Navigating intraocular lens calculation in patients with atypical eyes presents a unique challenge for cataract surgeons. Since these eyes deviate from the norm, standard formulas aren’t sufficient to factor in the many anatomical differences. In this article, experts discuss how the latest formulas can help surgeons achieve accurate IOL power calculation in eyes with keratoconus, post-refractive eyes and eyes with extreme axial lengths.
Modern Formulas
Variations in ocular anatomy impact the accuracy of traditional formulas. Experts say that the newer-generation formulas available today, which incorporate more anatomical parameters, are helping surgeons get closer to their targets. “When you have an average eye with normal axial length and normal Ks, all the formulas seem to work well and converge into a good number,” says William B. Trattler, MD, of Bascom Palmer Eye Institute. “But as the axial length increases or shortens, there’s more opportunity for errors in the formulas because the anatomy isn’t always the same.
“The effective lens position can differ more in unusual eyes,” he continues. “For example, a shorter eye could still have a normal anterior chamber depth and therefore the lens is back a bit farther. Or, you could have a patient with a short axial length and a very narrow anterior chamber, and therefore the effective lens position after surgery will be farther forward, closer to the cornea. The modern formulas that take into account other parameters such as anterior chamber depth, corneal shape and keratometry, for example, are more likely to be on target because they’re using multiple anatomical features to try to estimate where the effective lens position will be after surgery.”
Unusual eyes typically include those with unusual corneas—such as keratoconus or post-refractive eyes—and those with unusual axial lengths. “There are specialized formulas that have been developed for each of these scenarios,” Dr. Trattler says. “Many biometers have some of the formulas integrated into them. For example, the Argos and IOLMaster700 both have formulas integrated for the post-LASIK patients. You have to select whether it’s post-myopic or post-hyperopic LASIK. Then, you just toggle that and get the integrated printout. There’s no risk of transcription errors this way.”
Preoperative Measurements
Precise imaging is a crucial step for ensuring accurate IOL power calculation, particularly in unusual eyes. Divya Srikumaran, MD, of the Wilmer Eye Institute at Johns
Hopkins University, says that all of her patients with corneal problems who are having cataract surgery undergo corneal tomography with Pentacam, in addition to biometry with a LenStar or IOLMaster. “[Corneal tomography] gives us information about the regularity of the patient’s astigmatism and total corneal power,” she says. “It’s especially helpful for patients who are post-refractive surgery or who have keratoconus. Tomography is critical.”
“For imaging of patients [with unusual eyes], I typically like to have a Placido disc-based topography as well as Scheimpflug tomography (Pentacam),” says Rahul Tonk, MD, MBA, of Bascom Palmer Eye Institute. “I prefer to have two separate instruments looking at the corneal shape and curvature. I also like to have an IOL biometry device such as the IOLMaster700, which measures total keratometry, and preoperative OCT of the retina to evaluate for any posterior segment pathology that might limit certain IOL choices.”
Addressing any ocular surface issues, such as dry eye and meibomian gland dysfunction, before obtaining preoperative measurements helps to ensure accurate assessments and successful outcomes. “We’ve all come to recognize the importance of making sure that the ocular surface is optimized,” Dr. Srikumaran says. “[The ocular surface] impacts astigmatism measurements and the outcomes of all of our keratometry readings, which can have a significant impact on IOL calculation. I can’t understate the importance of that. If the ocular surface isn’t optimized prior to your measurements, don’t hesitate to repeat them.”
Dr. Trattler agrees. “I’m a big fan of doing a second measurement. I don’t do it for every case, but if patients have unusual anatomy or keratoconus or are post-LASIK, their measurements can be more aberrant. We typically treat patients for some presumed ocular surface disease, which is quite common, and bring them back for a second set of readings. They get two sets of readings because we think there may be some variability in the keratometry.”
Keratoconus
There are three challenges with keratoconus eyes, according to Dr. Tonk. “One is that there’s an altered anterior-posterior corneal curvature ratio,” he explains. “In most devices, the front surface of the cornea is measured and then some standard index is used to predict the characteristics of the posterior cornea. In an eye with keratoconus, and in any eye with an abnormal cornea, that ratio is altered. So, the assumption that you can predict the posterior cornea based on the anterior cornea using a standard index, gets thrown out. These eyes are more prone to refractive surprises because of that altered ratio.
