Patients undergoing cataract surgery have higher expectations than ever for their visual outcomes. When those patients have astigmatism, the current correction method of choice is toric IOLs; however, there’s no toric IOL for the correction of astigmatism <1 D approved in the United States. In this situation, surgeons find themselves turning to long-established intraoperative techniques, such as limbal relaxing incisions, to give patients the best vision possible. Here, experts share their techniques and tips for a successful outcome.
Why LRIs Still Matter
“In the U.S., the lowest power toric lenses, which are great for addressing astigmatism, only correct about 1 D at the corneal plane,” notes Uday Devgan, MD, a refractive and cataract surgeon practicing in Los Angeles. “If the patient has 1 to 2 D of astigmatism in the cornea, by all means put a toric lens in. But what do you do when the patient has 0.5 D of astigmatism or 0.75 D of astigmatism? You don’t want to leave them uncorrected.”
IOL affordability could also contribute to the decision to perform LRIs. “If you can convince all your patients to have some type of toric lens, you’ll never have to do an LRI,” says Jeffrey Whitman, MD, chief surgeon at the Key-Whitman Eye Center in Dallas. “However, we have a wide range of patients and perform over 7,000 cataract surgeries in our surgery center each year. We have patients who can’t afford premium toric lenses or presbyopia-correcting lenses. We offer financing options as needed, but also remember that there are patients for whom premium lenses just aren’t right. There are patients who have bad macular degeneration, so a multifocal lens doesn’t make sense. If they choose a monofocal lens, that’s not an excuse not to offer them a better quality of vision and fix low amounts of astigmatism. Give them the best visual outcome that they can afford.”
