Other than monovision LASIK, there are few extraocular surgical treatments for presbyopia that are squarely in the mainstream in the United States, though surgeons continue to search for them. Along these lines, companies have been hard at work attempting to create corneal inlays that could help patients see better at near without losing too much vision at other distances. Here is an update on two of the inlays that are currently being used or investigated for approval.
AcuFocus Kamra
 |
The Kamra inlay is a monocularly implanted disk with a central hole that enhances vision based on the pinhole effect. “In the current trial, the inlay is 5-µm thick, matte black, with a 1.6 mm central diameter and a 3.8 mm outer diameter,” says Indianapolis surgeon and Kamra investigator Kevin Waltz. “There are approximately 8,400 fenestrations in the face of the material in a pseudo-randomized pattern. This amounts to the pattern having very few holes close to the edge and relatively many holes toward the center, giving a significant increase in the flow of nutrients. The holes are between 5 and 11 µm in size and don’t have any optical effect. Since the holes occupy 9 percent of the surface area of the device, most of the device is opaque to light but relatively transparent to nutrients.” Currently, the Kamra inlay is implanted in the cornea at a depth of 200 µm beneath a LASIK-style flap or inside a corneal pocket. “The flap opens up the potential for LASIK in addition to the inlay,” explains Kamra investigator John Vukich, MD, of Madison, Wis. “Currently, surgeons in countries where the inlay is approved are performing a LASIK pretreatment of existing refractive error.” In the United States, the device is only being studied in emmetropic presbyopes.
“The Kamra is designed to give better distance, intermediate and near vision based on the pinhole’s depth-of-focus effect,” says Dr. Waltz. “The depth-of-field effect is about 2.5 D, and gives an approximation of accommodation.”
In practice, when implanting the Kamra, centration is key. “We initially thought that being within a couple hundred microns of the center of the visual axis would be ‘close enough,’ but it wasn’t,” says Dr. Waltz. “We’ve found that placing the Kamra’s aperture over the center of the axis is critical. For proper centration, we now use a device made by the SMI Corp. that images the visual axis, iris and the anterior segment and displays the relationship of all those factors to each other digitally.” Dr. Waltz estimates that the SMI device costs between $25,000 and $30,000.
“We only had a handful that required recentration during the study,” says Dr. Vukich. “Frankly, some of them were facilitated by our understanding of the disparity between the first Purkinje image, the visual axis and pupil opposition that we gained by using the SMI heads-up display device.” Dr. Waltz says the device usually doesn’t migrate after surgery, but, if a decentration does occur, it’s decentered during implantation. “It’s usually not something that happens a day or two later,” he says. “Once it’s sitting somewhere, that’s where it stays. In my patients in the trial, without the SMI device, I had to go back and recenter it between 5 and 10 percent of the time. With the SMI device you’re able to tell immediately if you need to recenter it.” The inlay is also very fragile. “Since it’s only 5 µm thick, you can destroy it easily,” says Dr. Waltz. “It’s easy to drop and let go of inadvertently. You have to be gentle when working with it.”
In a study conducted outside of the United States, in the 243 eyes available to follow-up at 18 months, the average uncorrected near acuity in the implanted eye is a little better than J3 (they saw an average of J8 preop). In the same group, the average uncorrected distance acuity in that eye is just below 20/20, which is a slight decrease from a baseline average in these emmetropes that was better than 20/20.
Dr. Waltz says the patients in the U.S. trial, who number a little more than 500, will reach the two-year follow-up point in the next six months, and the company may submit its application for approval early in 2012.
Flexivue Microlens
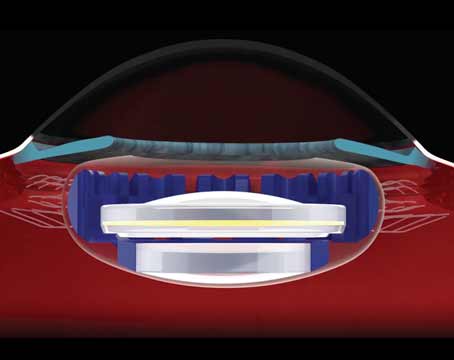
The Microlens is a 3.2-mm disk that is implanted 300 µm deep in a corneal pocket in a patient’s non-dominant eye. It has no power in the central 0.4 mm but has a power ranging from +1.5 to +3.5 D in the periphery in 0.5-D increments. “It reinforces the theory that the central visual axis must be respected to produce good distance visual acuity,” says Bogota, Colombia, surgeon and Microlens researcher Gustavo Tamayo.
