Preop Preparation
Surgeons pay close attention to the ocular surface preop, and manage dry eye aggressively.
"Since the introduction of Restasis (cyclosporine A, Allergan), I've been using it more and more prior to refractive surgery to get patients prepped and their eyes nicely lubricated," says Chicago surgeon Lou Probst. "We don't use it universally, but we have a very low tolerance for any dry-eye signs or symptoms. Basically, we'll use it for females over 35, anyone with contact lens intolerance, a patient who mentions that he's had dry eyes or used lubricating drops, or someone with a skin condition. This usually amounts to 50 to 60 percent of patients." He will put patients on it a month to a week before LASIK, depending on the severity of the dry eye, and have them stop using it the day before the surgery. They will then resume Restasis after LASIK for one to three months.
 |
|
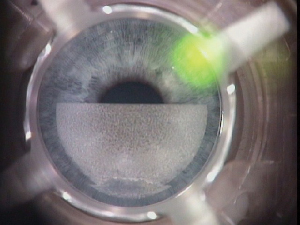
British surgeon Sheraz Daya waits for the IntraLase cavitation bubbles to disperse before checking pachymetry on certain eyes to ensure there's enough tissue remaining to ablate. |
In support of his use of Restasis, Dr. Probst points to a study presented at the 2005 meeting of the Association for Research in Vision and Ophthalmology (Ursea R, et al. Invest Ophthalmol Vis Sci 2005;46: ARVO E-Abstract 4381). In the retrospective report, surgeons looked at 100 patients who underwent LASIK for various levels of correction. There were 54 women and 46 men, with ages ranging from 22 to 69. The physicians treated 54 patients were with Restasis. At the beginning of the Restasis use, 63 percent of patients (34 patients) complained of dry eyes.
One week postop, 46 percent (25 patients) achieved 20/15 vision, 39 percent (21 patients) had 20/20 vision and 15 percent (eight patients) saw worse than 20/25. In the group of 46 patients not receiving Restasis, 57 percent (26 patients) didn't improve to better than 20/25 at one week after surgery. None of the Restasis patients reported adverse events. The researchers report that patients using Restasis were significantly more likely than those who didn't use Restasis to have 20/15 vision (p=.017). Non-users were significantly more likely than patients who used Restasis to have a visual outcome worse than 20/20 (p<.001).
Boston surgeon Samir Melki heavily emphasizes preop patient counseling and informed consent to make sure patients know the limits of the procedure and so that he's protected legally. Before the surgery, he has patients sign a list of statements about the procedure indicating that they're aware of unusual situations that could have an effect on the outcome, such as a history of dry eye, a small cataract or a history of mitomycin-c. "The patient writes in his own handwriting that he was informed about a particular risk," says Dr. Melki. "An example might be that large pupils might cause night-driving difficulty. This list is useful because, many times, I've discussed a particular risk with a patient and then, postop, he says he never heard about it."
If you're planning the ablation using the Visx CustomVue system, but find that you need to adjust the ablation calculations beforehand due to discrepancies between the clinical and the wavefront refractions, Dr. Probst says he uses a straightforward method that he's found to be very effective.
"We first do manifest and cycloplegic refractions," he says. "Then, we keep doing the CustomVue wavefront maps until we get a high-quality one that has a cylinder and axis that match the manifest refraction's cylinder and axis as closely as possible. In the ideal situation, the cylinder may be a little higher than the manifest cylinder, and the axis will be as close as possible. I then use the surgeon-adjust feature of the CustomVue program to adjust the myopic sphere to the lower value of either the manifest or cycloplegic sphere. I've done this for thousands of patients, and haven't had overcorrection problems."
Intraoperative Insights
For the surgery itself, Dr. Melki makes it a point of getting the best suction possible before making the flap cut. "I use pneumotonometry during LASIK, rather than a Barraquer tonometry, to make sure the pressure is above 80 mmHg," he explains. He doesn't feel that the indicator some surgeons use, vision loss by the patient, is a good one, and prefers to be more precise. "We've found that just pressing on the eye can induce amaurosis," he says.
A safety measure favored by London's Sheraz Daya, MD, is intraoperative pachymetry before and after the flap cut, to make sure there's enough tissue remaining to ablate. He says this is useful both for users of microkeratomes and those with IntraLase lasers. For the latter, he says that, though the device almost always makes a flap of the thickness you set at the controls, within a few microns, "sometimes it drifts and you have to watch out for that." If he begins to suspect that his IntraLase is drifting toward thicker flaps, he'll wait a while after flap creation for the residual bubbles (which the IntraLase leaves behind after making a flap) in the cornea to clear and then check the pachymetry. If the flaps are getting thicker, he stops using it in all high myopes until the company can recalibrate the laser.
 |
|
Suturing can help if vision-threatening epithelial ingrowth returns after scraping. |
Dr. Daya also tries to manipulate the flap as little as possible, avoiding the use of sponges in the middle of the flap or pressing the flap down with sponges. Instead, he uses a metal spatula because it's smoother and won't create ridges or striae. "It won't disturb the epithelium very much either if the eye is well-lubricated," he says. He will push down on the peripheral 1 mm with a wet Weck Cel sponge to just drain off the edges.
Postop Pearls
After LASIK, Greensboro, N.C., surgeon Karl Stonecipher takes a three-tiered approach to dealing with postop dry eye. At the one- or two-week mark, if a patient reports mild dryness, he prescribes a topical lubricant; if the dryness is moderate (i.e., the patient is having visual fluctuations or he doesn't respond to artificial tears), he uses Restasis; if it's severe (usually preventing contact lens wear and requiring some pre-LASIK intervention), he'll add punctal plugs.
When faced with a corneal abrasion postop, Minneapolis surgeon Y. Ralph Chu says he's learned to treat it aggressively. "Besides putting a bandage contact lens on, we start patients on once-per-hour steroids and keep the postop antibiotic drops going in order to help them heal faster and minimize the risk of diffuse lamellar keratitis," he says.
If Dr. Chu has to do a LASIK enhancement, he approaches that in a slightly different way, as well.
"I find the edge of the flap by depressing the cornea with Burato forceps with blunt ends," he explains. "Using this technique, you can sort of crack open the edge of the flap and peel it open in one maneuver without having to use a Sinskey hook to break the epithelium, minimizing the risk of epithelial ingrowth."
If a patient's eye has epithelial ingrowth postop, Dr. Melki will instill some fluorescein at the edge of the flap and look for staining that would indicate proliferating cells and an open fistula. If the area of cells isn't big enough to warrant scraping, occasionally, he'll place a bandage contact lens to promote healing. "If there is a fistula, we'll follow the patient a little more closely and make sure it's not progressing," he explains. "If it progresses, and gets closer to the visual axis, we'll scrape it. If it recurs, we'll place stitches."