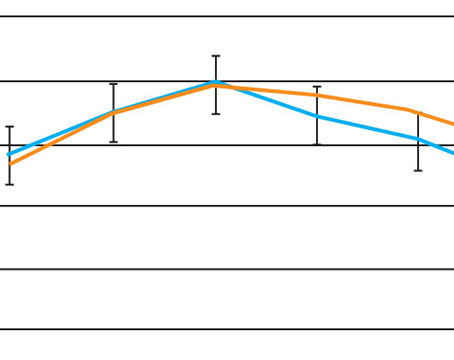
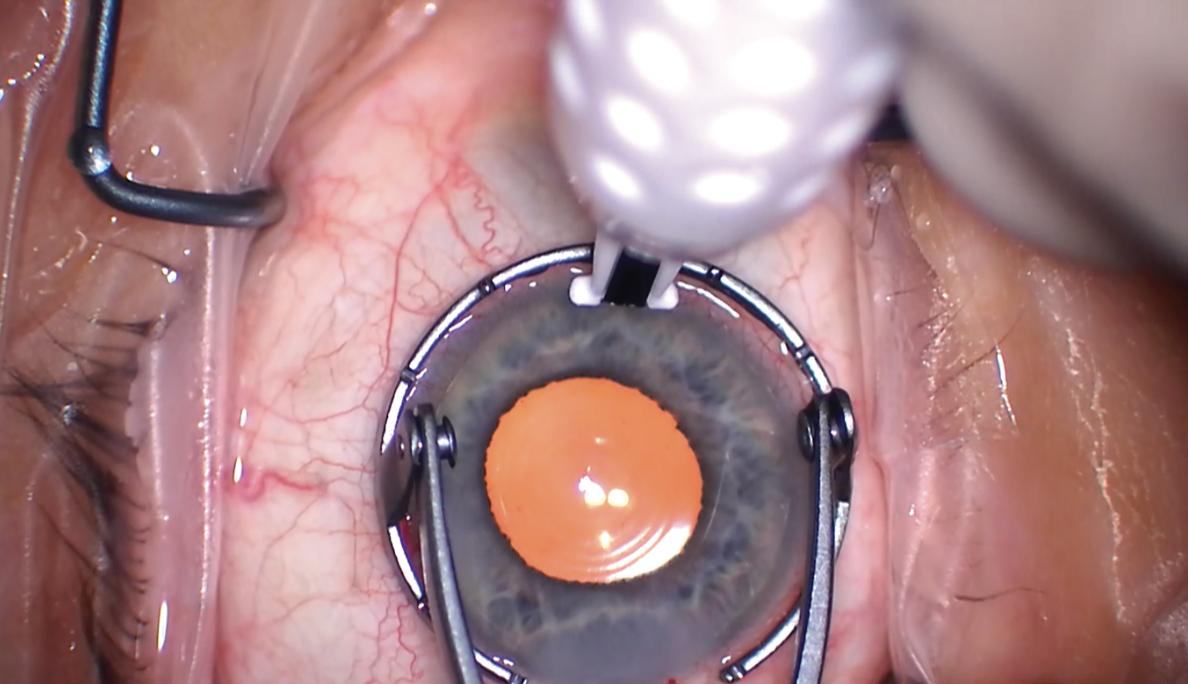
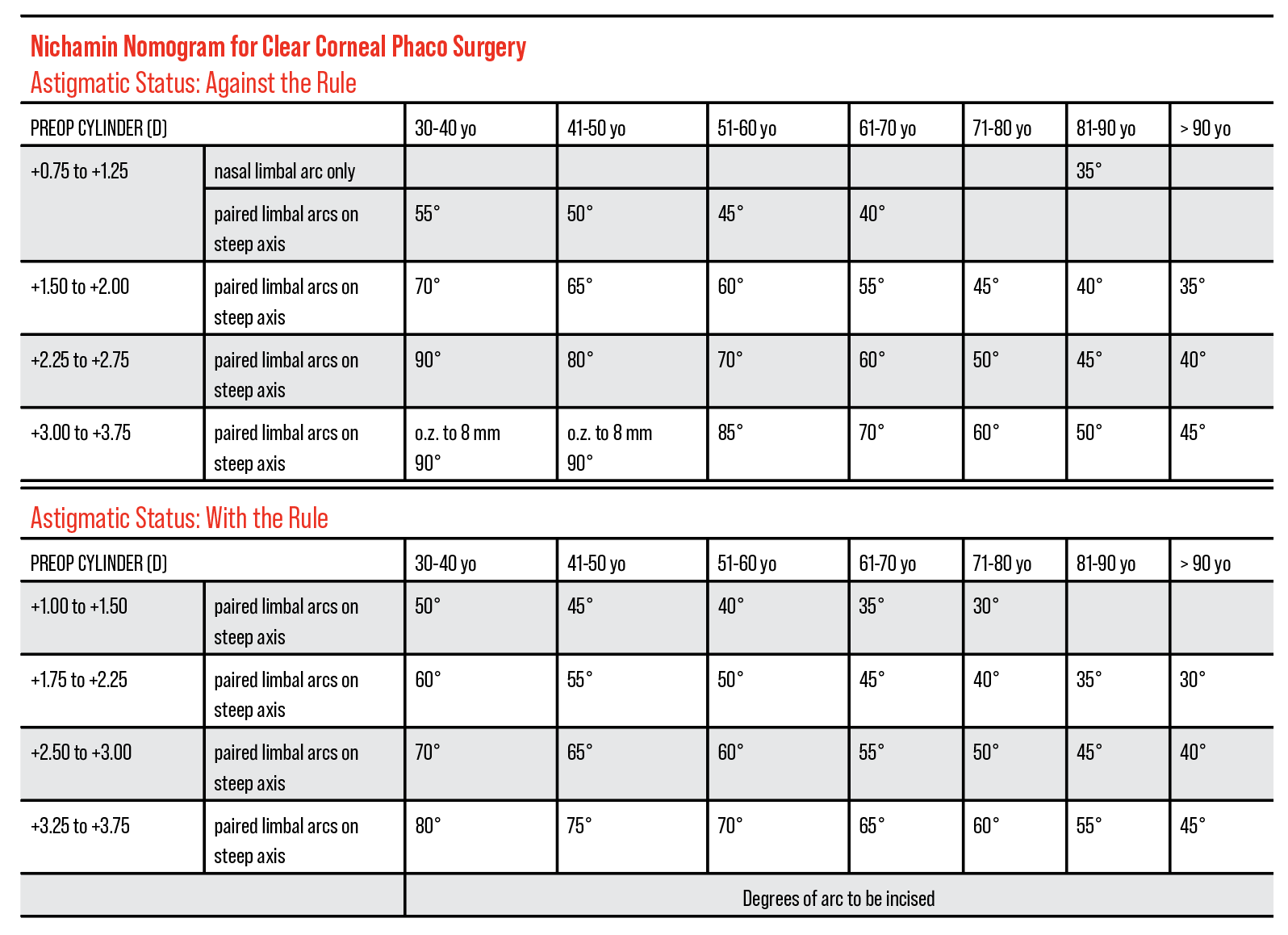 |
| The Nichamin nomogram is widely used for LRIs and accounts for the patient’s age in determining the degrees of arc to incise. It assumes the temporal incision is first made by creating a two-plane grooved phaco incision (600 μm depth), which is then extended to the appropriate arc length at the conclusion of surgery. (Courtesy of Uday Devgan, MD). Click image to enlarge. |
Screening Patients for LRI Candidacy
It’s important to recognize who best fits the profile for an LRI.
“Ideal candidates will have regular symmetric astigmatism,” says Dr. Devgan. “If it’s irregular, it’s not worth trying an LRI. The ideal candidate is a patient, who again, in this situation has less than 1 D of astigmatism. If they have more than that, LRIs lose their efficacy above a certain degree. I won’t even attempt an LRI for 2 or 3 D of astigmatism. It’s just not really feasible, whereas I can put a toric lens to correct 4 D of astigmatism very accurately.
“Candidates to avoid would be those with irregular astigmatism, a high degree of astigmatism or some other irregularity in the cornea,” he continues. “If you have a patient with keratoconus, that’s asymmetrical astigmatism, and an LRI may further destabilize the cornea.”
Thoroughly screening patients will provide further clues about their corneas because some findings may disqualify them as candidates.
“One of my screening questions for keratoconus is to ask the patient whether his eyes itch sometimes,” says Anita Nevyas-Wallace, MD, the medical director of Nevyas Eye Associates in the greater Philadelphia area. “If he says yes, I ask whether he sometimes rubs them. Patients who would never say yes if asked whether they rub their eyes, may admit to it, if the question is phrased as ‘Do you sometimes rub your eyes?’