In the recent past, many surgeons turned to surface ablation as a hedge against the risk of ectasia associated with LASIK procedures in certain corneas, and this trend reawakened general interest in procedures such as PRK. Since then, refractive surgeons have found that, far from just being a fallback option for LASIK, PRK might actually be preferable in certain situations. In this article, several surgeons well-versed in the use of surface ablation for challenging cases, such as post-radial keratotomy and post-penetrating keratoplasty, share their insights on how to make the most of the procedure in these kinds of patients.
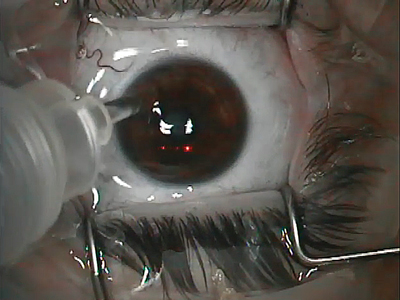
PRK After Cataract Surgery
Surgeons say the sort of cataract patient who needs surface ablation postop is most likely the premium lens patient, since these high-tech implants perform best when an eye’s visual system is as sharp as possible.
“Generally, most cataract patients, about 85 percent, are within 0.5 D of the intended target refraction,” says Sonia Yoo, MD, of Miami’s Bascom Palmer Eye Institute. “That being said, if a surgeon is performing refractive-lens surgery, this means that maybe 15 percent are outside that range. So, for a refractive-cataract surgeon whose patients want to be free of glasses after surgery, he or she has to be prepared to perform laser vision correction—or be affiliated with someone who can perform it—in at least some percentage of patients.”
The first step in giving these patients sharper vision, surgeons say, is making sure the refraction is solid. “It’s important to wait for the refractive error to be stable, and to ensure that the error is due to the way the lens has healed in terms of its effective lens position, and not because of some other reason,” advises Dr. Yoo. “For example, subclinical cystoid macular edema can sometimes cause a hyperopic refractive shift after cataract surgery in some patients and, obviously, that’s something you wouldn’t treat with refractive surgery. Also, though we all do mostly clear cornea cataract surgery, some cataract patients may receive a suture, so it’s also important to remove all the sutures and then wait four to six weeks for refractive stability.” Surgeons say it can take from six weeks to four months for the post-cataract patient to reach a level of stability necessary to undergo a PRK.
To help achieve stable visual acuity pre-PRK, Miami surgeon William Trattler says a YAG capsulotomy is key for getting the best target refraction.
“I often want to perform the YAG first, if necessary, before the PRK, because after the YAG the lens implant may shift slightly in position, which can change the refractive error,” he says. “This avoids a situation where you do the PRK on a patient, then a year later he develops posterior capsule opacification. Then, when you do the YAG, the lens shifts and the refractive error is off-target. In many of my patients who need refractive surgery after cataract surgery, we’ll do a YAG—even if they don’t necessarily need one—and we won’t charge insurance for it. That way, it will be done and we can do the PRK.”
|
The other issue surgeons can run into when dealing with the post-cataract patient specifically, and post-surgical patients in general, is ocular-surface disease. “It’s important to treat the surface aggressively and to acknowledge that having subsequent surgery is going to give the patients drier eyes, at least temporarily,” says Dr. Yoo. “So, I like to be very generous with my use of preservative-free artificial tears. I also have a low threshold for the use of punctal plugs to improve the level of the aqueous tear component both preoperatively and postoperatively. I also will consider using Restasis in patients who are symptomatic.” Dr. Yoo says patients with external lid disease such as rosacea and blepharitis need to have their conditions treated and under control before their PRK because of the infection risk. “Candidates who might not be good for the procedure include those with fluctuating refractive errors or those with corneal epithelial basement membrane dystrophy, whose refractions are somewhat off,” she says. “Also, patients with irregular astigmatism may not be good candidates for PRK.”
In addition to usually taking care of the patient’s residual refractive error, some surgeons say that performing PRK on premium lens patients, rather than LASIK, can have an unintended, though beneficial, side effect: These patients—who tend to be demanding because they’re paying a premium to try to be glasses-free post-cataract—are less likely to constantly return to the ophthalmologist’s office to treat insignificant amounts of refractive error, because surface ablation’s healing period isn’t a breeze. “You will sometimes get patients coming in after LASIK saying, ‘Yeah, I’m seeing 20/20 minus, but it’s not that clear, though,’ ” says Chicago surgeon Parag Majmudar. “Then when you refract them, they’re -0.25 D and they still want an enhancement. That’s inappropriate. You don’t want to take chances like that for what amounts to an insignificant refractive error.”