“The second challenge of keratoconus eyes is the effective lens position prediction error, since traditional methods of estimating ELP may fall short in these unusual corneas. The third challenge is the difficulty in obtaining accurate measurements of true central corneal power,” he continues. “The combination of all three of those things typically leads to very reduced refractive accuracy, and frequently, hyperopic surprises for patients.”
 |
|
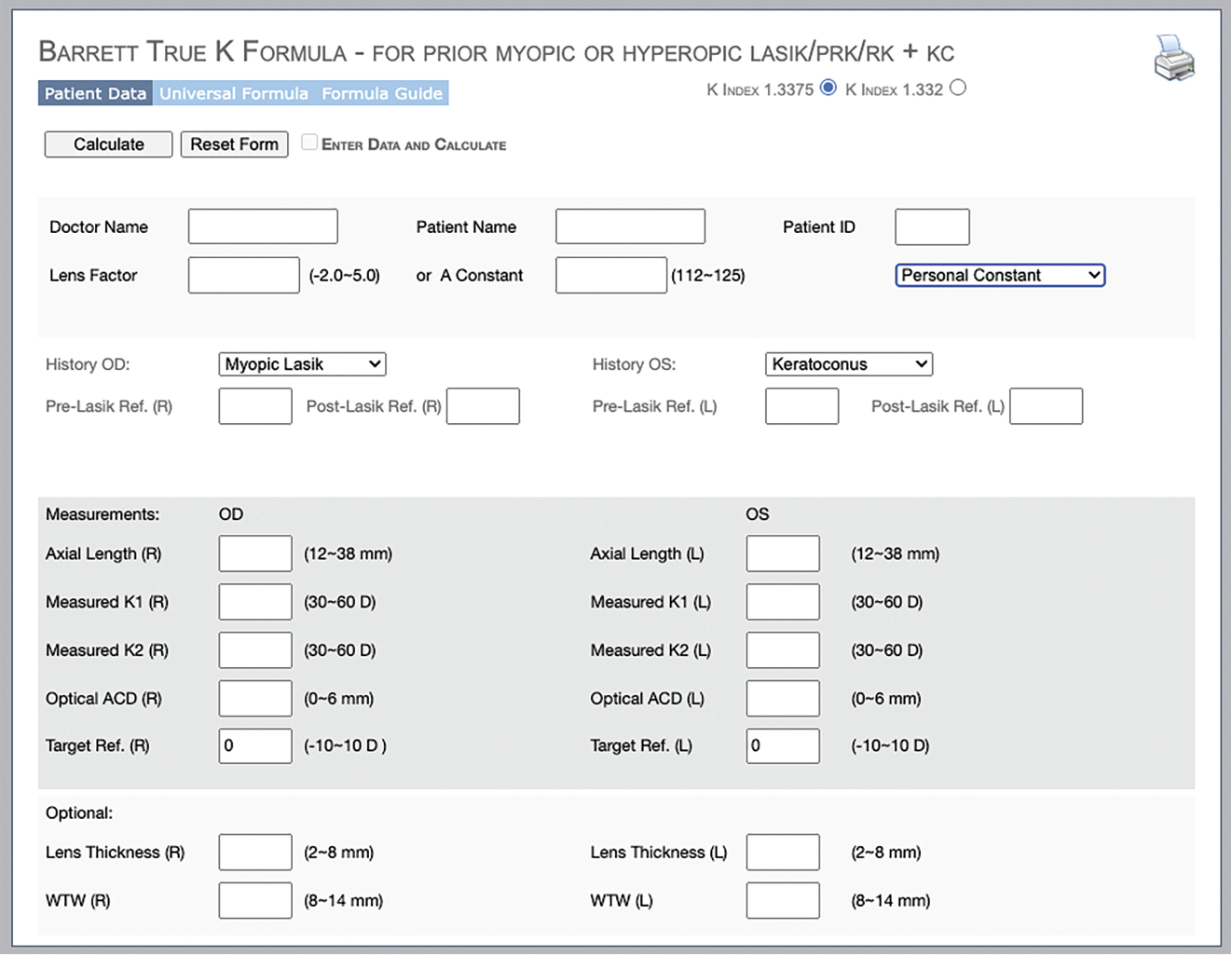
The Barrett True K formula is one of the most up-to-date formulas for keratoconus. Photo: APACRS.org |
Experts say that one of the best tools surgeons can use when calculating IOL power in keratoconus eyes is to use the most recent keratoconus formulas: the Barrett True K and Kane Keratoconus. “Up until about five years ago, the long-standing SRK/T formula seemed to be the best in keratoconus, but in recent years, we now have keratoconus-specific formulas, and they’re the most accurate,” says Tal Raviv, MD, of Eye Center of New York. “They can be found online for free (see sidebar “Links to Online Formulas”). You just check off the keratoconus box, put in the case, and those are your best chances of coming pretty close.
