The survey was emailed to 4,142 U.S. members of ASCRS, and 11 percent, or 452 surgeons, responded. Here’s a look at the highlights.
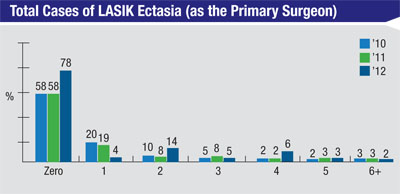
Ectasia Rates
Mobile, Ala., ophthalmologist Richard Duffey, who administers the survey each year with Palm Springs, Calif., ophthalmologist David Leaming, finds the ectasia results significant and encouraging. “It’s really important,” he says. “Seventy-eight percent of surgeons haven’t seen a case of ectasia of their own. This is because as newer, younger surgeons come in and adopt our more conservative approach to surgery and better diagnostic testing, they’re not operating on patients who have a greater likelihood of developing ectasia, just like more experienced surgeons won’t. I also think we’ll see the number of ectasia cases drop further and further as time goes by because of our improved diagnostic skills and more conservative thinking regarding such factors as the residual stromal bed.”
Part of the post-LASIK ectasia equation consists of such factors as corneal and residual stromal bed thicknesses, which the survey also inquired about. “Looking at the results from the survey’s question on the minimum corneal thickness a surgeon would operate on, 58 percent of the respondents would operate on corneas 480 µm thick or less,”
|
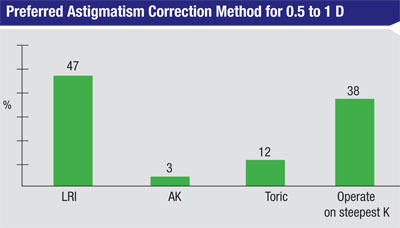
Managing Astigmatism
This year’s survey revealed that surgeons are pretty aggressive in terms of when they offer to correct astigmatism.
Forty-seven percent of surgeons will offer to correct a patient’s astigmatism when it reaches 0.75 D, and 78 percent offer to correct it when it’s at 1 D or higher. “I think we’re better at correcting astigmatism now,” says Dr. Duffey, suggesting a reason for the propensity of surgeons to offer astigmatism correction. “We can do limbal relaxing incisions and astigmatic keratotomy incisions better than we ever could before, and the presence of toric lenses makes surgeons feel more comfortable with managing astigmatism, as well. Also, the fact that you can be reimbursed by the patient for managing the astigmatism gives surgeons an incentive to get better at astigmatic correction and offer it to patients if it’s something that’s important to them.”
In terms of the astigmatic procedures surgeons prefer for low levels of astigmatism (0.5 to 1 D), 47 percent like LRIs, 38 percent prefer to operate on the steep meridian, 12 percent use toric lenses and 3 percent prefer AK. For moderate astigmatism (1.12 to 2 D), the percentage of toric IOL backers jumps to 74 percent, with 22 percent preferring LRIs. For astigmatism greater than 2 D, 94 percent of surgeons say they prefer toric lenses.
Procedure Preferences
Dr. Duffey points out that, even though LVC volumes are going down, PRK remains a popular option.
“We’re on a downward slide for LVC but, as a ratio, PRK is a fifth of all LVC, which is up from 12 percent in 2005,” Dr. Duffey says. “The reason for this is simple: If we have any doubt regarding the risk of ectasia or complications, we’re going to fall back more on PRK than on LASIK. I see this in my own practice. For patients on whom I would have done LASIK five years ago, if I see something out of the ordinary—even if it’s minimal like a 475-µm cornea or a very high myope whose postop stromal bed would be a little thinner than 300 µm—I’ll do PRK on that patient.
 |
The survey is also beginning to show that there’s a percentage of surgeons who are tolerant of other surgeons’ decision to perform bilateral, simultaneous intraocular surgery, which has historically been taboo. When asked if they’ve performed such a procedure, 24 percent say they have with phakic intraocular lenses, but only 9 percent say the same regarding refractive lens exchange. Seventeen percent have done it for corneal inlays. “This is not to say that these surgeons do these procedures routinely,” says Dr. Duffey. “They’re basically saying that they won’t protest if a surgeon thought it was the right way to do it. The higher rate for phakic IOLs is because they’re less invasive than refractive lens exchange. In P-IOL surgery, you’re not removing the patient’s crystalline lens, so there’s less risk of macular edema and retinal detachment, though there’s no less risk of infection. So there’s a little bit less of a risk with a phakic IOL implantation than there is when you’re removing the lens and placing an implant.”
Though procedure volumes are down, Dr. Duffey takes comfort in knowing that refractive surgeons still believe in refractive surgery procedures, based on how many have had it themselves. A quarter of the respondents have had refractive surgery, 56 percent say their siblings have had it and 28 percent of the surgeons say their spouses have had LVC. “When you see these rates, which have consistently stayed high, it tells you that we who know the most about the procedures, refractive surgeons and our families, have had them done at a higher rate than the general population,” notes Dr. Duffey. “It’s kind of an index of satisfaction. If you saw that, suddenly, no surgeons we’re having it done on their own eyes, then there would have to be a better alternative. Right now, though, there’s no better alternative than LVC.” REVIEW