|
| The Amoils brush can be useful when you need a large treatment area, surgeons say. (All images courtesy Elizabeth Hofmeister, MD.) |
The Right Patient
Surgeons say that, depending on your readiness to perform surface ablation, patient inclusion criteria can vary.
William Wiley, MD, assistant clinical professor of ophthalmology at University Hospitals/Case Western University, says he’s more apt to reserve surface ablation for certain patients. “I like surface ablation, but if I can do LASIK or—for a patient with high myopia—an ICL, I prefer to do either of those,” he says. “The main reason I would do surface ablation would be for thinner corneas with milder prescriptions. Also, if a cornea is borderline suspicious for keratoconus, or the patient has slightly irregular topographies, I’d prefer not to perform vision correction. However, in some cases involving a highly motivated patient with just one thing that might be slightly suspicious, such as slight inferior steepening and a mild prescription, we’d discuss surface ablation. I would also discuss the risk of ectasia, and that the patient might need to be followed over time. We’d also plant the seed for the possibility of cross-linking for corneal strengthening after six months.”
Austin, Texas, refractive surgeon Steven Dell says that, though dry-eye concerns might push some physicians in the direction of recommending surface ablation to certain patients, he doesn’t subscribe to that notion. “We don’t automatically do surface ablation in patients in whom we fear dry eye,” he says. “I don’t think dry eye is less common with PRK than it is with LASIK. In data on around 32,000 patients at [the U.K.’s] Optical Express, Dr. Steve Schallhorn found dry eye to be less common with LASIK than PRK postop. So, for us, the threat of dry eye isn’t a reason to go to surface ablation in a patient who would otherwise be a candidate for LASIK.”
In an interesting juxtaposition from most surgeons’ experience, in the U.S. Navy, PRK is actually more popular than LASIK, mainly because of patient choice. “Fifty-five percent of our procedures are PRK,” says Capt.
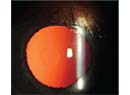
Elizabeth Hofmeister, MD, a refractive surgeon who practices at the Naval Medical Center in San Diego. “Forty-four percent are LASIK and just under 1 percent are ICL. We do a lot of surface ablation. It usually comes down to patient choice—they’ve done some research and heard the information in our informed consent process and they decide which procedure they want. Depending on what we find in their preoperative exam, however, we may steer patients toward PRK. One big patient category that we steer toward PRK consists of individuals with corneal scars. If the scar is deep or prominent enough, we’re concerned that that might be a place for vertical gas breakthrough during the creation of the femtosecond LASIK flap. Also, we operate on very young patients—in their early 20s—and we try to avoid performing any kind of corneal refractive surgery on anyone we think might have keratoconus. However, if they have questionable topography but it’s not at the point where you could even make a diagnosis of forme fruste keratoconus, we’ll steer them toward PRK. Otherwise, beyond those indications, it’s up to the patient to decide.”
Intraoperative Tips
Surgeons say you can have success with different methods of epithelial debridement to start the procedure.
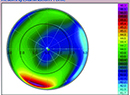
Dr. Hofmeister says the Navy’s centers have settled on debridement with a rotating brush. “Years back, we did studies on different methods of epithelial removal, and what we decided on as being the best, most reliable method was the rotating Amoils brush,” she says. “It’s rare that we’ll do alcohol debridement, and we don’t have the capability to do a laser epithelial removal that would get a large enough area of epithelium to incorporate the large-zone treatments we like to use—it would be limited to a 6-mm zone. We tend to use the 9-mm brush head for all our patients. We know that we might not quite need 9 mm for our myopes, but you definitely need it when treating a low hyperope.”
Dr. Dell, however, gets the best results with alcohol debridement. “We place a well over the desired optical zone and irrigate some alcohol solution, 20% ethanol, onto the cornea for about 30 to 35 seconds,” he explains. “The epithelium comes right off. Note that there will be a little bit of seepage of the alcohol beyond the confines of the well, so you’ll end up with a slightly larger epithelial defect than the size of the well. For example, using a 7.5-mm well would result in an 8-mm defect. This is nice because it allows you to titrate the defect. If I’m treating a low prescription, such as less than a diopter of myopia, I really don’t need a huge epithelial defect, so I can use a smaller well. Having a smaller defect speeds the healing process. The rationale behind this is that the so-called transition zone beyond the 6-mm optical zone isn’t important when you have a very low correction and the difference between treated and untreated cornea isn’t particularly significant.