| Links to Online Formulas |
| • Barrett True K • Kane KCN • ESCRS Calculator |
“Studies show that with Ks up until 50, you can target a little bit below plano and will usually do pretty well with those formulas,” he continues. “But once you go above 50, even the best keratoconus formulas start to fall short. I usually target more myopia the higher the Ks are, just to err on the side of myopia and not hyperopia. That’s my trick for keratoconus.”
It’s important that surgeons know about these new formulas, stresses Dr. Tonk. To enhance calculation accuracy, he uses the IOLMaster’s total keratometry measurement. Dr. Tonk, who has no financial interest in Zeiss, says “total keratometry measures the curvature of both the front and the back surface of the cornea directly, rather than just measuring the front surface and predicting the back surface. The developments of new formulas that take total keratometry into account have really improved our refractive accuracy for patients with keratoconus.”
 |
|
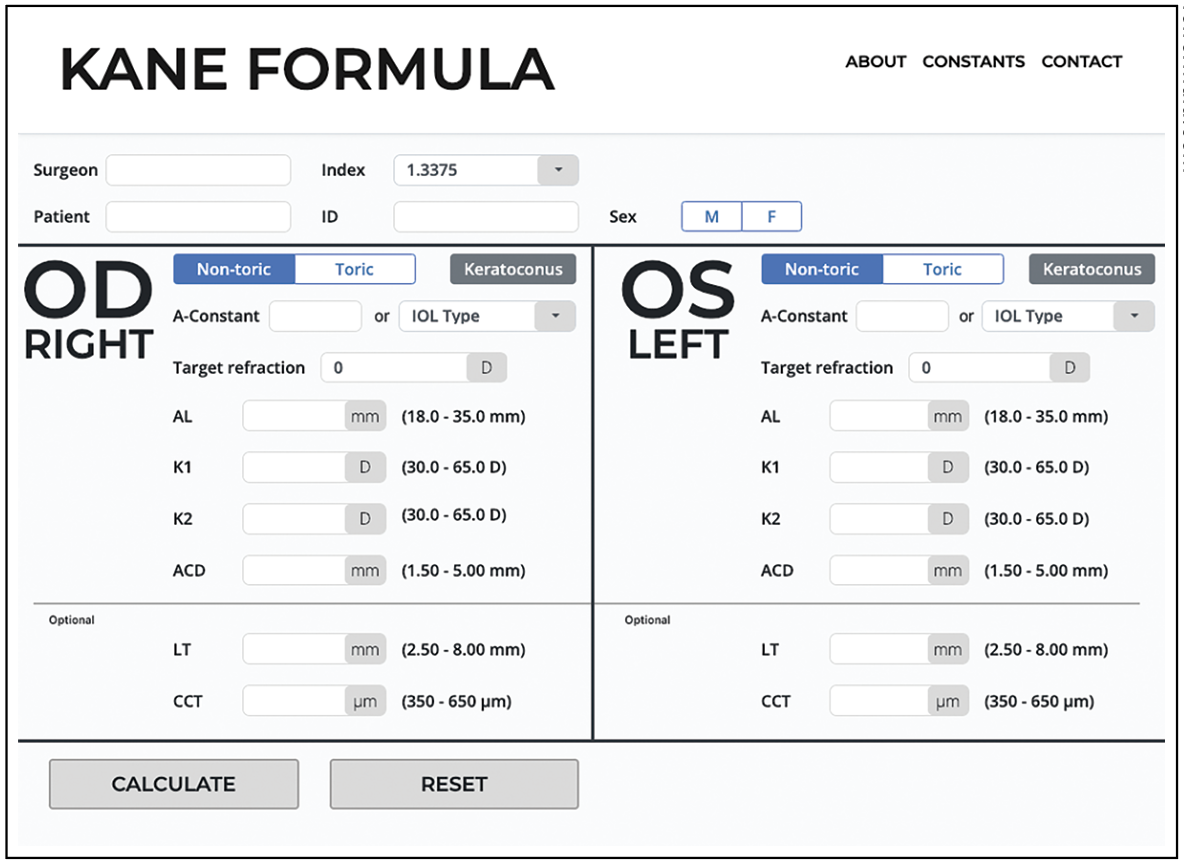
Experts caution that when using total keratometry in formulas such as the Kane Keratoconus, the anterior and posterior corneal values must be inputted separately. Photo: iolformula.com. |
In a 2023 multicenter study1 of 87 eyes of 67 patients with keratoconus by Dr. Tonk and his colleagues, the Barrett True K with total keratometry (measured posterior corneal astigmatism) achieved 35.4 percent of eyes within 0.5 D and 72.7 percent within 1 D, which was significantly better than formulas that used standard keratometry (predicted posterior astigmatism) alone. The group reported that without total keratometry, Barrett True K-K performed reasonably well, as did the Kane Keratoconus-K for eyes with severe keratoconus (steep K < 50 D).