—that, they’ll admit to. And if a patient volunteers that when he rubs his eyes, it feels ‘really, really good,’ that person is probably well on his way to keratoconus, regardless of what other testing shows. Such patients should not have incisional keratotomy, in my view.”
In addition to screening questions, diagnostic exams will complete the picture. “Preoperative corneal tomography provides vital information,” says Dr. Nevyas-Wallace. “At the very least, you need corneal topography. Tomography (such as with the Galilei or Pentacam devices) gives you additional information that’s important, both in assessing whether there’s a tendency to ectasia and also in providing a corneal thickness map.”
Dr. Devgan agrees. “I like to do topography, as well as tomography,” he says. “That will not only tell me the corneal astigmatism pretty accurately, but the tomography will tell us anterior and posterior cornea and also give me thickness (pachymetry). If you have access to it, also measure the pachymetry, if possible.”
The pachymetry reading will help guide the subsequent relaxing incision. “If you’re going to do a 500-micron deep LRI and the patient’s corneas are 550 microns, well that will have more of an effect as opposed to a patient with a 650-micron cornea,” Dr. Devgan says. “Even corneal diameter is a factor. If you have a small eye that’s very hyperopic and the patient is getting a 28-D lens, that same size LRI may have a different effect than in a big myopic eye with a 6-D lens. There’s some experience that you have to take into account. However, the nice part is, even if you just attempt it and even if you undercorrect, patients are still improved.”
