The patient was diagnosed with bilateral chorioretinitis and retinal vasculitis with ellipsoid layer alterations. Given his clinical history and examination, the differential diagnosis consisted of infection (syphilis, tuberculosis, Lyme disease); inflammatory diseases (sarcoidosis, granulomatosis with polyangiitis, birdshot chorioretinopathy); paraneoplastic syndromes; lymphoma; and multiple sclerosis.
Laboratory workup revealed a positive syphilis antibody and rapid plasmin reagin (RPR) at a titer of 1:128. HIV, Lyme, HLA-B27 ACE, ANA, ANCA and Quantiferon Gold were negative. The patient was diagnosed with acute syphilitic posterior placoid chorioretinitis (ASPPC), and admitted to the internal medicine service for treatment with intravenous penicillin 4 million units every four hours for 14 days. Lumbar puncture during admission was significant for negative Venereal Disease Research Laboratory testing. CSF protein was 35 mg/dL and glucose 69 mg/dL.
After treatment with penicillin, the patient had improvement in vision to 20/25 in the right eye and 20/20 in the left. Fundus photographs showed bilateral improvement in the yellow placoid lesions in the posterior pole (See Figure 4a, 4b). Follow-up SD-OCT scans demonstrated resolution of the retinal pigment epithelium nodularity and improved clarity of the inner segment-outer segment junction (See Figure 5).
Discussion
Acute syphilitic posterior placoid chorioretinitis is a variant of syphilitic chorioretinitis. It is characterized by one or more outer retinal yellow, circular, placoid, lesions usually found in the macula.1 The term ASPPC was first described by Donald M. Gass, MD, and colleagues, who postulated that this disease is caused by Treponema pallidum organisms entering the choroidal circulation to gain access to the outer retina.2
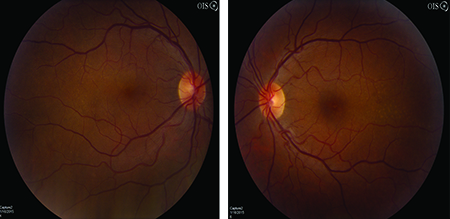 |
| Figure 4a and Figure 4b. Fundus photos OD and OS after intravenous penicillin therapy demonstrating resolution of placoid macular lesions. |
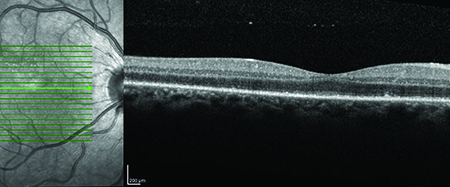 |
| Figure 5. SD-OCT of the left eye after IV penicillin therapy showing resolution of RPE nodularity and improved clarity of the inner segment-outer segment junction. |
SD-OCT findings in ASPPC show outer retinal abnormalities, which may include disruption of the inner segment/outer segment junction, nodular thickening of the retinal pigment epithelium, or loss of RPE/outer segment junction. In some cases patients may have loss of the external limiting membrane and accumulation of subretinal fluid.3 Fluorescein angiography typically shows hypofluorescence or faint hyperfluorescence in the early phase, with mid- and late-phase FA usually exhibiting progressive hyperfluorescence.1,4
Laboratory evaluation for ASPPC should include initial qualitative treponemal antibody assays (enzyme or chemiluminescent immunoassays) as the initial screening test. Positive tests are followed by non-treponemal RPR testing, which may then be used to quantify response to treatment.6 Testing for HIV status, if unknown, should be obtained due to the high rate of co-infection and the possibility of accelerated progression to neurosyphilis in HIV-positive patients.6 Although HIV has a high co-infection rate with syphilis, it does not appear to influence response to antibiotic therapy.1 Once confirmed, treatment with parenteral penicillin G should be initiated. Angiographic and OCT findings are mostly reversible with appropriate therapy with IV antibiotics.1,3,4 Our patient demonstrated a similar reversal of findings, with improvement in fundus appearance and OCT after antibiotics. One recent case study reported the possibility of spontaneous resolution of ASPPC.7 However, due to the sight-threatening and systemic manifestations of syphilis, antibiotic therapy remains a critical component of patient care.
Between 2005 and 2013, the number of reported cases of primary and secondary syphilis cases increased from 2.9 to 5.3 cases per 100,000 people, with men accounting for 91.1 percent of cases.8 As the frequency of early syphilis rises, ophthalmologists may be confronted with more cases of syphilitic uveitis.6 Although ASPPC is an unusual manifestation of syphilis, it is critical to maintain a high index of suspicion in this rare but distinct manifestation of ocular syphilis and to initiate appropriate therapy promptly. REVIEW
1. Eandi CM, Neri P, Adelman RA, et al. Acute syphilitic posterior placoid chorioretinitis: Report of a case series and comprehensive review of the literature. Retina 2012;32:1915-1941
2. Gass JDM, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology 1990;97:1288-1297.
3. Pichi F, Ciardella AP, Cunningham ET Jr. Spectral-domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinitis. Retina 2014;34:373-384
4. Brito P, Penas S, Carneiro A. Spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis: the role of autoimmune response in pathogenesis. Case Rep Ophthalmol 2011;2:39-44
5. Veys MC, Lafaut B. Ocular syphilis, a case of acute posterior placoid chorioretinitis. Bull Soc Belge Ophthalmol 2013;322:21-25.
6. Davis JL. Ocular syphilis. Curr Opin Ophthalmol. 2014;25(6):513-8.
7. Aranda S, Amer R. Sequential spontaneous resolution of acute syphilitic posterior placoid chorioretinitis. Eur J Ophthalmol. 2015; 25(3):263-5.
8. Patton ME, Su JR, Nelson R, Weinstock H;Centers for Disease Control and Prevention (CDC). Primary and secondary syphilis--United States, 2005-2013. MMWR Morb Mortal Wkly Rep 2014;63(18):402-6.