“If you have total keratometry, then your very best option across the board is to use the Barrett True K-TK,” Dr. Tonk says. “Not everyone has total keratometry, however, so if you don’t have it, you can use the Barrett True K with standard keratometry.”
He adds it’s important to note that you can’t substitute total keratometry values for standard keratometry values in online calculators. “If you’re going to use total keratometry, you have to separately input the anterior corneal values, i.e., your standard keratometry, and separately input your posterior corneal values, which are on a separate column of the IOLMaster device.”
Many surgeons run their calculations through multiple formulas and compare them. “We tend to get hyperopic errors in keratoconus patients, and these errors aren’t well tolerated,” explains Dr. Srikumaran. “These patients are used to being very myopic their entire lives and it’s quite disturbing to suddenly end up hyperopic. I compare all the formulas and then take the highest power IOL because that’s going to have less chance of ending up with a hyperopic error. I’d rather err on the side of myopia. There isn’t always agreement [among the formulas] unfortunately, because they all have different strategies for adjusting for corneal power.”
Surgeons say that when it comes to IOL selection in keratoconus patients, their preferred lenses include the Light-Adjustable Lens, small aperture IOLs and monofocals. “If the patient’s astigmatism is regular and they’ve had stable corneas for years and aren’t wearing RGPs, I try to treat the astigmatism,” says Dr. Raviv. “For keratoconus patients wearing glasses, any reduction in astigmatism is helpful, so I do believe in using monofocal torics for keratoconus. In irregular keratoconic eyes, we can consider small aperture IOLs, but I’m hesitant to use these lenses in very irregular keratoconic eyes with 7 or 8 D of astigmatism because that pinhole optic is still not enough to address all that.”
Dr. Raviv says the Light-Adjustable Lens is another good option, with “the limitation that we can only adjust maybe 1 or 2 D, maximum
3 D of astigmatism postop. We want to use it in keratoconic eyes that are going to be within that range—not the super high astigmatic ones, at least not by itself. There are a few surgeons who do piggyback IOLs with LALs and other lenses, but we aren’t yet sure how efficacious that is in the long term. All the issues of piggyback lenses come into play when we do that, including interlenticular opacification and iris chafing if the lens is put in the sulcus.”
“For keratoconus, I typically use a neutral asphere monofocal lens,” says Dr. Trattler. “The LAL is my other go-to.”
Post-refractive Eyes
As with keratoconus, the latest formulas tailored for post-refractive eyes, including the EVO 2.0, Barrett True K, Pearl DGS and Hoffer QST, seem to offer the most accuracy, surgeons say. “We’ve found that the combination of one of these modern formulas and total keratometry is the best way to predict IOL power for patients who have had myopic laser vision correction,” says Dr. Tonk, citing a 576-eye study he and his colleagues published this year.2
“The best formulas for 2024 for predicting IOL power in post-myopic LVC patients are the EVO 2.0 with posterior keratometry (PK), the Barrett True K-TK and the Pearl DGS-PK. All three of these formulas are new and all three involve posterior or total keratometry,” he says.
“If you don’t have total keratometry, you can still use some of these new formulas with standard keratometry,” he continues. “In those situations, the top two formulas were the Pearl DGS-K and the EVO 2.0-K, which were statistically significantly better than the Barrett True K No History (NH)-K or the Barrett True K-K.”
Dr. Tonk presented an abstract at this year’s ASCRS meeting on 153 post-hyperopic LVC eyes as well. “We found that when using total keratometry, the Barrett True K-TK and EVO 2.0-PK performed the best,” he says. “Without total keratometry, the EVO 2.0-K and Barrett True K-NH are reasonable performers.”
