Chemical injuries to the eye can have serious consequences and require prompt and appropriate management. Individuals who work around chemicals are most at risk for this type of injury, and we encourage this population to wear eye protection every time they’re handling chemicals. That said, many of the chemical injuries we see occur in individuals doing cleaning or house projects who aren’t well-versed in eye safety and protection. As we move towards “spring cleaning” these injuries become even more common. I had a patient who was opening his pool without eye protection and chlorine splashed back into his eyes, causing very severe injury.
Here, I’ll discuss the steps necessary when dealing with ocular chemical injury, from substance identification and classification to medical and surgical management.
Initial Steps
Limiting the amount of contact the chemical substance has with the eye is crucial. Most ocular chemical injury patients come through the emergency department, which is where we’re best able to irrigate the eye with something like a Morgan lens. However, because time to irrigation greatly influences visual prognosis, it’s recommended that patients who can’t get to the emergency department right away irrigate with whatever they have on hand, even if it’s not sterile, such as tap water.
 |
|
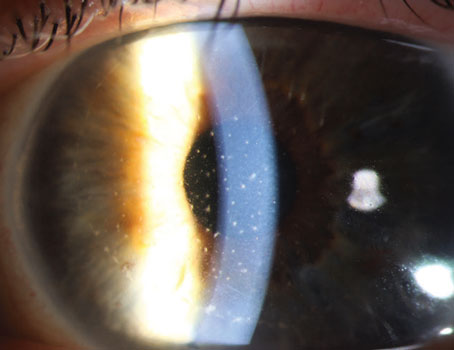
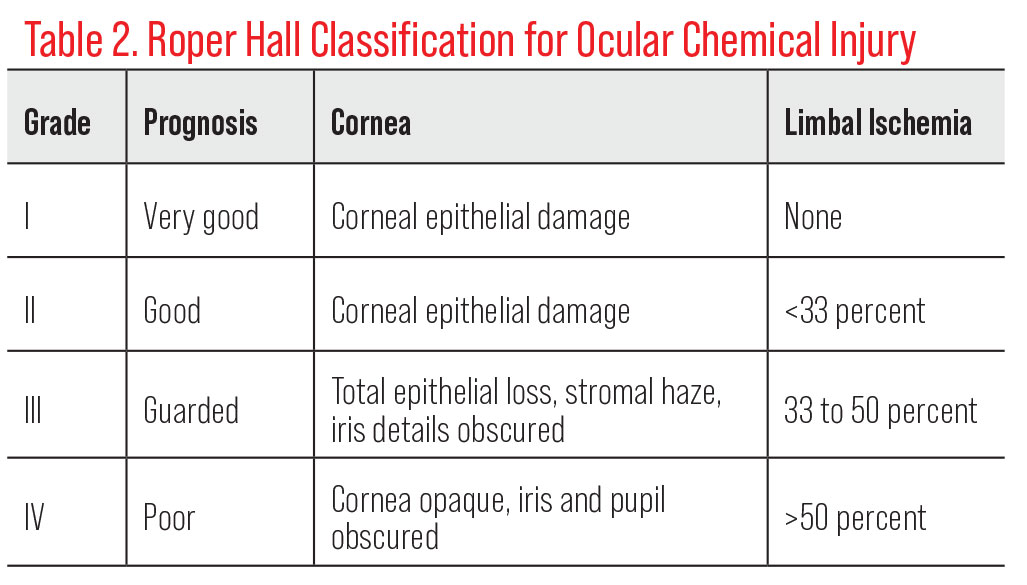
Figure 1. An alkali burn (sodium hydroxide degreasing solution: pH 13-14) 10 days after accident with complete stromal opacification of the cornea, 100-percent corneal epithelial defect and 360-degree-conjunctival epithelial defect. (All images: Laura Palazzolo, MD, and Alex Mammen, MD) |
When performing the initial exam, ensure that all of the toxic substance is fully out of the eye. Carefully flip the eyelids and evaluate underneath with a cotton tip, checking for any remaining fragments or debris that could cause persistent damage. I’ve had one case of wet concrete exposure where concrete bits stuck deep in the fornix and continued to leak chemicals and cause injury. This wasn’t initially identified in the emergency department, and pH remained high despite continuous irrigation.
Acidic vs. Alkali Burns
Understanding the nature of the chemical substance and its mechanism of injury at each phase is important for management. Acidic and alkali damage have several important differences:
• Acidic substances create a fair level of damage, but this damage is usually limited to the surface, to the epithelium and the skin. With the exception of hydrofluoric acid, acids denature and precipitate the tissue proteins they come into contact with, so they create their own coagulated protein barrier that blocks further penetration into the eye.