No two patients’ tissues will respond the same, he continues. “If you compare a 50-year-old cataract patient to a 90-year-old cataract patient, the same incision in those eyes is going to have a different effect,” he says. “That’s partly due to corneal elasticity. It changes as you get older and becomes less elastic. There’s an age component to how much you’re going to treat their astigmatism.”
LRIs can also be used as a touch-up technique. “One of the advantages of LRIs is that they leave the central cornea untouched, unlike LASIK and PRK,” Dr. Nevyas-Wallace says. “Another advantage is that the very patients who most commonly require LRIs—elderly patients having cataract surgery—are excellent candidates for LRIs and are often not such good candidates for LASIK or PRK. Because we get significantly greater astigmatic effect with an LRI as corneal rigidity increases—and it’s well demonstrated that it increases with age—they actually work better in older patients as well. LRIs of relatively short arc length, performed at the 9- or 10-mm optical zone will correct relatively modest amounts of astigmatism, and are also well-suited to touching up other procedures, such as toric lens implants.”
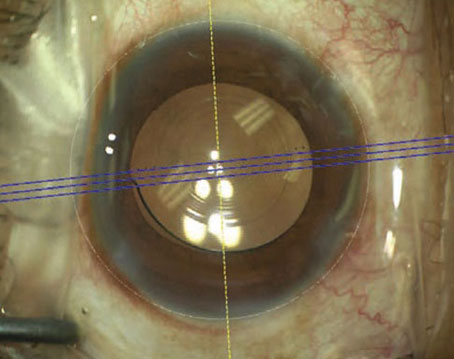
 |
| Uday Devgan, MD, performs LRIs manually with the help of a fixation ring marked off in clock hours to guide his incisions. (Courtesy Uday Devgan, MD) |
Considerations for the Procedure
Whether it’s determining when to perform the LRI or the number of incisions, surgeons must consider the risks and their own skill set.
“My preference is to do the LRI before the cataract procedure so as to avoid placing a side port right where an arcuate incision is planned,” says Dr. Nevyas-Wallace. “Placing an arc over a sideport risks perforation. The corneal marking and the incision are done at the beginning of the case.”
Dr. Devgan says perforation is the worst possible complication of LRIs. “If you need to do an LRI at 500 microns depth and the cornea has a thickness of 560 microns, that’s great; you’re not going to perforate,” he says. “But if you end up compressing the corneal tissue or pushing down too hard and the blade goes full thickness and aqueous leaks out, now you’ve got to put in at least one suture if not multiple sutures to close that to prevent leaking. That’s the challenge.” For this reason, Dr. Devgan says he prefers to perform LRIs at the end of a case.
The question of how many incisions are needed depends on the amount of astigmatism, as well as other factors of the surgery itself. “Symmetry is nice, but it can depend on the level of astigmatism. Sometimes a small amount can be taken care of by one incision,” says Lisa Arbisser, MD, an adjunct professor at the University of Utah, Moran Eye Center. “Something that helped me tremendously was the Mastel keratoscope, which is a simple little ring of lights that goes on to the bottom of the ocular of the microscope. It’s so helpful for any astigmatic work including toric because you get a reflex off of the cornea and you also get a reflex off of the lens, which you can then make sure it’s 90 degrees apart. And with some practice, you can even pick up 0.75 D or 1 D of astigmatism with that. And that was always reassuring for me, despite any markings or any other equipment, that I was on the correct axis and I could see it change with my LRI/PAK and confirm.”
