LASIK has been performed for more than 30 years with impressive results, but surgeons and patients are always on the lookout for something new and—possibly—improved. It’s with this mindset that eyes were turned toward the relative newcomer in the refractive surgery marketplace, small-incision lenticule extraction, performed with the VisuMax femtosecond laser (Carl Zeiss Meditec; Jena, Germany). Even though SMILE is in its relative infancy as a go-to refractive procedure, it’s producing results similar to advanced LASIK—but it’s not without its issues. Here, experts discuss the relative merits of the two procedures, and we also look at the results of well-performed studies of the surgeries.
A Look at the Results
|
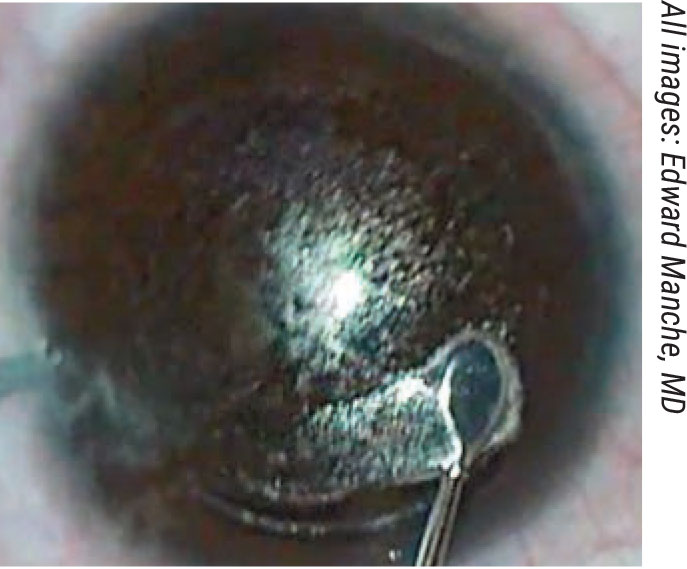
| Separating the lenticule from the stroma can be technically difficult, surgeons say. |
Because the results are so similar, it can be difficult for surgeons and patients to choose between the two procedures.
For example, a retrospective case series from Turkey found that SMILE and FS-LASIK were safe and similar in terms of efficacy and predictability at five-year follow-up for the correction of myopia and myopic astigmatism.1 The study included 44 eyes from 22 patients who received SMILE in one eye and FS-LASIK in the contralateral eye. Patients were examined at one, three and five years.
At the five-year follow-up, all eyes in both groups were within 1 D of attempted spherical equivalent refraction, and no statistically significant difference was found between the intended and achieved correction comparing the groups at any time points.
Edward Manche, MD, director of the Cornea and Refractive Surgery Service at Stanford University School of Medicine, has been performing SMILE surgery since it was approved in 2016, so he’s familiar with the trade-offs of each. “Both LASIK and SMILE work very well,” he says. “Both provide excellent outcomes and safety, and both can be used in about 85 percent of all patients that come into a typical practice. However, SMILE isn’t yet approved for hyperopia or mixed astigmatism. In addition, in the United States, we’re limited to 3 D of astigmatism or less with SMILE. So, within those parameters, SMILE and LASIK have a pretty wide approval, and a lot of the choice in procedure comes down to patient preference.”
John Vukich, MD, who is in practice in Wauwatosa, Wisconsin, was one of the primary investigators for SMILE and VisuMax and has a long history of performing LASIK. “In my previous refractive surgery practice, we were considering SMILE to be a premium procedure, so we were charging slightly more for it,” he says. “We believe that SMILE and LASIK aren’t completely equivalent and, physiologically, SMILE may have some advantage over LASIK, the more traditional option. SMILE is the newer technology, has a very good safety profile, and preserves a greater amount of integrity of the structure of the cornea.”
Dr. Vukich says he’s encountered patients who have done research and have come to the conclusion that SMILE was a better procedure for them. “You try to be even-handed,” he says. “The majority of our cases remained LASIK, however. When given the choice, some of the decision was driven by the price differential, some of it was driven by familiarity and some of it was driven by just the potential longevity of exposure to LASIK.
“The quality of vision is very high for both procedures,” he adds. “Sometimes, there’s a day or two of additional recovery time for SMILE. However, there’s also always the possibility of delayed healing with LASIK, whether it be from striae or epithelial issues related to drops or other things. So, I would say the procedures are roughly equivalent in terms of acuity and patient satisfaction.”
The Advantages of LASIK
According to Dr. Manche, one of the advantages of LASIK is that it’s been around a long time, with tens of millions of procedures having been performed. “It’s a very well-known and mature technology,” he says. “SMILE was approved in the United States in 2016, and about 3 million cases have been performed worldwide.”
Additionally, LASIK has faster visual recovery. “When SMILE was initially approved in the United States, we were using relatively high energy levels,” Dr. Manche says. “ The use of higher energy levels in SMILE surgery has been associated with significantly slower visual recovery. So, when SMILE was first released, many patients experienced slower recovery of vision. It was common to have patients seeing 20/40 or 20/30 on postoperative day one. This is in contrast to what you see with LASIK, after which the majority of patients see 20/20 or 20/15 on day one.”