• Alkali substances are lipophilic and saponify fatty acids of cell membranes, allowing them to rapidly penetrate the corneal stroma and enter into the anterior chamber, causing many levels of damage (Figure 1). Mucous membrane loss, meibomian gland dysfunction with long-term dry-eye complications, limbal stem cell deficiency and even glaucoma are all possible consequences of intraocular penetration.
Be sure to confirm the pH level of the substance and check the eye’s pH level until it neutralizes to 7.
Classification
There are two main classification systems for the prognosis of ocular chemical injury. The Dua classification system considers the estimated degree of limbal and bulbar conjunctival involvement, with an analogue scale representing the amount of limbal involvement in clock hours divided by the percentage of conjunctival involvement (Table 1).
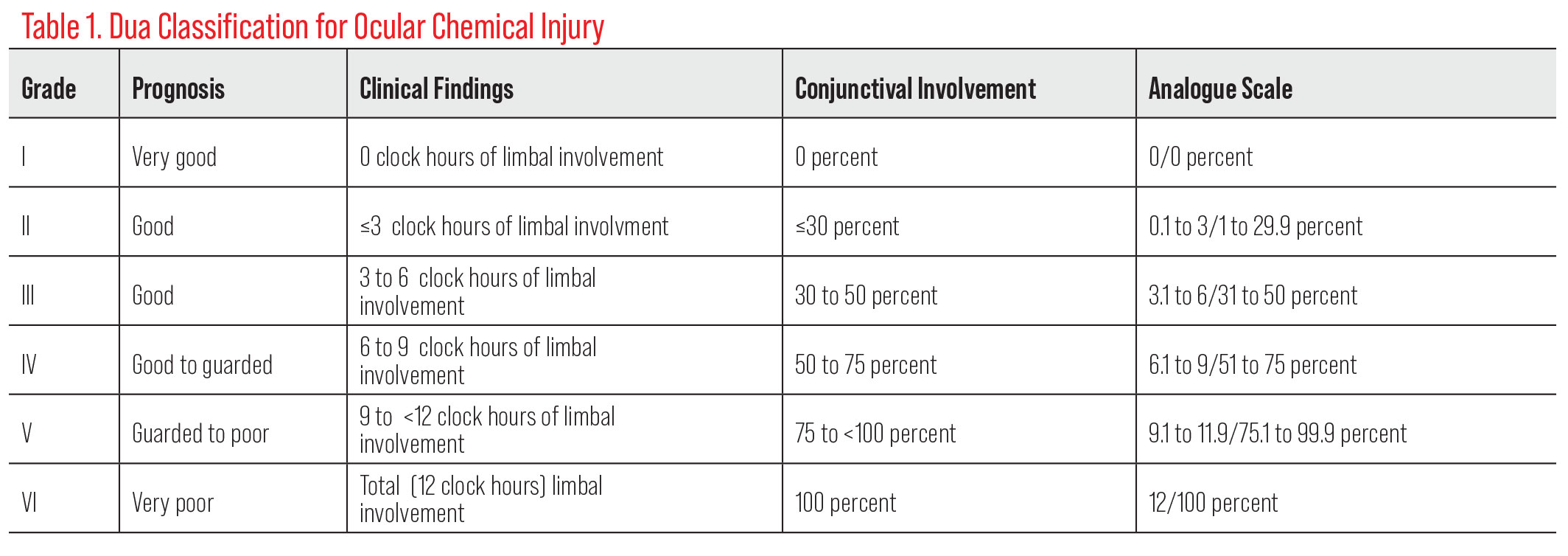 |
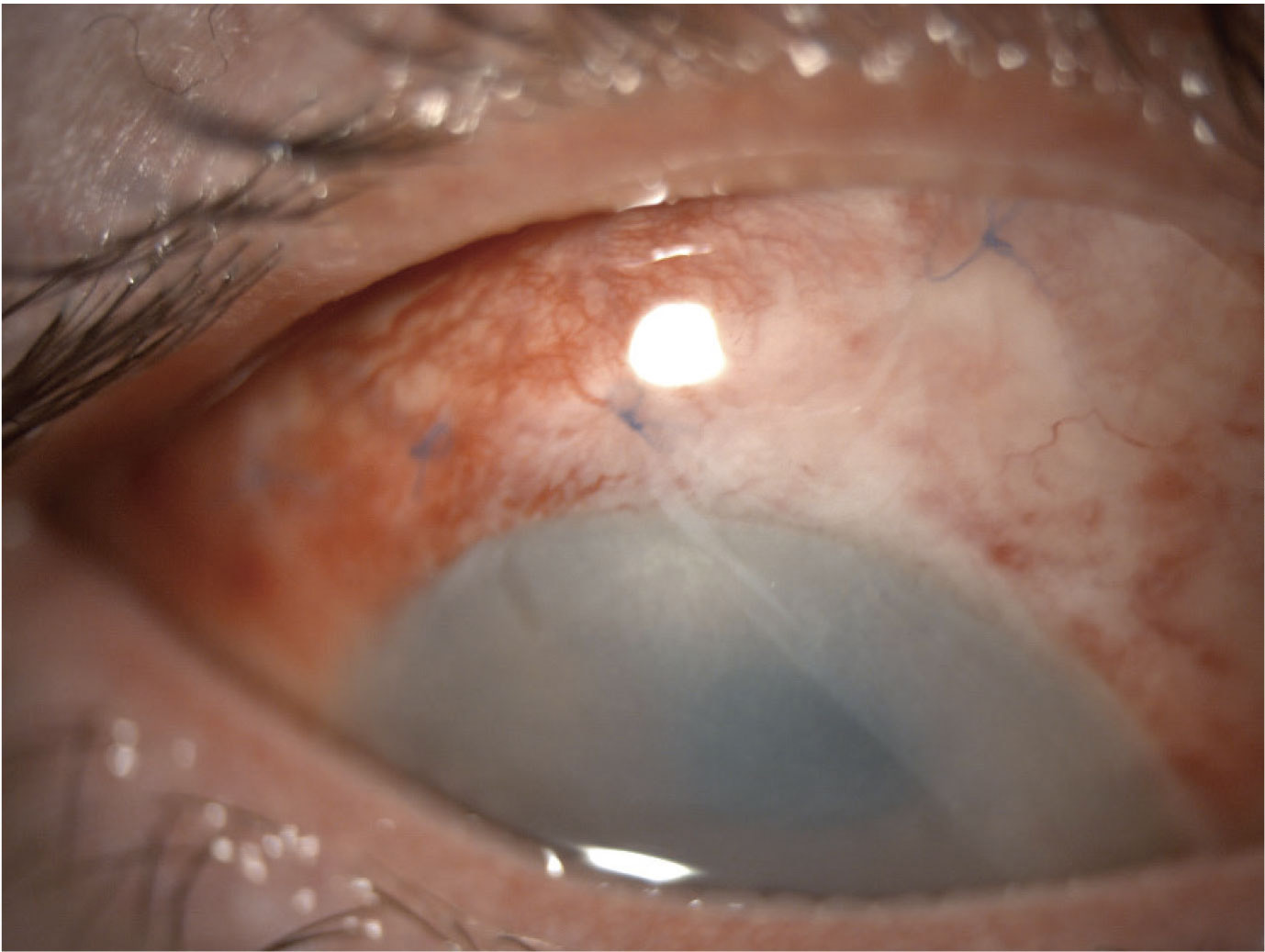
The Roper Hall classification system characterizes the corneal injury based on corneal involvement (e.g., epithelial damage, corneal haze, corneal opacification) and the amount of limbal ischemia (Table 2). Both systems are used in clinical practice, with varying evidence in the literature for their prognostic values.
 |
Medical Management
Conventional medical management for chemical injury focuses on controlling inflammation in the eye and creating an optimal healing environment.
The body and eye respond to chemical injury by producing inflammatory factors, and this inflammatory response can precipitate further damage even beyond what the chemical itself did. Early on, medical treatment should focus on limiting inflammation by promptly administering a topical corticosteroid such as prednisolone acetate. For severe chemical injuries with limbal involvement and corneal opacification, start with a high-frequency dose, about every one to two hours. For milder injuries, administer corticosteroids four times daily. Steroid dosages must be decreased and tapered within the first week or two to allow the eye to heal.
For cases with epithelial defect or any range of injury, antibiotics are given to prevent infection. A cycloplegic such as atropine or cyclopentolate can be given for comfort.
There’s evidence for using 1% medroxyprogesterone as an alternative to a corticosteroid or after corticosteroid treatment. This progestational steroid also limits inflammation, but as a collagenase inhibitor, it allows for stromal repair to take place. Oral doxycycline, another collagenase inhibitor, and vitamin C, which promotes collagen synthesis, also foster healing. Oral vitamin C is commonly used, but there’s also evidence for using 10% ascorbic acid drops applied hourly.