Surgeons can also pair their phaco incision with an LRI. “If we happen to be operating on the steep meridian, then the surgical incision can be considered one of the astigmatic incisions,” says Dr. Nevyas-Wallace. “A single arcuate incision opposite that gives good effect. Or you can plan the surgery so that the surgical incision is on the steep meridian. That certainly simplifies the vector addition calculations which add the effect of the surgical incision and the astigmatic incisions in order to determine at what axis the astigmatic incision should be placed. Online calculators are helpful, but it’s simplest if the main incision is on the steep axis, which isn’t always possible. It’s hard to make the main incision at 6 o’clock, and if the superior cornea is truncated, it’s hard to make it at 12 o’clock. Location of the cataract incision is determined partly by the corneal anatomy.”
“In general, I tend to do two limbal relaxing incisions, unless I’m pairing it with the phaco incision,” says Dr. Devgan. “If I’m pairing it with a phaco incision, I’ll do one opposite the phaco incision. When you calculate how to do the LRI you have to take into account the effect of your phaco incision. When you’re doing your LRI and the patient’s steep axis is 30 degrees, you can make the phaco incision at 30 degrees and therefore opposite that on the other side I can do another limbal relaxing incision to pair it up with that so I don’t need to have two. As long as I’m placing my phaco incision on the steep axis then I can just make the LRI opposite. If I’m making my phaco incision somewhere else, then I probably want to do paired LRIs, but I also take into account mathematically what is the effect of my phaco incision on changing the astigmatism.”
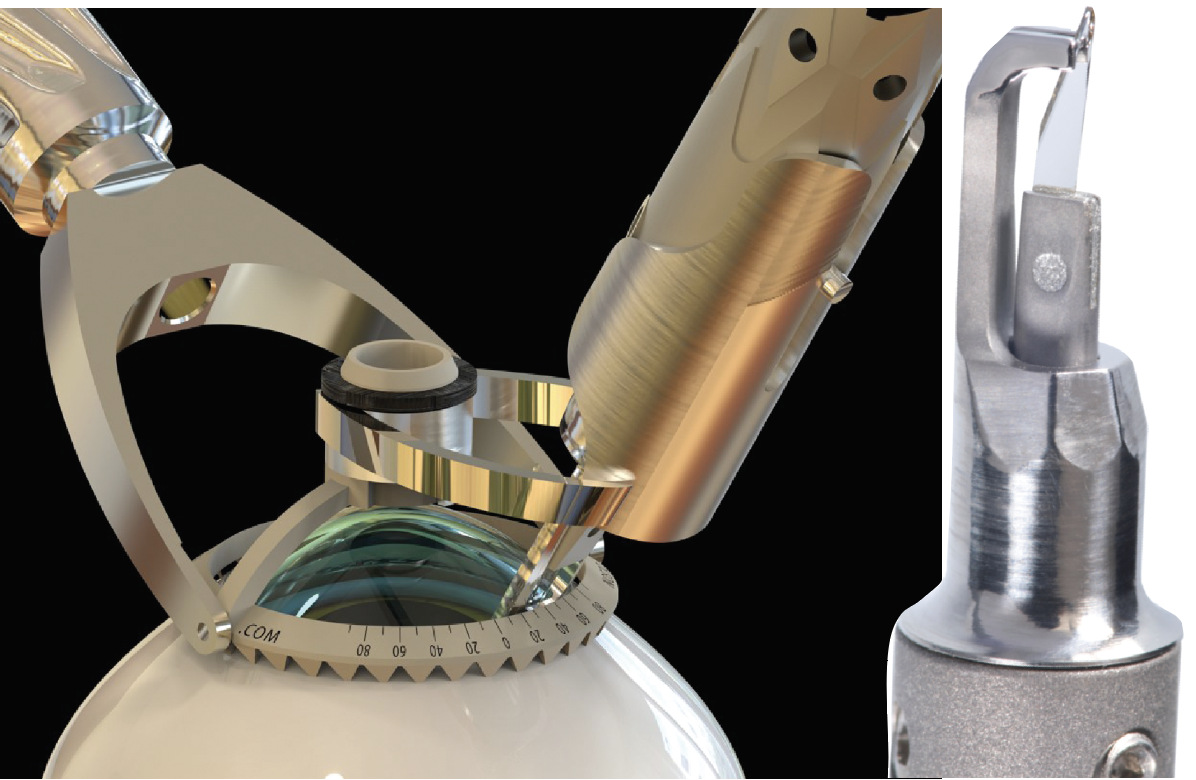 |
| Tools such as the Bridge AK knife (right) and the arcuate compass (left), both from Mastel, can improve accuracy of manual LRIs. The compass is used to make an arcuate incision at a lesser depth, then the Bridge AK knife deepens the two ends. |
Techniques and Tools For Success
The right technique and the right tools will go a long way for LRIs. One of the first pieces of advice Dr. Nevyas-Wallace offers is regarding fixation of the globe.
