We asked several ophthalmologists who have experience with this problem to share what they've learned about it, the latest thinking about causes and possible treatments, and what the future may hold.
The Nature of NAAION
Jacqueline M. S. Winterkorn, MD, PhD, clinical professor of ophthalmology and neurology and neuroscience at Weill-Cornell Medical College and attending ophthalmologist at New York Presbyterian Hospital, notes that a patient with NAAION may have no known medical problems. "He doesn't go to a doctor," she says. "He bought +2 D reading glasses when he was 43 that he's been wearing for the past 10 years. He wakes up one morning and shaves. Then he sits down for breakfast and finds he can't read the paper.
"There may be nothing in his medical history that would predict this," she adds, "except that about a month ago an internist started him on a beta blocker because his blood pressure was edging up. It's typical to find no history of blood pressure problems, or only a recent diagnosis."
Sohan Singh Hayreh, MD, MS, PhD, professor emeritus of ophthalmology and director of the Ocular Vascular Clinic at the College of Medicine at the University of Iowa, notes that multiple risk factors play a role in the development of NAAION. "I divide all risk factors into two categories: predisposing and precipitating," he says. "Predisposing risk factors make a person susceptible to the disease but do not necessarily produce it. Precipitating risk factors act as the 'last straw' leading to NAAION."
Dr. Winterkorn notes that a key contributing factor appears to be a small disc with a very small cup—the so-called "disc at risk." (See picture, below.) "This is a typical hyperopic-looking disc," she says. "If axons begin to swell, they have no place to go, so they compress neighboring axons, causing further swelling. You have a cascade of infarction, killing off axons. That appears to be the pathophysiology of AION."
A "disc at risk." A small, crowded optic nerve head is a risk factor for AION; if axons swell, they may compress neighboring axons, triggering a cascade.
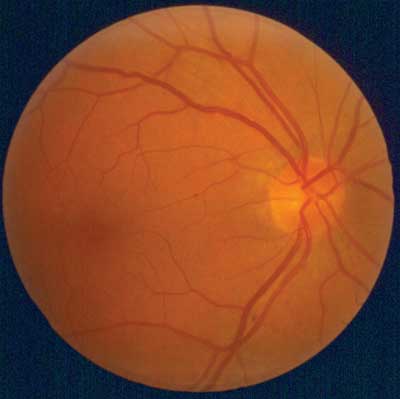
All images courtesy of Jacqueline M.S. Winkerton, MD, PhD
As to what triggers the lack of perfusion that sets this chain of events into motion, a number of possibilities are currently under scrutiny. These include hypotension at night and upon awakening (likely compounded by treatment for hypertension); sleep apnea; drugs being taken for erectile dysfunction; and a likely connection to elevated cholesterol.
Nighttime Hypotension
NAAION most often occurs upon awakening in the morning or shortly thereafter. This fact has led to numerous studies relating NAAION to the well-established pattern of blood pressure dropping during overnight sleep—and concern about the potential contributing effect of medications intended to lower high blood pressure, often taken by older patients.
Dr. Hayreh, who first described AION in a 1974 study1 believes that nocturnal arterial hypotension is the most important causal factor. "My studies have shown that in more than 75 percent of cases the precipitating risk factor is nocturnal arterial hypotension," he says. "The main source of that is overmedication with blood pressure lowering medications, or having patients take them at bedtime or in the evening."
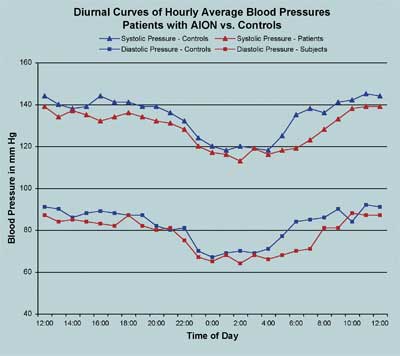
One study2 found that diurnal curves of blood pressures of patients with AION were close to controls during the day and through the nighttime nadir, but diverged in the early morning hours. This suggests that a failure of autoregulation upon awakening could be a key factor in NAAION, which frequently occurs at this time of day.