To promote healing, it’s important to keep the eye well-lubricated. Preservative-free artificial tears can be given hourly. Autologous serum tears or platelet-rich plasma are options with similar efficacy for severe dryness.
 |
|
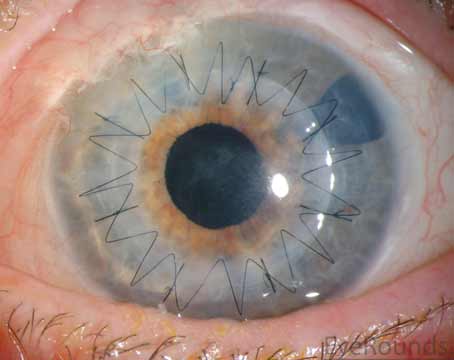
Figure 2. Sutured amniotic membrane. |
When assessing dryness, pay special attention to the eyelids and how they sit. Chemical injury management often warrants an interdisciplinary approach with oculoplastics to address other issues that contribute to dryness such as scarring, symblephara and lagophthalmos. A temporary tarsorrhaphy early on can help with healing if the eyelids aren’t apposing well.
If necrosis occurs early on, debride the epithelium and place an amniotic membrane to aid corneal healing. Amniotic membrane transplantation (Figure 2) or mucous membrane grafting is also used in cases requiring fornix reconstruction or with significant conjunctival involvement. Timing is important when using amniotic membrane for chemical injuries. It’s most effective when applied within the first two weeks.
Surgical Management
When it comes to surgical intervention, set yourself and the patient up for success and wait for the right conditions. I always counsel patients with severe chemical injury that the road to healing is a slow one. There are several steps, and much of it consists of waiting and continuing the same treatment until the eye is at a point where it’s ready for surgery.
At the two- to three-week point, begin assessing the level of limbal stem cell involvement and damage. However, before undertaking any surgical treatments, ensure the eye has healed and the ocular surface and tear film have improved. If oculoplastics needs to intervene with the eyelids, this should absolutely be done before turning to the limbal stem cells. While a limbal stem cell transplant could be done as early as two weeks, it’s generally best to wait and perform the procedure on a non-inflamed eye.
 |
|
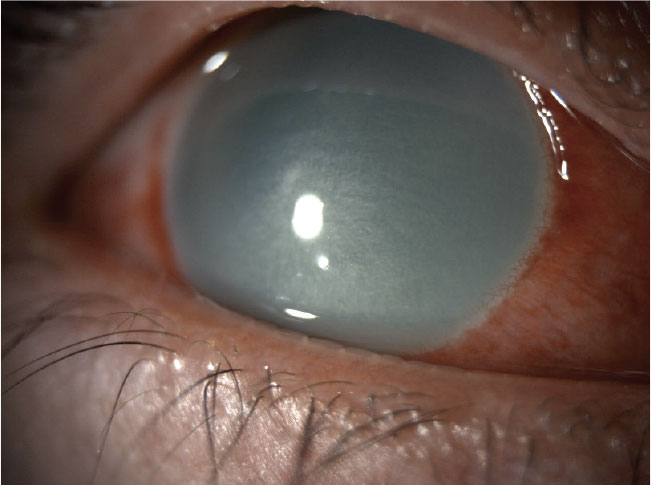
Figure 3. One week after conjunctival limbal autograft. |
 |
|
Figure 4. One month after conjunctival limbal autograft with reduced vascularization at graft sites and healed epithelium. |
There are three primary types of limbal stem cell transplantation:
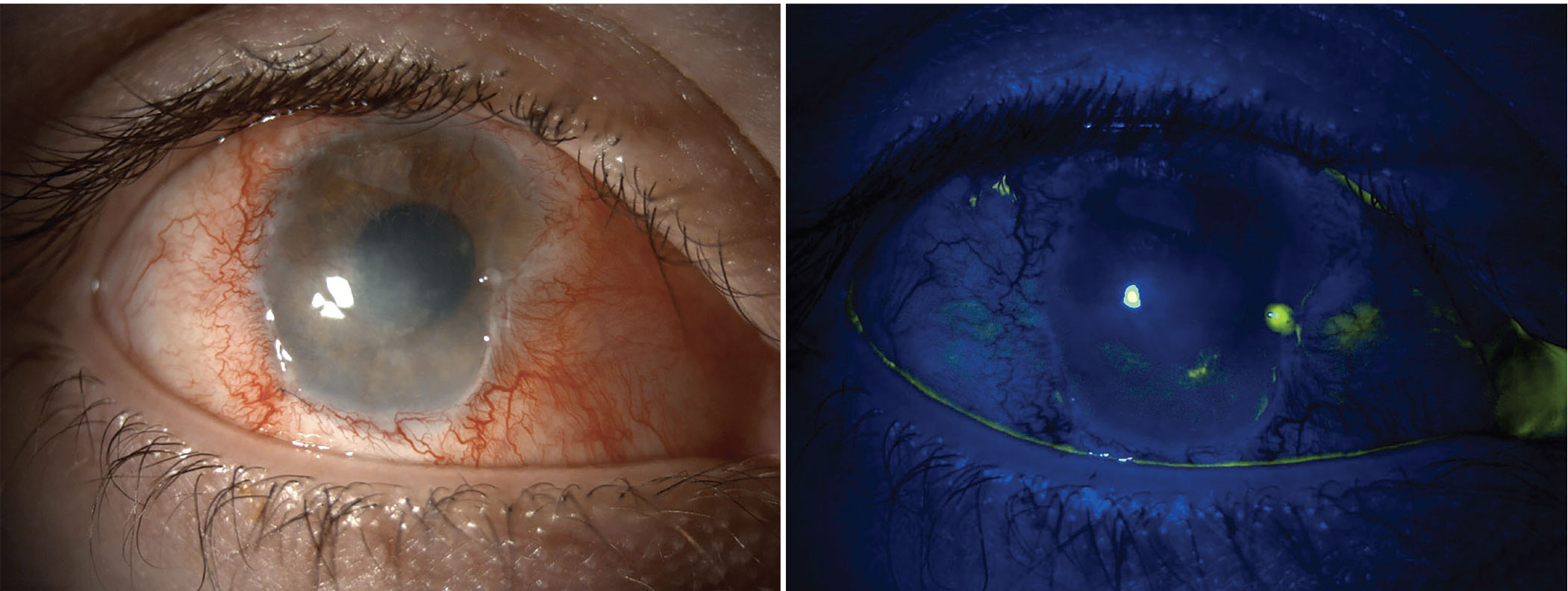
• Conjunctival limbal autograft. If the patient’s chemical injury is unilateral and the fellow eye is healthy, consider an autograft procedure (Figures 3 and 4). Before doing a transplant, be sure to remove any scarring or pannus.