The RK Patient
Years ago, these patients turned to what was then state-of-the-art refractive surgery, RK, to decrease their dependence on glasses. Now they’re back for more. This time, however, their incised corneas pose more of a challenge.
The first hurdle with these patients is nailing down a good target refraction for the PRK, since in many of them their refraction can fluctuate from morning to night.
“We try to get a couple of different measurements throughout the day,” says Dr. Majmudar. “And we want to get a sense from the patient of how much diurnal fluctuation he has. If he has three or four pairs of glasses for breakfast, lunch, dinner and sometime in between, that’s not a good sign. If it’s a 2- to 3-D shift, you have to find out what the patient’s expectations for surgery are and maybe find a target in between the range of the shift, or err on the side of myopia a little so he can still perform more near tasks, rather than have him be plano-plus after the treatment. This is something you just have to determine on a case-by-case basis. It’s possible that, in the future, cross-linking plus surface ablation may help stabilize these kinds of patients, but that still needs to be fleshed out.”
Dr. Trattler makes sure that the patient can actually benefit from the PRK. “One of the keys is finding out if he’s correctable to 20/20 or 20/25,” he says. “This is important because some of these post-RK patients can have poor vision. However, if he’s correctable to 20/25 or better and is symmetrical on topography, he can be a good candidate.” Dr. Yoo, however, is more conservative, and thinks that a patient whose vision fluctuates more than 0.5 D or so may not be a good candidate. “Usually, though, more than refractive error, there may be times of day that, no matter what refraction you were to put in front of the patient, he simply won’t see well,” she says. “So it’s not just a fluctuation of the refractive error, it’s that no refraction corrects them well because of some amount of irregular astigmatism. I pay close attention to the patient history in these cases.”
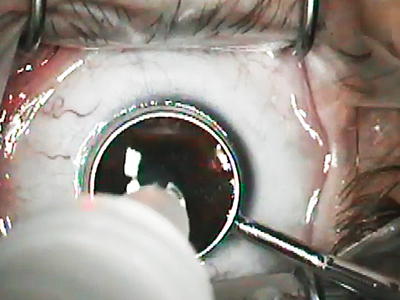
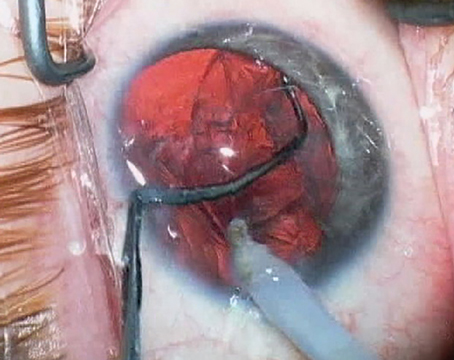
Unlike performing PRK in patients who’ve had cataract surgery, in whom the steps of the procedure itself are pretty standard, PRK in an RK patient has some pitfalls that the ophthalmologist needs to watch out for, say experts.
“It’s important to be careful when removing the epithelium over the RK wounds during the initial part of the surface ablation procedure,” advises Dr. Yoo. “Once you remove the epithelium over the incisions, there may be a roughness there, or you may have difficulty removing it completely, which can induce some irregular astigmatism when you ablate over the incisions.” Some surgeons advise using mitomycin C in these cases to help prevent haze postop.
Dr. Majmudar is also cognizant of the incisions as he works. “You definitely want to make sure that there aren’t any epithelial plugs in the incisions,” he says.
“If there are plugs there, then once you remove the epithelium with alcohol or however you do it, those plugs can come out and you can then get two things: the incisions can splay open, resulting in significant shifts in the refraction; and, if this patient has had micro-perforations in the past, this is a complication that can potentially occur again. Because of these risks, it’s important to make sure that enough time has passed since the RK procedure that there are no epithelial plugs, and that you use a minimally invasive technique when removing the epithelium. To this end, I do the removal using alcohol so as not to put too much mechanical force on the RK incisions themselves.”
|
Toronto surgeon David Rootman adds that he removes the epithelium in a certain fashion so as not to cause problems with the RK cuts. “When you take off the epithelium, take it off from the center out toward the periphery,” he says. “This way, you’re peeling it parallel to the incisions, which are radial. Otherwise, you may split the incisions if they’re not well-healed, which could affect your result and cause the eye to have progressive flattening.”