One suggestive piece of evidence for the medication connection, cited by Dr. Hayreh, is that NAAION was much rarer before the advent of today's blood pressure lowering medications. "NAAION was an extremely rare disease before the late 1960s, with only a handful of cases reported in the literature under different eponyms when I first described it," he says. "Now NAAION has become far more common. One reason is pretty obvious: Before the mid-1960s, the only available treatment for arterial hypertension was diuretics. But then came the beta-blockers; then calcium channel blockers; then ACE [angiotensin-converting enzyme] inhibitors. Now we have many highly potent blood pressure lowering drugs."
Given the possibility that taking the medication at bedtime could be part of the problem, Dr. Hayreh urges caution. "Many NAAION patients are taking these drugs for heart problems, and they may be essential," he notes. "Simply to advise these patients not to take their medicine at bedtime could cause serious problems, even death. I strongly advise all my patients not to change their medication unless and until they have the agreement of the internist who prescribed it. I tell them that if their heart stops working, they won't need their eyes anyway!"
A Failure of Autoregulation?
Dr. Winterkorn's work has convinced her that the connection between NAAION and nighttime hypotension has more to do with autoregulation of pressure after awakening than with the absolute drop in blood pressure during nocturnal sleep. "Dr. Klara Landau and I collaborated on a study of blood pressure in NAAION patients and controls matched for medical conditions and medications," she says.2 "We found that the AION patients' and controls' blood pressure curves were very close during most of the day and night. [See chart.] Everybody had lower pressure at night, and everybody had a nadir. But the nadir of the AION patients was at no time lower than the controls.
"Instead, the major difference between the two groups was upon awakening in the morning," she continues. "The control group without AION had a rapid and precipitous rise in blood pressure to meet the demands of the day. In contrast, the AION patients' pressures went up more slowly, and irregularly—not as responsive to the demands of morning activity. So we believe the AION occurs because the person is unable to mount a response to the day's demands for higher blood pressure. In other words, they experience relative hypotension."
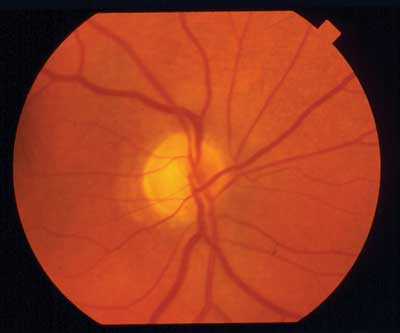
Pseudo Foster Kennedy Syndrome: Pallor from AION suffered 10 years ago, OD. (Also, see picture below.)
Dr. Winterkorn notes that a similar observation has been made in connection with the timing of heart attacks. "Most people don't have a heart attack while they're sleeping—they wake up and have it," she says. "We believe you don't have your AION while you're sleeping—you wake up and then have your AION. And that seems to fit with the data collected during the ION trial, which is that these people didn't complain of waking up with their vision not working. Instead, an hour or so later they went to read the paper and found that they couldn't see."
Part of the problem, according to Dr. Winterkorn, could be the idea that when it comes to blood pressure, a little bit lower is always better. "We have to remember that our aim is not to hit a certain pressure, but to perfuse the brain and eyes. Some elderly people have been hypertensive for so long that their blood vessels need a certain level of pressure to perfuse the tissues. If you decrease the pressure below that level, you put them at risk of ischemia."
Dr. Winterkorn notes that a "disc-at-risk" may still be a necessary predisposing factor. "People without this type of disc, such as myopes and glaucoma patients, rarely have this problem," she says.
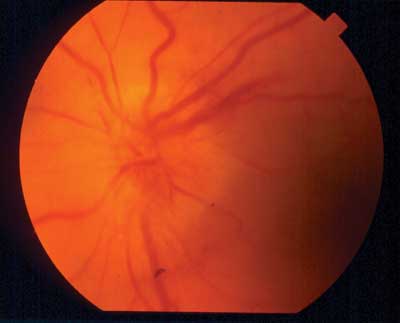
Pseudo Foster Kennedy Syndrome: Acute AION with disc edema, hemorrhage and hyperemia, OS.
Sleep Apnea: Cause for Concern?