“Performing an LRI or AK is significantly safer when the globe is fixated with a surgical instrument. One thing that’s become popular is doing LRIs at the slit lamp,” she says. “In an LRI course I teach, I point out that if you have one hand on the joystick and one hand on the knife, that doesn’t leave you any way to fixate the globe. When performing LRIs at the time of cataract surgery, the surgeon shouldn’t have two hands on the knife, but rather one hand should be fixating the globe. The best way to fixate it is with forceps that grasp limbus-to-limbus, meaning two points 180 degrees apart. But even grasping one point is a lot better than no fixation at all, because without fixation, there’s a risk that the patient suddenly glancing away could result in disaster.
“That doesn’t mean that you can’t do LRIs in the office,” she continues. “When we do LRIs in the office, we lay the patient down under a surgical microscope so that the surgeon can use one hand to fixate as the other creates the incision.”
Dr. Devgan uses a specially designed fixation ring to hold the eye. “This fixation ring is marked off in clock hours,” he says. “Each clock hour is 30 degrees. If I want to do a 30-degree arc, that’s just one clock hour. I usually put my fixation ring down and you can just trace the blade against that so your arc will be perfect.”
It’s important to accurately mark your steep axis and take cyclorotation into account when the patient is lying down, continues Dr. Devgan. “Surgeons need to have a guarded diamond blade, or at least a guarded blade of some sort—it doesn’t necessarily have to be diamond, but that’s our sharpest option if we can keep it safe and in good condition,” he says. “We need to know what depth to place it, although in general, people will often use 600 microns, which works for just about everyone, however it’s nice to have topography ahead of time to be sure we have regular astigmatism to help us choose our steep axis and to be able to follow that patient afterwards as well.”
LRIs can be made much more predictable by using instrumentation that allows the surgeon to control the incision architecture, says Dr. Nevyas-Wallace. “We used to think that creating uniform depth incisions would solve those problems and give a more regular and predictable effect,” she says. “To some extent, uniform depth incisions are more predictable in that at least the effective axis is what it’s intended to be, but the depth is still an issue. With femtosecond laser corneal relaxing incisions, most nomograms call for an incision depth that’s not really deep enough to get the desired effect. Consequently, the arcs are longer and/or the optical zones smaller than they might ideally be. We know that the longer the arc, especially beyond a certain point, the greater the induced aberration.”
One of the most significant sources of inaccuracy is that the effective portion of a limbal relaxing incision is usually far shorter than the incision length on the surface, explains Dr. Nevyas-Wallace. “Most manual corneal incisions are shallower at each end than they are at the center of the arc. At the slit lamp, blade incisions are shallow at both ends. Only the deep portion has useful astigmatic effect,” she says. “So a 45-degree arc may actually be at the intended depth for only 30 degrees. But here’s the problem: a diamond blade doesn’t reach the micrometer-set depth until it’s been cutting through tissue. Consequently, the portion at the intended depth is not the central 30 degrees of that arc. The effective portion is nearly the terminal 30 degrees, so the effective axis is likely to be way off.”