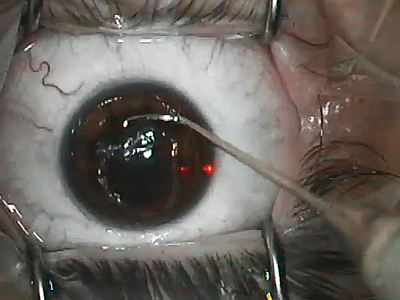
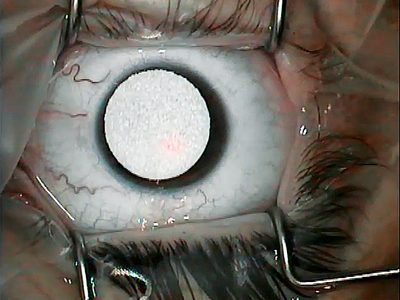
Post-PK Patients
Using PRK to help the vision in a patient who has had a penetrating keratoplasty is challenging because of the variables it presents to the surgeon. Surgeons say, however, that even though it may take a couple of procedures, PRK can help these patients too.
“The post-PK patient is kind of why I initially abandoned LASIK for post-transplants,” says Dr. Majmudar. “This cornea behaves differently biomechanically than the normal one. When you’re making flaps, you cut through the patient’s portion of the cornea, the interface of the transplant, and then the donor cornea, a process which will yield variable results. The other issue is that the refraction can be limited because these patients often have higher amounts of astigmatism, which in many cases may be irregular. This means it’s not a crisp, symmetrical bow-tie pattern that would refract very well. Because of this, you have to look at many parameters when planning any kind of refractive correction. You should probably err on the side of undercorrecting in order to avoid shifts in outcome. I’ve found that Scheimpflug-type imaging isn’t very useful in the post-PK patient. Instead, I get a lot more information on the post-transplant cornea from placido-based topography. Topography gives me a better understanding of what the true astigmatism is, which may not be reflected in the refraction you get from a phoropter.
“The way wavefront aberrometry is in the United States now, it’s really for normal eyes,” continues Dr. Majmudar. “I’m not sure that an irregular eye, such as a post-transplant patient’s, would yield that much data on a wavefront. In the end, you can get a wavefront map, and combine that information with data from your other instruments, and develop your own internal nomogram that involves cutting back on some of the treatment. Of course, depending on the laser system used, you may not be able to treat all the astigmatism and would need to back down the correction anyway. I’d suggest trying to normalize the astigmatism on the surface as much as you can. That way, it might be easier to get a glasses’ prescription or a contact lens fit. In these patients, you have a different endpoint; it’s not necessarily 20/20 vision like someone who’s never had any kind of eye surgery before. Your mindset and the patient’s mindset have to change, a concept that goes back to counseling, managing expectations and all those sorts of patient education issues that we talk about with refractive procedures.”
Dr. Rootman plans the procedure based on the amount of astigmatism.
“If it’s greater than 6 D, I’d precede PRK with an Intralase-assisted astigmatic keratotomy to minimize the amount of surface ablation necessary,” he explains. “Once the keratotomy is healed, which will be in about two to three months, I’ll proceed with the PRK.”
|
During the PRK itself, the presence of the graft-host junction may call for a slightly altered approach. “Just like it’s important to be careful when removing the epithelium over the RK wounds in the post-RK patient, I try to be gentle over the graft-host junction in the post-transplant patient,” says Dr. Yoo. Dr. Majmudar thinks this is an important point. “If someone has a lot of astigmatism, you want to make sure the graft-host junction is even and smooth,” he says. “When we remove the graft sutures in the early postop period, there may be an override so that the junction isn’t a flat surface but more of a step. You have to be careful in those cases because, first, this step is causing astigmatism. Second, the graft-host interface may be somewhat weakened in that area. Of course, you also want to be confident that all the sutures are out for a long enough length of time so that you have achieved refractive stability before you plan your treatment. You also have to allow enough time to pass after the transplant so as not to threaten the integrity of that wound.”
Since the post-PK patient has a lot of issues that could make the PRK more challenging, Dr. Majmudar has used mitomycin in the cases that he has done. “You’re dealing with a situation in which the biomechanical properties aren’t quite normal,” he says. “So, mitomycin may be helpful in preventing scar and haze formation.”
Ultimately, Dr. Majmudar says, at least in the case of post-premium lens patients, the best PRK is the one you never even have to do. “About five or six years ago, a lot of premium lens surgeons weren’t so meticulous about the refractive result of the cataract surgery, especially if they didn’t have a refractive surgery background,” he says. “But at our practice, we’ve always had more of a refractive mindset when it comes to cataract surgery, and I think that’s helped us not have a high rate of enhancement.”
REVIEW