Several studies have found a high correlation between sleep apnea and NAAION.3,4 Notably, a recent study conducted in Grenoble, France,5 suggests a highly significant connection. In the latter study, 27 newly diagnosed NAAION patients were tested for sleep apnea syndrome (as opposed to simply being asked whether they experienced the symptoms). Eighty-nine percent of the patients exhibited the syndrome; in fact, the risk ratio for a NAAION patient to have sleep apnea was 4.9 compared to the general population (p=0.001). Furthermore, compared to other risk factors typically associated with NAAION, such as hypertension and diabetes, sleep apnea was found to be present 1.5 to 2 times as often in these patients. If these data are duplicated in other studies, breathing irregularities at night could turn out to be a key factor in NAAION.
Michaela K. Mathews, MD, clinical assistant professor of ophthalmology at the University of Maryland in Baltimore, has been aware of the potential connection. "In my practice," she says, "I try to elicit a history of symptoms that are suspicious or suggestive of sleep apnea. Snoring, of course, can be a symptom of sleep apnea, but many time male patients who have NAAION deny that they snore. Then the wife says, 'Are you kidding? You snore like crazy!' It's a piece of the history that may be better gathered from the significant other than from the patient.
"Some have recently questioned the connection between sleep apnea and NAAION," she continues, "but research supports it. Sleep apnea has also been connected with hypertension, cardiovascular disease and increased risk of stroke; it all goes down the same aisle. If a patient appears slightly overweight and complains of snoring and daytime drowsiness, I'd refer him for a sleep study."
Dr. Mathews notes that one treatment for sleep apnea that has been tried in this context is CPAP (continuous positive airway pressure). "In some instances these patients still developed AION," she notes, "so this treatment may not be enough to prevent damage to the other eye or further complications."6 She adds, however, that compliance to the treatment protocol is difficult to ensure.
NAAION and Erectile Dysfunction
In 2005, Howard D. Pomeranz, MD, clinical associate professor of ophthalmology at New York University, published a report describing seven cases in which men between 50 and 69 years showed symptoms of NAAION within 36 hours of taking sildenafil citrate (Viagra); all subjects had pre-existing hypertension, diabetes, elevated cholesterol or hyperlipidemia.7 Similar associations have been found in other studies.8
"There are many problems with drawing conclusions based on these reports," admits Dr. Pomeranz. "A lot of the patients have other vascular risk factors like high blood pressure, diabetes or high cholesterol. It can be very difficult to tell whether the ION occurred as a direct result of using the drug or as a result of the risk factors which may have led to the erectile dysfunction in the first place."
Nevertheless, he says the evidence suggesting a connection is hard to ignore. "Most of the patients in the 2005 study had the attack within 24 hours of taking the ED drug," he notes. "That's what convinced me of the connection. In one case, the onset of visual symptoms occurred less than an hour after taking the drug." Dr. Pomeranz adds that many other cases suggesting a connection have been reported. "At the time of publication of that paper, the Food and Drug Administration was aware of 40 or 50 cases," he says. "I've had another 10 or 12 reported to me by patients and other ophthalmologists. However, no one has yet proven the connection."
Asked about a possible mechanism to explain the connection—if it is real—Dr. Pomeranz says there are several theories. "One is that since the drug is involved in modulating blood vessel diameter, it may alter arterial blood perfusion to the optic nerve, causing it to drop below a threshold point, producing ischemia," he says. "The other possibility is that the blood pressure around the optic nerve is autoregulated, meaning that it automatically shifts in response to changes in the body. It could be that something is wrong with the autoregulatory capacity in individuals who are susceptible to ION, and when this drug is given it enhances the problem."
Dr. Pomeranz admits that the number of reported cases seems small given the large number of individuals taking ED drugs. However, he notes that NAAION is rare to begin with. "In general," he says, "the incidence of NAAION is about one in 50,000 people 50 years or older. You have to use that as your baseline for the number of cases there are, and then ask whether taking Viagra increases that frequency ratio. The problem is, we know the numerator is 50 or 60 cases, but we don't know what the denominator is, in terms of how many total potential cases there are out there."
Dr. Pomeranz adds that many patients and doctors may not make the connection, or report it even if they do. "If men lose vision in their eyes while taking one of these drugs and go to the eye doctor, how many will make the connection and point out that they're taking a drug for ED?" he asks. "Actually, in some of the early cases that were brought to my attention, patients raised this possibility with their primary-care doctors; the doctors told them there was no way they could be connected."