In eyes with prior radial keratotomy for myopia, the Barrett True-K NH and the ASCRS Maximum power were found to be more accurate than the Humphrey Atlas method, IOLMaster/Lenstar method and ASCRS Average power formulas, according to a 2023 retrospective study3 of 25 eyes that compared the accuracy of IOL power prediction of the formulas available on the ASCRS’ post-refractive calculator.
“The LAL gets the patient all the way to the finish line in these eyes that are more difficult to calculate,” says Dr. Trattler. “I use this lens for most of my patients with a history of previous LASIK now, as well as for post-RK patients.”
Dr. Raviv says that in addition the LAL, he likes to use EDOF lenses such as the Symfony OptiBlue, in post-refractive eyes. “It’s hard to reach exactly plano in these eyes with a standard, non-adjustable lens, so we want to go with one that’s forgiving,” he says.
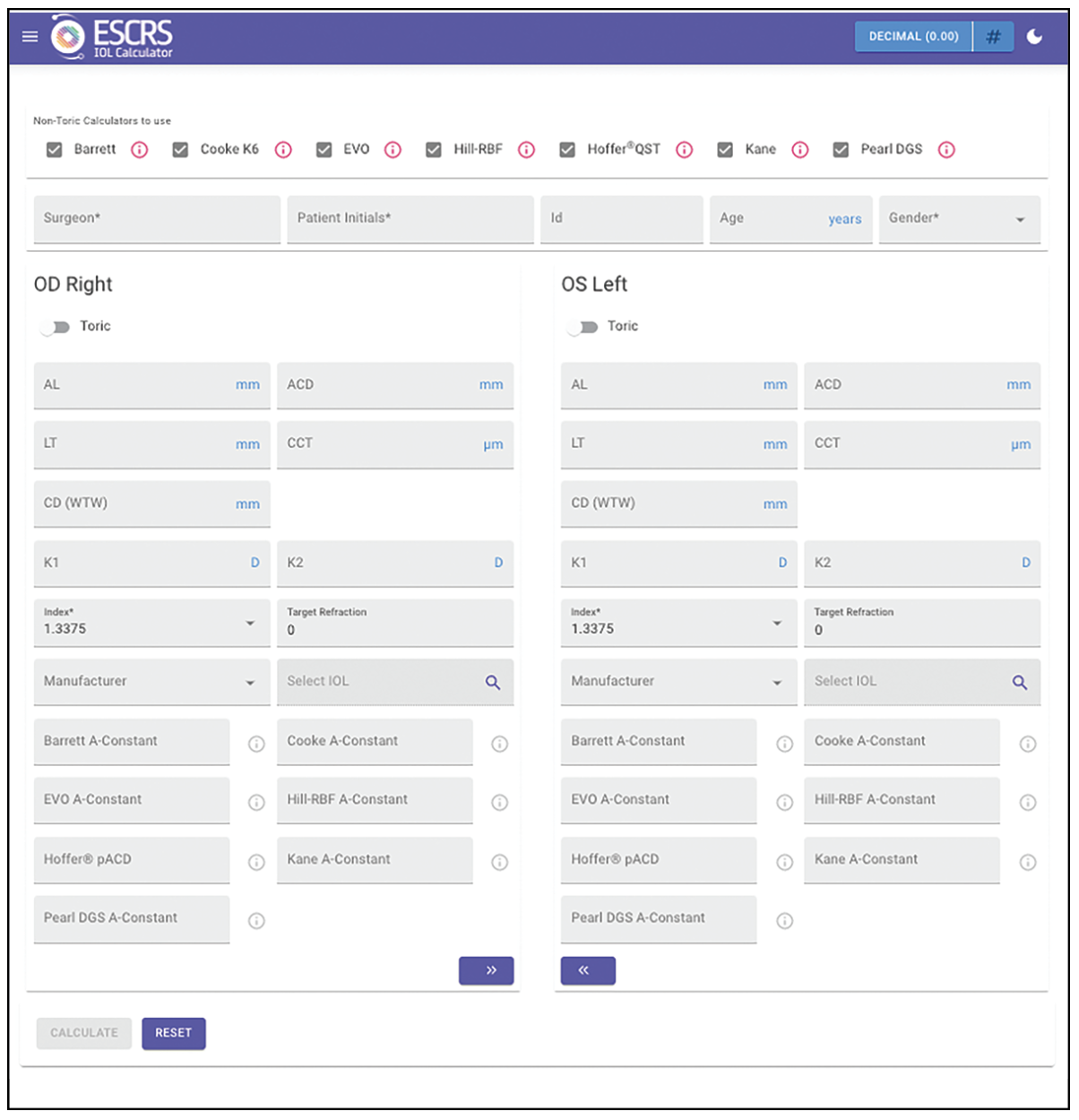 |
| Surgeons can compare the outputs of multiple formulas using the European Society of Cataract and Refractive Surgery’s online calculator. Experts advise choosing the result that leaves the patient either plano or with slight myopia. Photo: ESCRS. |
Extreme Axial Lengths
“For extreme axial lengths, but especially long eyes, one of the big challenges is getting an accurate measurement,” says Dr. Srikumaran. “Sometimes patients have staphylomas, and if they have poor vision, they also have poor fixation. It’s important to try to get the optical biometry when you’re confident that you’re getting good fixation in the fovea. The IOLMaster700, which shows you where it’s fixating on the fovea, can be very helpful.