“If you’re treating a very high prescription, however,” Dr. Dell continues, “you don’t want an abrupt transition zone between treated cornea and untreated peripheral cornea. In those cases, the optical zone and the transition zone are both very important. In those cases, we’d tend to use a larger epithelial defect diameter. Whichever size well you use, after you remove the epithelium it’s important that you wick away the alcohol and don’t let it get on the conjunctiva, because it can be very irritating to the patient.”
Dr. Wiley sometimes uses the laser scrape technique referred to by Dr. Hofmeister, but says, “We’ve seen some variable responses due to irregular epithelium in which the stroma is ablated along with the epithelium, causing unexpected outcomes or refractive surprises.” He says he prefers to use the alcohol technique. Recently, however, he’s been incorporating a new device from Israel’s Orca Surgical called Epi Clear. The device is used for a procedure the company is billing as epithelial Bowman’s keratectomy. “EBK preserves Bowman’s membrane prior to laser ablation,” Dr. Wiley explains. “Of course, when you laser the cornea you laser through Bowman’s, but in the periphery Bowman’s will still be intact. By preserving Bowman’s there, it’s thought that, when the epithelium regrows, it grows in more of a lamellar, regular fashion that could result in faster healing. We haven’t done enough eyes to see if that theory is correct, but it looks promising. The way the Epi Clear works is it scrapes across the cornea with two parallel plastic blades. One of the blades is a little lower than the other, allowing it to remove epithelial cells in a controlled manner. The cells slide up off the cornea and between the two blades. The blades are designed to be sharp enough to remove epithelium but dull enough to not penetrate Bowman’s. It’s a single-use blade head.”
Refractive surgeons also make sure to take steps to reduce the risk of haze postop. “The naval centers vary, but most try to rapidly cool the cornea as soon as the refractive ablation is completed,” says Dr. Hofmeister. “Some use a chilled Merocel sponge, some use chilled BSS. At our center, since our rooms are so cold, we use room-temperature BSS after the ablation, and this might reduce the risk of haze. We also use mitomycin-C on many of our PRK patients, an off-label use of the drug. We use 0.1 mg/ml for a duration of 15 seconds, followed by copious rinsing with BSS.” Drs. Dell and Wiley use MMC for all of their ablation cases. “It’s been many years since I’ve seen a case of haze,” avers Dr. Dell.
 |
| An ice-pack mask placed over the eyes from time to time during the postop period following a surface ablation procedure can help reduce swelling and decrease postoperative pain until the eye has had a chance to recover. |
Postop Pain Control
Though PRK doesn’t stand for Painful Refractive Keratectomy, there are some patients who might disagree for the first couple of days postop. Here are some ways to control PRK’s sometimes considerable discomfort.
Dr. Hofmeister takes several measures. “Pain is definitely a big concern for patients following PRK,” she says. “We spend a lot of time preop explaining what they should expect so that when they have the pain afterward, they’re not shocked or surprised. To try to manage it, we take a multilevel approach: an oral NSAID, and we try to have them keep a steady state of that medication as a baseline; a bandage contact lens postop, which I think is the biggest advance in reducing pain after PRK; ice packs to try to decrease swelling and pain; a breakthrough pain medication such as Norco or Percocet; and a non-preserved topical anesthetic—we use tetracaine—which has been a wonderful source of relief for patients. When the pain gets really bad on the first or second postop night, they can use the non-preserved anesthetic. The benefit of the bandage lens is today’s lenses can breathe and move, yet still reduce the friction of the lid against the large epithelial defect that we’ve created. This really helps with pain management.”
In addition to NSAIDs, steroids, antibiotics and an anesthetic rescue drop for two days postop, Dr. Dell has taken a cue from Colman Kraff, MD, of Chicago, and places a drop of Bausch + Lomb’s Prolensa under the bandage contact lens, which Dr. Kraff believes helps with healing. Dr. Dell also gives patients an oral pain medication, but, he says, “The vast majority of patients don’t need to use it.” REVIEW
None of the surgeons has a financial interest in any product mentioned in the article.