SMILE was first approved in the United States for spherical myopia. A second approval for the treatment of compound myopic astigmatism came in 2018. With the second approval, surgeons were finally allowed to make adjustments to the energy levels. “The Zeiss clinical care specialist, in concert with the surgeon, carefully adjusts the energy levels to the point where the surgeon can still achieve easy lenticule dissection, but where they’re not seeing much of the opaque bubble layer,” explains Dr. Manche. “Lower energy levels can provide significantly better uncorrected visual acuity from postop day one. With the lower energy settings, we’re now seeing patients who are 20/20 or 20/25 on day one. We even see an occasional patient at 20/15 or better. The postoperative day one vision is still not quite as good as with LASIK, but it’s significantly better than what we saw in the early approval with our standard, fixed, higher treatment energy levels.”
Another advantage of LASIK is that it’s easy to do a touch-up. Surgeons can lift the flap and perform a retreatment. “In comparison, surgeons cannot perform a repeat SMILE surgery on an eye that’s already had SMILE,” notes Dr. Manche. “If an eye that has previously had SMILE requires an enhancement procedure, you are left with a couple of options. You can perform LASIK surgery by cutting a flap in the SMILE cap. In the United States, the SMILE cap thickness is defaulted at 120 µm, so you then have to cut a LASIK flap at either 90 µm or 95 µm, which only gives you about 25 to 30 µm of play between the cap cut and the flap cut. Some surgeons aren’t comfortable with that. Another choice is to perform a side cut and open up the original 120-µm SMILE cap and convert that into a LASIK flap. A final choice is to perform PRK surgery on top of the SMILE cap. I don’t like to cut a LASIK flap 25 to 30 µm away from the SMILE cap interface, so I perform PRK touch-ups for all of my SMILE enhancements.”
The Advantages of SMILE
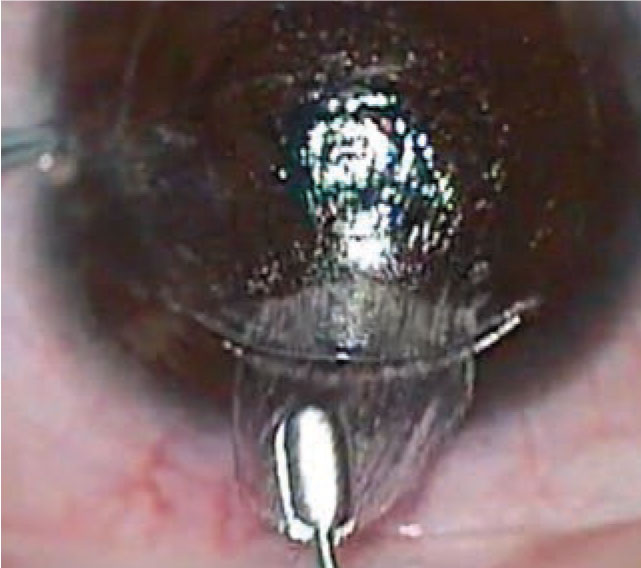
|
| Physicians say that, once the SMILE lenticule is removed, it pays to check it for tears that could mean tissue is left behind. |
One of the advantages of SMILE is the smaller incision. “We’re defaulted to a 4-mm incision in the United States,” Dr. Manche explains. “In other countries, it’s even smaller. This small incision provides less transection of the nerves in the cornea, and that’s directly correlated to how denervated the cornea becomes, and also how much dry eye the patient experiences, especially in the early postoperative period. Typically, there’s less induced dry eye with SMILE compared with LASIK because LASIK requires a 270-degree circumference flap. With LASIK surgery, you’re severing all of the nerves in that area, which leads to relative denervation of the cornea. Typically, corneal reinnervation takes place over the course of six to 12 months. Another advantage to SMILE is that there are no flap complications.”
Additionally, studies have shown that, compared to LASIK, SMILE provides potentially better biomechanical stability of the cornea. “Some very good work has shown that the anterior lamellar tissue in the cornea is the strongest,” Dr. Manche says. “SMILE spares the anterior corneal lamellar tissue. The side incision with SMILE is only 4 mm compared to the 20-mm incision with LASIK. There’s significantly more transection of the corneal lamellae with LASIK compared to SMILE. Preservation of the anterior stromal tissue results in a reduced biomechanical insult to the cornea with SMILE, and that could have implications with regard to lowering the risk of ectasia.”
Head-to-Head Studies
As mentioned above, outcomes of the two procedures are quite comparable. Dr. Manche just completed a randomized clinical trial of 40 patients who underwent wavefront-guided LASIK in one eye and SMILE in the fellow eye. He assessed patients at one, three, six and 12 months. “We did find slightly better outcomes with wavefront-guided LASIK compared to the SMILE surgery,” he says. “We had slightly more LASIK eyes achieve an uncorrected visual acuity of 20/20, as well as higher levels of visual acuity of 20/16 and 20/12.5. Additionally, we had greater gains of lines of best-corrected visual acuity in the wavefront-guided LASIK group compared to the SMILE group. So, on the whole, the outcomes were very similar, but there were small but measurable benefits to wavefront-guided LASIK compared to SMILE.” Dr. Manche will be presenting the results of this study at this year’s meeting of the American Society of Cataract and Refractive Surgery.