From the fellow eye, excise 4 to 6 clock hours of limbal tissue and a small amount of adjacent conjunctiva. Avoid taking too much tissue from the healthy eye, as this carries the risk of that eye developing limbal stem cell deficiency. Divide the limbal tissue into two segments and place them on the recipient eye about 12 clock hours apart. This tissue will integrate into the recipient eye to aid corneal re-epithelialization and reduce any conjunctivalization that’s occurred with the limbal stem cell deficiency. (View a video of this procedure below.)
• Conjunctival limbal allograft. If the patient has a bilateral injury, an allograft procedure may be needed. Limbal stem cell donor tissue can come from a living relative or a deceased donor in the form of a cadaveric transplant. This approach is effective, but it’s accompanied by the risk of graft rejection and the need for the patient to be on systemic immunosuppression.
• SLET. An alternative to an autograft, simple limbal epithelial transplantation is suited for patients with unilateral injury and one healthy eye. SLET involves the removal of a 2 x 2-mm strip of limbal tissue from the healthy eye. This strip is divided into eight to 12 several smaller fragments, which are then placed epithelium-side up on top of an amniotic membrane covering the entire cornea and adhered using fibrin glue such as Tisseel. A bandage contact lens is placed on top.
Choosing among these procedures depends on the eyes involved, the state of the fellow eye, the patient’s preference and the conditions under which the transplant would take place.
As the transplant heals, re-epithelialization will occur and any pannus will begin to regress. Injection will also decrease. When limbal stem cell function is evident, it’s then time to determine, based on the severity of the injury, whether or not a full-thickness corneal transplant is needed, such as in cases of significant scarring.
Full thickness corneal transplants for severe chemical injury will have greater likelihood of success after a limbal stem cell transplant has been completed, and with a minimum of six weeks between the two surgeries. In the absolute worst-case scenarios, if a first or even second penetrating keratoplasty isn’t effective, a keratoprosthesis may be needed. This is typically a last resort.
In summary, when confronted with ocular chemical injury, it’s important to stage the patient and counsel them carefully about all the levels of management that may need to happen. Be sure to emphasize that early management—reducing inflammation, improving the tear film and optimizing the healing environment—is critical for success later on.
Dr. Palazzolo is a clinical assistant professor at the New York University Grossman School of Medicine Department of Ophthalmology. She’s also the medical director for ophthalmology at the NYU Langone Hospital, Long Island; NYU Langone Ambulatory Care, Garden City; and Huntington Medical Group. She has no related financial interests.