Dry eye is a complex disease with many underlying causes and influential factors. It may be due to a deficiency in one or more of the three tear film layers and can be exacerbated by environmental factors. Consequently, there are many clinical and research tools that are used to diagnose and study dry eye, the sheer number of which can be daunting to a busy ophthalmologist, let alone a patient who wants to learn more about his condition. This month's column will review three simple concepts that will help you educate your patients so that they better understand their dry eye and how it can be managed.
Non-invasive Tear Break Up Time
Many feel that the accuracy and reproducibility of tear film break-up time has improved significantly over the last few years. Researchers have shown that by using well-controlled, micro-quantities of sodium fluorescein (5 µl or less), tear-film breakup measurements are more precise. Having achieved standardization of this tool, it was also discovered that a correlation between ocular discomfort and tear-film breakup time exists. In hundreds of dry-eye patients, it has been observed that within one second of tear-film breakup time, 73 percent of the patients experience ocular awareness followed by discomfort. This manifestation of ocular discomfort may stimulate the eye to blink, replenishing the tear film and providing protection of the ocular surface. If the patient has a short tear film break-up time due to disease or other factors such as systemic medications known to cause ocular drying or an altered blink rate as a result of staring at a computer screen, symptoms and signs can be exacerbated. Therefore, the relationship between tear-film breakup time and blink rate is critical as we have discussed in recent columns. But what does this mean to the patient?
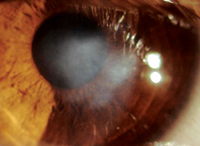
Our improved understanding of tear-film breakup time and its relation to blink rate suggests a potentially simpler and non-invasive determinant of tear-film stability. This test is known as the Non-Invasive Tear Film Break-Up test or NIBUT. If you have your patient stare straight ahead and monitor the time from his last complete blink and the moment he reports ocular awareness, this time will be within approximately one second of his tear-film breakup time (See Figure 1). Not only can the ophthalmologist perform this test in the office, but a patient can conduct it at home as well. The non-invasive breakup time test allows dry-eye patients to independently monitor their condition under different circumstances and evaluate the ability of currently available treatments to relieve his symptoms.
| Figure 1. Non-invasive Breakup Test |
| Improved understanding of tear-film breakup time and its relationship to ocular awareness allows for a simple test. The Test - • Obtain a stop watch or clock • Blink twice, then stare straight ahead • Record the time between the last complete blink • and the first sensation of ocular awareness This time (in seconds) is the non-invasive breakup time. |
A Dry Eye Symptomatic "Zone"
In a recent study, researchers learned that duration of dry-eye symptoms correlates with corneal sensitivity. They observed that, in dry eye, patients with normal corneal sensitivity (> 4 aesthesiometer reading) have been experiencing symptoms for 6.5 years while dry-eye patients with low corneal sensitivity (</= 4 aesthesiometer reading) have been experiencing symptoms for 10 years. Surprisingly, regardless of their corneal sensitivity, these patients reported a similar low-level intensity of ocular discomfort when not exposed to adverse environmental conditions. This data suggests that a dry-eye symptom "zone" may exist in which most dry-eye patients experience similar levels of discomfort. The mechanisms that maintain dry eye patients within this symptomatic zone may be a proper balance of their compensatory mechanisms.
Therefore, it may be suggested that a patient's ability to compensate, such as reflex tear or blink, is what regulates a patient's ability to remain within the low-level ocular discomfort zone for as long as possible when faced with a challenging situation. These situations include dry environments, extended visual tasking and the use of systemic medications known to cause ocular drying. As seen in Figure 2, severe dry-eye patients may become more symptomatic compared to mild dry-eye patients more quickly when presented with a challenging situation.
 |
The graphical representation of this symptomatic zone may prove useful when explaining to a patient how and why he experiences ocular discomfort. By better educating a patient about the severity of his condition with this simple tool, he may be more compliant when instructed to avoid situations that may exacerbate his signs and symptoms.
The Surface Microenvironment
Over the past three decades, studies have identified numerous interrelationships among hormones, mucins, oils, growth factors, retinoids, cytokines and their sites of action found in lacrimal, corneal and conjunctival tissues. To better understand such findings, researchers began to conceptualize the ocular surface as a single-functioning and highly interactive unit. The importance of this concept is understood by ophthalmologists but not necessarily by their patients. So how can we translate the information for dry eye sufferers, who desperately want to learn more but do not have a scientific background?
| OPI in the Clinic |
| Calculate the OPI by: |
|
Visual count of blinks/min. while patient reads ETDRS Chart; If TFBUT is Ž IBI Patient is PROTECTED Severity may be determined by the degree of discrepancy between IBI |
An analogy which may help simplify the importance of the various components of the tear film is that of a goldfish. Explain to your patient that the epithelial cells on the surface of her eye are each similar to a fish. And the tear film surrounding the cell is like a fish bowl, containing a proper balance of hydration, pH, osmolarity, temperature, oxygenation, nutrients, amino acids, glucose and waste removal. When there is dirty water in the fish bowl, which equates to an imbalance within the tear film, the goldfish begins to die just as the epithelial cell would.
A simple image such as the one shown in Figure 3 can help demonstrate this concept to your patients. This tool may inform dry-eye patients about how delicate the system actually is and that by modifying simple behavior, such as avoiding smoky environments, they can better control their disease.
Patients who can understand the underlying causes of their condition and the factors that may influence it can then participate in the process of managing it. The concepts presented in this month's column represent a step in the direction of simplifying a complex disease and arming dry-eye patients with tools that can be used to monitor their condition and evaluate the effectiveness of therapy.
 |
Next month, we'll discuss the newest entry for the treatment of dry eye, the recently approved Restasis (cyclosporin 0.05% ophthalmic emulsion, Allergan). Restasis is indicated to increase tear production in patients whose tear production is presumed to be suppressed due to ocular inflammation.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Mr. Ousler is senior clinical manager of the dry eye department and Ms. Humphrey is a research associate at Ophthalmic Research Associates in North Andover.
Suggested Reading:
1. Nally L, Ousler GW, Abelson MB. Ocular discomfort and tear film break up time in dry eye patients: a correlation. IOVS 2000;41:4(ARVO Abstract#1436).
2. Abelson MB, Ousler GW, Nally LA, Emory TB. Dry eye syndromes: Diagnoses, clinical trials and pharmaceutical treatment: 'Improving clinical trials'. In Sullivan DA, ed. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3. New York: Kluwer Academic/Plenum, 2002:1079.
3. Nakamori K, Odawara M, Nakajima T, Mizutani T, Tsubota K. Blinking is controlled primarily by ocular surface conditions. Am J Ophthalmol 1997;124:24-39.
4. Lemp MA. Report of National Eye Institute/industry workshop on clinical trials in dry eye. CLAO J 1995;21:221-32.
5. Ousler GW, Emory TB, Welch D, Abelson MB. Factors that influence the inter-blink interval (IBI) as measured by the ocular protection index (OPI) (poster presentation). The Association of Research in Vision and Ophthalmology, 2002 (Abstract #56).
6. Korb DR, Finnemore VM, Herman JP, et al. A new method for the fluorescein breakup time test. IOVS 1998;40.
7. Bron AJ, Mengher LS. The ocular surface in keratoconjunctivitis sicca. Eye 1989;3:428-37.