“We advise all Microlens users to do a monovision trial in a patient before implanting the lens,” explains Dr. Tamayo. “But the trial has to be with a low-power contact lens, maybe 1.25 to 1.5 D in one eye at the most, because the difference between the two eyes with the Microlens isn’t very much at six months postop. The patient has to have a somewhat easygoing personality, and be someone who can accept a little bit of loss of distance vision in one eye for a gain in his near vision. The implanted eye’s distance vision will be around 20/30 or 20/25, while the fellow will be 20/20 or 20/15.”
To implant the lens, surgeons currently use a femtosecond laser. “We create the corneal pocket with an IntraLase iFS 150,” says Dr. Tamayo. To generate just a pocket and not an entire flap, the surgeon places a mask over the laser cone. The mask blocks some of the beam, preventing the femtosecond laser from going to certain areas of the cornea and allowing it to make the pocket shape the surgeon needs. “The pocket is a kind of flap,” says Dr. Tamayo. “It has a border where you can dissect it open. The surgeon then places an inserter, containing the inlay, into the pocket and slowly releases the Microlens as he extracts the inserter. We center the inlay with the Purkinje image that’s produced when the patient fixates on the microscope light. We align the center of the disk with the patient’s visual axis.
“There are reports of the need to recenter some inlays,” Dr. Tamayo continues. “The incidence, though, is no more than 3 or 4 percent. Of course, the surgery isn’t really complete until you see the inlay perfectly centered at the slit lamp after the implantation. Recentration shouldn’t be a problem as long as the patient is taken back to the slit lamp postop. There also have been some problems reported with halos, but they tend to disappear with time just as they tend to do with multifocal intraocular lenses. Also, these halos are mainly related to decentered inlays, so centration, again, is crucial. The other thing is the presence of transient light sensitivity, which has been reported as being similar to that experienced with other femtosecond laser treatments. If this light sensitivity occurs, it resolves with a one-month treatment of a mild steroid.”
In terms of results, Dr. Tamayo says that the results from the inlay’s CE approval in Europe show that 90 percent of patients see 20/30 or better at distance and near at six months uncorrected. He says the intermediate vision is affected immediately postop, and takes some time to recover. “We believe it’s related to the fact that the distance vision is decreased in the first couple of months and then slowly returns as well,” he says.
The Microlens is currently in Phase II trials in the United States, and is only used for emmetropic presbyopes who have an error of no more than +1 or -1 D. “The company is looking into widening the number of patients that the lens can work for,” Dr. Tamayo says.
ReVision Optics PresbyLens
The PresbyLens is a hydrogel implant thinner than a human hair, with a refractive index similar to corneal tissue. Used in emmetropic presbyopes, it works as an additive treatment rather than one in which tissue is subtracted. When placed beneath a corneal flap, its presence changes the anterior curvature of the cornea to enhance a patient’s near vision.
ReVision Optics is close to submitting its trial data for approval, so the company is holding off on discussing it until later in the process.
“The Kamra is designed to give better distance, intermediate and near vision based on the pinhole’s depth-of-focus effect,” says Dr. Waltz. “The depth-of-field effect is about 2.5 D, and gives an approximation of accommodation.”
In practice, when implanting the Kamra, centration is key. “We initially thought that being within a couple hundred microns of the center of the visual axis would be ‘close enough,’ but it wasn’t,” says Dr. Waltz. “We’ve found that placing the Kamra’s aperture over the center of the axis is critical. For proper centration, we now use a device made by the SMI Corp. that images the visual axis, iris and the anterior segment and displays the relationship of all those factors to each other digitally.” Dr. Waltz estimates that the SMI device costs between $25,000 and $30,000.