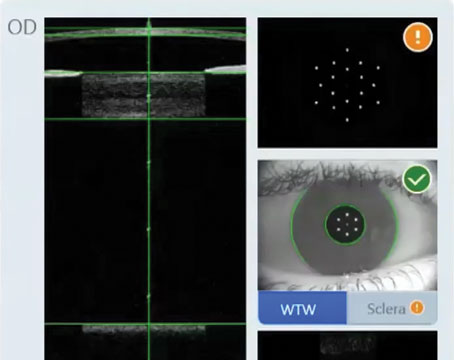
Dr. Nevyas-Wallace says it’s important to consider the early days of elevation corneal topography to understand how tools have been developed. “In the early days of elevation corneal topography, I noticed that the arcuate incisions were having more effect at the center of the incision than at the two ends,” she says. “This was leading to induced astigmatism at oblique axes. I’m not the first person to notice that; it’s called keratopyramis because it does look sort of like a pyramid. There was a procedure designed to correct this (described by Canrobert Oliveira, MD, from Brazil), in which a smaller incision was made just peripheral to each end of the AK in order to augment the effect at the ends. And someone else, also from Brazil, suggested placing the smaller incisions just central to LRIs. At least until recently, you could buy markers from Mastel for the ‘Canrobert C Procedure.’ But the problem is that additional incisions can have unexpected effects as well and it seemed to me that if we could only make our incisions uniform depth, that would solve the problem.”
Dr. Nevyas-Wallace says a modification to knives used for radial keratotomy helped improve LRI outcomes. “First, the DuoTrak/Genesis knife didn’t allow the surgeon to visualize the blade cutting an arcuate incision, as it was designed for radial incisions, not arcuate incisions,” she says. “The solution was a diamond knife whose blade was mounted just a little bit in front of the footplates, which Mastel made for me. But the other issue was that, to my surprise, I found that for a uniform depth incision, the uneven effect of the incision was less pronounced, but it still existed. There continued to be greater effect at the center of the incision. That was when I realized that indeed the center has to be the area of greatest relaxation because each end is stabilized by an intact cornea. Any incision is apt to gape the most at its center. In order to reduce the effect of the arc’s center, I started making the arcuate incisions shallower in the center. That helped, but didn’t solve it completely. I made the arcs more and more shallow at the center until there was no longer an uneven effect. Surprisingly, I was also getting the desired astigmatic effect with shorter incisions.”
While Dr. Nevyas-Wallace continued doing LRIs that way, it occurred to her that a femtosecond laser might be able to control the incision architecture. She says that after working with a team of researchers in Switzerland, they found that her “ ‘shallower in the center incisions’—which she calls ‘Bridge AK’ (because the shape reminded her of a bridge)—induced a lot less aberration. The modeling also showed that a Bridge AK incision actually gets greater astigmatic effect—15 percent more in that [Swiss] study.
“The next question was how would you know just what that Bridge AK contour should be?” continues Dr. Nevyas-Wallace. “We’re developing a way to make this capability available to surgeons. This will tell the femtosecond laser just what the arc’s shape should be. Creating manual LRIs that use this principle is an improvement over uniform depth incisions and certainly over traditional shallow-ended manual LRIs.”
However, Dr. Nevyas-Wallace says manual LRIs don’t need to be done freehand. A helpful tool to consider is an arcuate compass (Mastel), that allows guidance of the manual incision, she says. “Now, that alone doesn’t give you a bridge incision or even uniform depth because the diamond, as I mentioned, doesn’t achieve the desired depth until it’s been moving through tissue. Even then, it achieves full depth only if it’s applanating the cornea. Applanating the cornea is counterintuitive. I can’t think of anything else we do in cataract surgery or corneal surgery in which you press hard enough to dent anything in. Normally, we pride ourselves on not doing that. And yet in this particular situation, the desired depth is not achieved unless the footplates applanate the cornea,” says Dr. Nevyas-Wallace.