Dr. Pomeranz says that, given the possible connection, there are a few things the average clinician and patient can do to try to minimize the risk of NAAION. "Clinicians should ask patients about the use of ED drugs when they diagnose NAAION," he says. "Patients who take these drugs might want to be examined to find out if they have the small optic disk and small cup-to-disk ratio that's highly associated with NAAION. Any patient who has lost vision in one eye due to NAAION definitely should not use this class of drug, as it may increase the risk of occurrence in the fellow eye. And a patient who takes these drugs should be told to see his ophthalmologist right away if he experiences any visual disturbance other than transient color changes."
Dr. Winterkorn notes that pre-existing cardiac or vascular problems could be a predisposing factor when ED drugs are taken. "Many men who take Viagra have erectile dysfunction because they have vascular disease, so they're at risk for AION even if they don't take Viagra," she says.
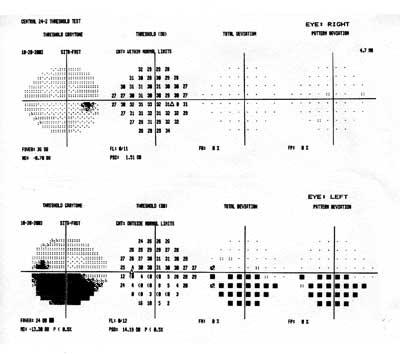
A 55-year-old man with sudden, painless visual loss OS shows a typical AION visual field loss. Humphrey 24-2 threshhold test is normal OD, with inferior altitudinal loss OS.
In any case, Dr. Winterkorn agrees that patients who have predisposing factors should be warned about the risk. "I'm now telling vasculopathic patients who have the typical looking hyperopic small disc and small cup that they may be at risk for AION if they take medications like Viagra," she says. "Certainly if they've already had transient visual loss or an AION in one eye, they should be very careful."
The Cholesterol Connection
Clinical evidence has demonstrated a likely connection between NAAION and atherosclerosis. Dr. Mathews is interested in that possibility, particularly in younger people who are usually thought to not be vasculopathic.
"Vincent Deramo, Robert Sergott and fellow researchers published a study in 2003 regarding NAAION as a first manifestation of elevated cholesterol level in patients who were 50 years old or younger," she points out.9 "There was a statistically significant difference in cholesterol between normal controls and people who had NAAION within the same age group. Those with NAAION averaged 235 mg/dl; controls averaged 204 mg/dl. The odds ratio of having high blood cholesterol—over 240 mg/dl—was 3.3 with NAAION compared to controls, and the likelihood increased when the comparison was restricted to nondiabetic patients."
While it might be difficult to know which younger, otherwise healthy, patients have the elevated levels noted in this study, Dr. Mathews points out that NAAION in a younger individual could be seen as a warning of possible cardiovascular trouble. "If we have a patient with ION, the least we can do is direct him to a good internist and have him worked up for cardiovascular risk factors," she says. "Treatment might prevent ION in the second eye; it also might prevent a heart attack or stroke five or 10 years down the road."
Treating NAAION
Unfortunately, no one has any easy answers when it comes to prevention or treatment of NAAION, even when someone has already had an attack. "The problem is that even though we know some of the risk factors for AION, we have no cure," observes Dr. Winterkorn. "We're only grasping at theories of how to prevent it.
"For example," she says, "a paper by Mark Kupersmith, MD, reports that giving an AION patient aspirin prevents or protects the second eye from developing AION.10 People are trying brimonidine, on the premise that it's neuroprotective, but without good evidence to support its effectiveness in this situation. Some people give pentoxifylline (Trental)—a drug that changes the shape of red blood cells so they can get into places they would not ordinarily go, but there haven't been controlled trials of its effectiveness in AION. Ginkgo biloba and other medicines have also been tried."
Dr. Hayreh believes that aspirin is unlikely to help. "In our study11 we showed that aspirin does not make any difference to development of NAAION, he says. "That was also shown by the multicenter optic nerve sheath decompression study.12 Stroke is a thromboembolic disorder, while NAAION is a hypotensive disorder. Atherosclerotic changes in the arteries can make the optic nerve head and other structures more susceptible to ischemic disorders, and thus may act as a predisposing factor. But embolism is only occasionally the cause of NAAION."
