use riboflavin with Dextran.” Instead, he now uses riboflavin with saline (0.25% Riboflavin-5-Phosphate, Saline), which has yet to be approved in the United States; only riboflavin with Dextran is currently sold here.
“I initially did LASIK Xtra because John Marshall, MD, told me that, by his calculations, it should double the strength of the postop LASIK cornea,” Dr. Tan continues. “Regular cross-linking with the Dresden Protocol, with 30 minutes of riboflavin soaking and 30 minutes of UV irradiance of 3 mW/cm2, will make it 3.5 times stronger. For LASIK Xtra, though, we just want it to be a little bit stronger; we don’t need it to be like a rock as it is after a keratoconus treatment.” Dr. Tan’s LASIK Xtra protocol consists of a 45-second soak and a 45-second irradiation with 13 mW/cm2.
“I started performing LASIK Xtra on my high myopes because they require a lot of tissue to be removed,” Dr. Tan explains. “I began on patients -8 D and above, and actually found the results to be superior to my -6 and
-8 D LASIK results without combined cross-linking, so I began doing LASIK Xtra for patients -6 D and above. I then compared those patients to my LASIK-only patients between -4 and -6 D, and LASIK Xtra again showed slightly better results. As a result, I then decided that I might as well use LASIK Xtra on everyone.”
Bogota, Colombia, surgeon Gustavo Tamayo also uses LASIK Xtra on a lot of patients, but is more selective. “We have some indications for its use, mainly high myopes or hyperopes who have normal corneas with no signs of ectasia,” Dr. Tamayo explains. “We also use it in patients under 22 years old, or in patients whose corneas are completely normal but whose families have a history of keratoconus. However, in any patient in whom we suspect there’s a possibility of developing keratoconus or postop ectasia based on the Randleman score or any other table or index, we don’t recommend the use of LASIK Xtra. Instead, we’d advise surgeons to use LASEK or surface ablation and not put the patient at risk.”
The Results
In addition to acting as a hedge against future ectasia, surgeons say the other goal of the procedure is to help decrease regression of LASIK’s effect.
In a study of 155 consecutive eyes planned for myopic LASIK, Dr. Kanellopoulos and his colleagues treated 73 with LASIK Xtra (Group A) and 82 with stand-alone LASIK (Group B). At one-year postop, 90 percent of Group A patients saw 20/20 or better uncorrected vs. 85 percent of the patients in Group B (p=0.042).1 The researchers reported that, at one year, the manifest spherical equivalent in Group A was -0.19 D, compared to -0.27 D in Group B, indicating a reduced refractive shift in the LASIK+CXL group (p=0.063). They go on to say that in the LASIK-only group there was a slight positive slope in the K readings, both in the flat and steep meridians, “suggestive of mild progressive corneal steepening,” but there wasn’t such a trend in the combined-procedures group.
The researchers caution, however, that cross-linking in other scenarios has demonstrated a propensity for progressive corneal flattening. They note that LASIK Xtra differs from the cross-linking used in these other scenarios in two key ways: The other corneas were fundamentally unstable (ectatic), while LASIK Xtra is performed in healthy corneas; and keratoconus cases receive the “full-energy” treatment, while LASIK Xtra cases only get a “partial-energy” treatment, which amounts to less than half the energy of the standard protocol.1 They acknowledge that further long-term studies are necessary to evaluate this flattening effect.
Dr. Tamayo says that, even though he’s seen positive results with LASIK Xtra, “We really need more time to prove that it works; we don’t have enough follow-up time to make sure that we’ve definitely stopped the development of ectasia in these patients.” He says lack of knowledge of the procedure’s limitations is a potential drawback. “One of the biggest problems occurs when the general ophthalmologist, without enough knowledge, believes he can do LASIK Xtra in a keratoconus patient or a patient at risk for ectasia,” he says.
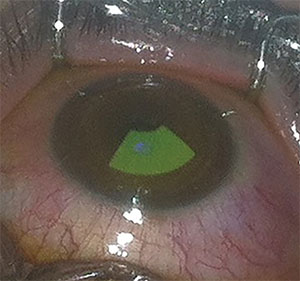
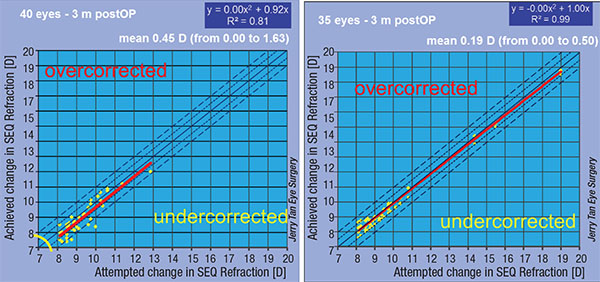 |
| Singapore’s Jerry Tan says that LASIK+cross-linking (right) in patients -8 D and above yielded results with less scatter than LASIK alone (left) in his practice. |
One of the benefits however, Dr. Tamayo says, is that cross-linking has blended seamlessly with his LASIK. “The important fact is we’ve proved it doesn’t change the LASIK nomogram,” he explains. “It doesn’t change the final result. It also doesn’t require you to change your LASIK protocol.
“So far, though I only have three years of follow-up, my results have been very stable,” Dr. Tamayo continues. “I don’t have a high complication rate, but there are a few I want to mention: First, one of my main complications is dryness. Dry eye remains for a longer time in LASIK Xtra than in LASIK-only patients. Therefore, I explain to my patients that they’ll need a little more time to overcome the dryness compared to regular LASIK. A second complication I’ve seen is increased light sensitivity after the LASIK Xtra treatment, lasting for three to four months. Sometimes I keep these patients on steroids for a longer time than the regular LASIK patients. With normal LASIK, I keep them on a steroid regimen for one to two weeks. But I keep LASIK Xtra patients on steroids for a month—sometimes a couple of months—until the photosensitivity resolves.”
Based on his current knowledge of LASIK Xtra, Dr. Tamayo sees a future indication for the procedure: LASIK candidates with allergy. “Lately, I’ve been doing it in patients with allergic conjunctivitis,” he says, “because they’re more prone to rubbing their eyes. So, in patients with a history of eye-rubbing, I now do LASIK Xtra—in addition to advising them to not rub their eyes, of course. Ultimately, I don’t think we’ll use it in all our patients, but there are cases such as deeper ablations, thin corneas and high myopes in whom we’re hesitant to use surface ablation in which we can perform LASIK Xtra very safely, and avoid the hassle of recovery time, corneal haze and the like.” REVIEW
Dr. Kanellopoulos has been a consultant for Avedro and Dr. Tamayo is on Avedro’s medical advisory board. Dr. Tan has no financial interest in any of the products mentioned.
1. Kanellopoulos AJ, Asimellis G, Karabatsas C. Comparison of prophylactic higher fluence corneal cross-linking to control, in myopic LASIK, one year results. Clin Ophthalmol 2014;27;8:2373.