“We only had a handful that required recentration during the study,” says Dr. Vukich. “Frankly, some of them were facilitated by our understanding of the disparity between the first Purkinje image, the visual axis and pupil opposition that we gained by using the SMI heads-up display device.” Dr. Waltz says the device usually doesn’t migrate after surgery, but, if a decentration does occur, it’s decentered during implantation. “It’s usually not something that happens a day or two later,” he says. “Once it’s sitting somewhere, that’s where it stays. In my patients in the trial, without the SMI device, I had to go back and recenter it between 5 and 10 percent of the time. With the SMI device you’re able to tell immediately if you need to recenter it.” The inlay is also very fragile. “Since it’s only 5 µm thick, you can destroy it easily,” says Dr. Waltz. “It’s easy to drop and let go of inadvertently. You have to be gentle when working with it.”
In a study conducted outside of the United States, in the 243 eyes available to follow-up at 18 months, the average uncorrected near acuity in the implanted eye is a little better than J3 (they saw an average of J8 preop). In the same group, the average uncorrected distance acuity in that eye is just below 20/20, which is a slight decrease from a baseline average in these emmetropes that was better than 20/20.
Dr. Waltz says the patients in the U.S. trial, who number a little more than 500, will reach the two-year follow-up point in the next six months, and the company may submit its application for approval early in 2012.
Flexivue Microlens
The Microlens is a 3.2-mm disk that is implanted 300 µm deep in a corneal pocket in a patient’s non-dominant eye. It has no power in the central 0.4 mm but has a power ranging from +1.5 to +3.5 D in the periphery in 0.5-D increments. “It reinforces the theory that the central visual axis must be respected to produce good distance visual acuity,” says Bogota, Colombia, surgeon and Microlens researcher Gustavo Tamayo.
“We advise all Microlens users to do a monovision trial in a patient before implanting the lens,” explains Dr. Tamayo. “But the trial has to be with a low-power contact lens, maybe 1.25 to 1.5 D in one eye at the most, because the difference between the two eyes with the Microlens isn’t very much at six months postop. The patient has to have a somewhat easygoing personality, and be someone who can accept a little bit of loss of distance vision in one eye for a gain in his near vision. The implanted eye’s distance vision will be around 20/30 or 20/25, while the fellow will be 20/20 or 20/15.”
To implant the lens, surgeons currently use a femtosecond laser. “We create the corneal pocket with an IntraLase iFS 150,” says Dr. Tamayo. To generate just a pocket and not an entire flap, the surgeon places a mask over the laser cone. The mask blocks some of the beam, preventing the femtosecond laser from going to certain areas of the cornea and allowing it to make the pocket shape the surgeon needs. “The pocket is a kind of flap,” says Dr. Tamayo. “It has a border where you can dissect it open. The surgeon then places an inserter, containing the inlay, into the pocket and slowly releases the Microlens as he extracts the inserter. We center the inlay with the Purkinje image that’s produced when the patient fixates on the microscope light. We align the center of the disk with the patient’s visual axis.
“There are reports of the need to recenter some inlays,” Dr. Tamayo continues. “The incidence, though, is no more than 3 or 4 percent. Of course, the surgery isn’t really complete until you see the inlay perfectly centered at the slit lamp after the implantation. Recentration shouldn’t be a problem as long as the patient is taken back to the slit lamp postop. There also have been some problems reported with halos, but they tend to disappear with time just as they tend to do with multifocal intraocular lenses. Also, these halos are mainly related to decentered inlays, so centration, again, is crucial. The other thing is the presence of transient light sensitivity, which has been reported as being similar to that experienced with other femtosecond laser treatments. If this light sensitivity occurs, it resolves with a one-month treatment of a mild steroid.”
In terms of results, Dr. Tamayo says that the results from the inlay’s CE approval in Europe show that 90 percent of patients see 20/30 or better at distance and near at six months uncorrected. He says the intermediate vision is affected immediately postop, and takes some time to recover. “We believe it’s related to the fact that the distance vision is decreased in the first couple of months and then slowly returns as well,” he says.
The Microlens is currently in Phase II trials in the United States, and is only used for emmetropic presbyopes who have an error of no more than +1 or -1 D. “The company is looking into widening the number of patients that the lens can work for,” Dr. Tamayo says.
ReVision Optics PresbyLens
The PresbyLens is a hydrogel implant thinner than a human hair, with a refractive index similar to corneal tissue. Used in emmetropic presbyopes, it works as an additive treatment rather than one in which tissue is subtracted. When placed beneath a corneal flap, its presence changes the anterior curvature of the cornea to enhance a patient’s near vision.
ReVision Optics is close to submitting its trial data for approval, so the company is holding off on discussing it until later in the process.