For another perspective, a recent study conducted in China found that, when compared to LASIK, SMILE may offer better safety and objective visual quality, comparable stability and efficacy, but slightly inferior predictability when correcting myopia exceeding 10 D.2 This prospective, randomized, comparative study included 60 eyes in 60 patients. Thirty eyes were corrected using SMILE, and 30 were corrected using FS-LASIK. Patients received preoperative and six-month postoperative examinations.
At six months postoperatively, the uncorrected distance visual acuity was -0.01 ±0.06 logMAR (a little better than 20/20) in the SMILE eyes and -0.05 ± 0.10 (a little better still) in the LASIK eyes, while the corrected visual acuity was -0.07 ± 0.07 logMAR in the SMILE eyes and -0.08 ± 0.08 (a shade off of 20/16) in the LASIK eyes.
Postoperative spherical equivalent refraction was -0.20 ±0.25 D in the SMILE eyes and -0.03 ± 0.20 D in the LASIK eyes, and the posterior corneal curvature was unchanged after both procedures. The measured corneal thickness was reduced by 137.40 ±15.01 µm in the SMILE eyes and by 155.06 ±17.43 µm in the LASIK eyes. The change in the SE was -0.01 ±0.26 D in the SMILE eyes and -0.13 ± 0.30 D in the LASIK eyes after one week. Only the peak distance (the distance between the highest points of the nondeformed corneal parts) differed between the groups; the distance was 1.06 ±1.44 mm in the SMILE eyes and -0.26 ±1.16 mm in the LASIK eyes. The SMILE eyes had smaller changes in higher-order aberrations and spherical aberration than the LASIK eyes.
Interestingly, another Chinese study found that, while SMILE is as effective as FS-LASIK in correcting high myopia, attention should be paid to the induction of vertical coma in highly myopic patients following SMILE.3
This prospective, comparative study included 52 eyes of 34 consecutive highly myopic patients with spherical equivalent between -8 and -10 D. Twenty-three eyes of 16 patients underwent FS-LASIK, while 29 eyes of 18 patients underwent SMILE. Visual outcomes and wavefront aberrations were analyzed preoperatively and six months postoperatively.
At the six-month visit, 96.6 percent of eyes in the SMILE group and 91.3 percent in the FS-LASIK group achieved unchanged or better best-corrected distance visual acuity. Additionally, 96.6 percent of eyes in the SMILE group and 95.7 percent in the FS-LASIK group achieved uncorrected distance visual acuity of 20/20 or better. As for wavefront aberrations, high-order aberrations and spherical aberrations increased significantly after surgery in both groups relative to preoperative values, and vertical coma increased after SMILE. Other than the difference in vertical coma, there were no statistically significant differences in the changes in higher-order aberrations, spherical aberrations, horizontal coma, coma, horizontal trefoil, vertical trefoil or trefoil between the two groups.
The Future
According to Dr. Vukich, SMILE is another step in the evolution of corneal recontouring as it relates to a refractive outcome. “We have data to support that the intrastromal removal of tissue versus the creation of a cap leaves intact a greater percentage of the corneal strength and integrity, and we believe that to be an advantage in the long run,” he says. “Many patients seeking refractive surgery are in their 20s and 30s, and they’re making decisions with the understanding that they will need to have healthy eyes and good vision for maybe another 70 years. All things being equal, a greater percentage of retained corneal structural integrity is a tiebreaker for many people.”
Dr. Manche agrees. “In all fairness, SMILE is relatively new, and it’s really quite impressive how good the data are this early in the evolution of the procedure,” he says. “I think it’ll just get better with time.”
Pertinent to the article’s topic, Dr. Manche performs sponsored research for Alcon, Carl Zeiss Meditec and Johnson & Johnson Vision. He is a consultant for Johnson & Johnson Vision. Dr. Vukich has no financial interest in any of the products discussed.
1. Aygun BT, Cankaya KI, Agca A, et al. Five-year outcomes of small-incision lenticule extraction vs femtosecond laser-assisted laser in situ keratomileusis: A contralateral eye study. J Cataract Refract Surg 2020;46:3:403-409.
2. Yang X, Liu Q, Liu F, Xu J, Xie Y. Comparison of outcome between small incision lenticule extraction and FS-LASIK in eyes having refractive error greater than negative 10 diopters. J Cataract Refract Surg 2020;46:1:63-71.
3. Yang W, Liu S, Li M, Shen Y, Zhou X. Visual outcomes after small incision lenticule extraction and femtosecond laser-assisted LASIK for high myopia. Ophthamic Res 2020;63:4:427-433.