At the moment, the only course of action that everyone agrees upon is reducing risk. "NAAION happens in persons who have predisposing risk factors," notes Dr. Hayreh. "Thus, to reduce risk you must try to reduce as many risk factors as possible. A thorough medical evaluation is essential."
Dr. Winterkorn agrees. "Although 50 percent of these patients have no prior medical diagnosis, 30 to 50 percent have hypertension—including overtreated hypertension," she says. "Twenty-five percent have diabetes, and 20 percent are smokers. So we can advise the patient to minimize these risks. And we can learn more about the autoregulation of blood pressure by studying AION patients—especially their 24-hour blood pressure curve."
1. Hayreh SS. Anterior ischaemic optic neuropathy. Br J Ophthalmol 1974;58:955-989.
2. Landau K, Winterkorn JMS et al. 24-hour blood pressure monitoring in patients with AION. Arch Ophthalmol 1996;114:570-575.
3. Mojon DS, Hedges TR 3rd, et al. Association between sleep apnea syndrome and nonarteritic anterior ischemic optic neuropathy. Arch Ophthalmol 2002;120:5:601-5.
4. Palombi K, Renard E, et al. Non-arteritic anterior ischaemic optic neuropathy is nearly systematically associated with obstructive sleep apnoea. Br J Ophthalmol 2006;90:7:879-82. Epub 2006 Mar 23.
5. Palombi K, Renard E, Levy P, et al. Non-arteritic anterior ischaemic optic neuropathy is nearly systematically associated with obstructive sleep apnoea. Br J Ophthalmol 2006;90:7:879-82. Epub 2006 Mar 23.
6. Behbehani R, Mathews MK, Sergott RC, Savino PJ. Nonarteritic anterior ischemic optic neuropathy in patients with sleep apnea while being treated with continuous positive airway pressure. Am J Ophthalmol 2005;139:3:518-21.
7. Pomeranz HD, Bhavsar AR. Nonarteritic ischemic optic neuropathy developing soon after use of sildenafil (Viagra): A report of seven new cases. J Neuroophthalmol 2005;25:1:9-13.
8. McGwin G Jr, Vaphiades MS, Hall TA, Owsley C. Non-arteritic anterior ischaemic optic neuropathy and the treatment of erectile dysfunction. Br J Ophthalmol 2006;90:2:154-7.
9. Deramo VA, Sergott RC, Augsburger JJ, Foroozan R, Savino PJ, Leone A. Ischemic optic neuropathy as the first manifestation of elevated cholesterol levels in young patients. Ophthalmology 2003;110:5:1041-6.
10. Kupersmith MJ, Frohman L, et al. Aspirin reduces the incidence of second eye NAION: a retrospective study. J Neuroophthalmol 1997;17:250-3.
11. Beck RW, Hayreh SS, Podhajsky PA, Tan ES, Moke PS. Aspirin therapy in nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 1997;123:212-7.
12. Optic nerve decompression surgery for nonarteritic anterior ischemic optic neuropathy (NAION) is not effective and may be harmful. The Ischemic Optic Neuropathy Decompression Trial Research Group. JAMA. 1995 Feb 22;273:8:625-32.
13. Bernstein SL, Guo Y, Kelman SE, Flower RW, Johnson MA. Functional and cellular responses in a novel rodent model of anterior ischemic optic neuropathy. Invest Ophthalmol Vis Sci 2003;44:10:4153-62.
14. Goldenberg-Cohen N, Guo Y, Margolis F, Cohen Y, Miller NR, Bernstein SL. Oligodendrocyte dysfunction after induction of experimental anterior optic nerve ischemia. Invest Ophthalmol Vis Sci 2005;46:8:2716-25.
15. Bernstein SL, Koo JH, Slater BJ, Guo Y, Margolis FL. Analysis of optic nerve stroke by retinal Bex expression. Mol Vis 2006;1;12:147-55.
16. The BRAION study group; Wilhelm B, Ludtke H, Wilhelm H. Efficacy and tolerability of 0.2% brimonidine tartrate for the treatment of acute non-arteritic anterior ischemic optic neuropathy (NAION): a 3-month, double-masked, randomised, placebo-controlled trial. Graefes Arch Clin Exp Ophthalmol 2006;244:5:551-8. Epub 2005 Sep 8.