The Bridge AK knife has a vertical “enhancement” edge sharp only for the distal 300 microns, she continues. “We use the compass to make an arcuate incision at lesser depth and then use the Bridge AK knife to deepen the two ends. This incision architecture is often detectable at the slit lamp and the results are more predictable,” Dr. Nevyas-Wallace says.
Predictability may be improved with the use of nomograms and femtosecond lasers. Dr. Devgan recommends starting with a simple nomogram proposed by Kevin Miller, MD, of UCLA Health. He explains:
- use 1 clock hour of paired incisions for 1 D of corneal astigmatism;
- note that 1 clock hour is 30 degrees;
- vary this with the patient age;
- do a little more in younger patients (<60);
- do a little less in older patients (>80);
- take into account the effect of your phaco incisions;
- if operating temporally, more LRI arc length for WTR, less for ATR.
The Nichamin nomogram (Figure 1) is another vetted nomogram, Dr. Devgan adds.
Dr. Whitman recommends speaking with colleagues about their nomogram preference if you’re just starting out with LRIs. Using a femtosecond laser has helped him as well.
“I have my own self-generated nomogram developed over the years, but there are a lot of published nomograms that you can use for accurate, long-lasting astigmatism correction,” Dr. Whitman says. “A lot of that has to do with doing adequate depth, which has to be at least 80 percent or more depth because you don’t want the effect to go away. In the past people may have avoided doing LRIs thinking the effect goes away too soon. But a lot of people were afraid to go deep, only doing 50 to 60 percent depth. Incisions like that will close up. We always went for 80 to 90 percent depth when we used a diamond blade for manual LRIs, and we would do ultrasound measurements over the area so we could be more accurate.
“We now routinely use the laser for LRIs. It’s much easier using modern lasers because they’ll take a measurement, and if you tell it to do 80 percent, it’s going to do 80 percent,” he continues. “It takes all of the guesswork out of it. It can make sure you’re doing a consistently deep incision, at a consistent length, in a consistent optical zone because the smaller the optical zone and the longer the incision, the more effect you’re going to get.”
Dr. Whitman advises that every femtosecond laser is somewhat different. “They don’t all measure the depth in the same manner, so my advice would be to know your laser well so you can get the best performance from your LRIs,” he says. “If you don’t get enough correction or you overcorrect, it’s not the laser’s fault. You have to figure out what to do differently.”
Complications
Aside from the aforementioned perforations, surgeons should be aware of other complications involving LRIs.
“People do get concerned with flipping the axis, and we can overcorrect,” says Dr. Arbisser. “There are some people who will make it a full thickness, nasal clear corneal incision that they never open as another option for treating against-the-rule-astigmatism along with their temporal clear corneal incision that they use for the surgery. That’s another route I never chose as that’s now through-and-through the incision with a very rare—but potential—risk for endophthalmitis.”
Along with overcorrection, Dr. Nevyas-Wallace mentions ectasia. “This can occur either because the incision is longer than that cornea can tolerate or because the patient had undetected subclinical keratoconus,” she says.
Dr. Whitman says postop topical antibiotics are important to prescribe. “There are a lot of surgeons who put antibiotics inside the eye at the end of surgery, but don’t place the patient on topical antibiotics afterwards,” he says. “I think you need them. We learned that the hard way when we were doing dropless surgery for a while and LRIs would sometimes get inflamed. There’s always the possibility of bacteria from the eyelid and eyelash junction rubbing over the LRI area, causing an infection or ulcer.”
Dr. Nevyas-Wallace expects LRIs will remain an important technique for refractive cataract surgeons. “I think it’s very important to be able to do LRIs and to be able to do them safely and precisely,” she says. “As our diagnostic equipment and technology improve, we’ll be able to be even more precise and get even better results.”
Drs. Arbisser, Devgan and Nevyas-Wallace have no relevant disclosures. Dr. Whitman discloses consulting relationships with Alcon, Johnson & Johnson Vision and Bausch + Lomb.