“Also be sure to recognize when you have an error in your measurements,” she continues. “Some of these really long eyes, for example, may have been vitrectomized or have buckles if they’ve had prior retinal problems, and those can throw off your measurements. That’s something to keep in mind as you’re doing your measurements.”
Dr. Srikumaran asys her favorite formula is the Barrett Universal II for long and short eyes. “I also really like the Hill RBF formula,” she says. “Over the years, it’s expanded. Before, there were cut-offs and you couldn’t do extreme axial lengths, but now if there’s an expanded range available, you can do the Hill RBF calculator as well on the ASCRS site. I like to compare formulas and make a decision.”
Today’s formulas for long and short eyes are much better, Dr. Trattler says. “I feel very comfortable using Barrett [Universal II] in shorter eyes as well as longer eyes now.”
“Some of the best formulas for very long or very short eyes are the newer generation formulas that many of us don’t have on our biometers,” Dr. Raviv says. “The Pearl DGS, EVO, Hoffer QST and Kane formulas are excellent formulas for long and short eyes. The SRK/T, Holladay and Hoffer fall short in 2024.
“Short eyes are some of the most challenging eyes to calculate because as we go up in power, the lens implants that we use are in the 30-D range and we have less predictable effective lens position,” Dr. Raviv continues. “Even a millimeter forwards or backwards from that plano positioning of these IOLs can affect the refractive outcome. So, these are the most challenging eyes, and for these eyes, I use the latest formulas on the ESCRS website.”
When consulting the various outputs of the different formulas on the ESCRS website, Dr. Raviv says he looks at all the results and picks the one that will leave the patient either plano or with slight myopia. “For example, in a very high myope, I’ll choose one that is either plano or at worse minus 2, as opposed to plano or plus 2.
“On the hyperopic side, it’s a little trickier,” he adds. “For these patients, patient education is going to be key. It’s good for them to be aware that the smaller axial length, the more the residual refractive error. I sometimes show them the formulas we have on the screen, so they understand how each one shows a different lens. That lets them know that we’re going to get as close as we can. If the LAL is an option, then they understand why the LAL exists, and they may opt for that if they’re really particular or want the best chance of reaching a specific refractive target. I also use ORA in these very long or very short eyes. I find it helps sometimes, but it doesn’t predict ELP.”
“Even with the more advanced formulas, the standard deviation is higher than for normal patients,” Dr. Trattler says. “So, we’re still not as accurate in these unusual eyes. That’s why we consider options like the LAL or discuss with patients that we may need to do a piggyback lens or IOL exchange if it’s not on target.”
Dr. Raviv is a consultant for Johnson & Johnson. Dr. Trattler is a consultant for RxSight, Johnson & Johnson, Bausch + Lomb, Rayner and Zeiss. Dr. Srikumaran and Dr. Tonk have no related financial disclosures.
1. Heath MT, Mulpuri L, Kimiagarov E, et al. Intraocular lens power calculations in keratoconus eyes comparing keratometry, total keratometry, and newer formulae. Am J Ophthalmol 2023;253:206-214.
2. Anter AM, Bleeker AR, Shammas HJ, et al. Comparison of legacy and new no-history IOL power calculation formulas in postmyopic laser vision correction eyes. Am J Ophthalmol 2024;264:44-52.
3. Shetty N, Sathe P, Aishwarya, et al. Comparison of intraocular lens power prediction accuracy of formulas in American Society of Cataract and Refractive Surgery post-refractive surgery calculator in eyes with prior radial keratotomy. Indian J Ophthalmol 2023;71:9:3224-3228.




