This year, contact lens researchers have uncovered new information in multiple areas: risk factors for microbial keratitis; characteristics of wearers' refractive errors, lens use and care regimens; how contact lens wear affects myopia progression; new data regarding orthokeratology; the toxicity of cleaning solutions; and new ways to increase contact lens wear by combating dry eye. (Unless otherwise noted, studies received no commercial support.)
Decreasing Lens Wear Risks
Researchers at seven universities and research centers in
The data showed that independent risk factors were: wearing CLs every day, compared with less frequent use (odds ratio 6.0x); overnight wear, compared with daytime-only use (OR 1.2x); less frequent hand washing (OR 3.2x); smoking (OR 1.7x); and having allowed more than one year to elapse since the last aftercare (OR 1.8x). Younger age and more frequent checkups were protective (OR 0.2x). Risk varied with CL type, material properties and design.1305
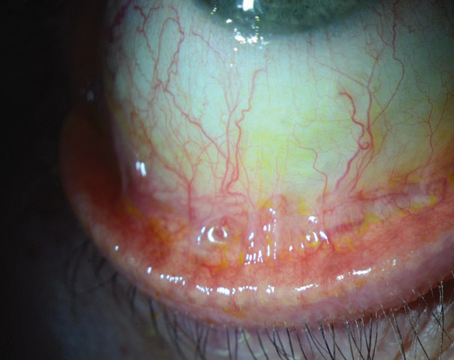
Researchers at the
The cells were then treated with one of four commercially available cleaning solutions or a 0.01% solution of benzalkonium chloride in phosphate-buffered saline. After one hour, they assessed loss of cell surface mucins (using rose bengal staining); cytotoxicity (using an MTT assay); the presence of mucins -1, -4, and -16 in cell extracts and the cleavage of these mucins into the media (using western blotting); and mucin mRNA levels (using semi-quantitative RT-PCR). Data showed:
• Only BAK had a significant cytotoxic effect on HCLEs.
• Treatment with BAK or solution #3 (containing aldox, polyquad and EDTA) significantly reduced the ability of HCLEs to exclude the rose bengal dye, indicating increased susceptibility to infection.
• In contrast, treatment with solution #2 (containing polyhexamethylene biguanide) increased dye exclusion.
• None of the treatments caused a significant change in mRNA or intracellular protein levels.
• Solution #3 increased the levels of Muc-16 cleavage into the culture medium.
• Cells treated with solutions containing EDTA were significantly less adherent to the culture dish, although cell survival rates were not affected.1536
Researchers at the University of Texas Southwestern Medical Center in
Each patient was asked 26 questions regarding his lens care practices and knowledge about contact lens use and potential risks.
Of these patients, 86.4 percent perceived themselves as compliant with their prescribed lens care regimens, and 79.6 percent reported an awareness of risk factors associated with lens wear. Nevertheless, 40.7 percent reported a positive history for some form of contact lens-related complication; 14.2 percent admitted to sleeping in lenses; 29 percent reported wearing lenses longer than recommended; 24.1 percent admitted replacing lenses less frequently than recommended; 27.8 percent admitted swimming in their lenses; 6.8 percent topped off their care solutions regularly, with an additional 3.1 percent topping off occasionally; 22.2 percent did not replace their lens cases and 6.7 percent admitted they didn't wash their hands. The study authors note that extrapolation of these numbers over the entire contact lens wearing population could explain, in part, the persistent incidence of infection associated with lens wear.1514
Increasing Lens Comfort
A doctor at the Southern College of Optometry in
After treatment, TBUT increased from 3.1 ±1.37 to 7.69 ±3.5 seconds. Schirmer test scores also increased, from 8.17 ±5.9 mm to 11.79 ±4.26 mm. Contact lens wear time increased from 6.54 ±5.28 hours to 12.4 ±3.64 hours. All three increases were statistically significant (p=0.05).
The author notes that six of the study patients were unable to tolerate contact lens wear before the study; using the cream, all are now able to comfortably wear contact lenses.6271
Characteristics of Lens Wearers
In a study supported by CIBA Vision, the charts of 3,549 soft contact lens patients from 8 to 33 years old were reviewed at six clinics at colleges in
At the baseline visit, 63 percent were between
• More than 15 percent of 8- to 12- year-olds wore lenses with power >+4 D; 15 percent of 26- to 33-year-olds wore >-6 D.
• A significantly higher percentage of 8- to 12-year-olds had hyperopic lens power (r:+0.25 to +8 D), compared to 13- to 33-year olds (p<0.0001).
• A significantly greater percentage of the 26- to 33-year-olds demonstrated myopia >-6 D (p<0.0001). (See chart, above.)
Other findings: The highest rate of anisometropia (>1 D spherical equivalent difference between eyes) was 14 percent among the 8- to 12-year-olds, compared to 9 percent of the 13- to 33-year-olds (p=0.006); there was a higher frequency of daily disposable prescriptions for 8- to 12-year-olds compared to all others (p=0.04); and toric prescriptions were less likely among 8- to 12-year-olds (p=0.09).1512
A study conducted at the
Based on the data, the author estimates that during these years:
• 18.6 million Americans over age 10 who used refractive correction for distance vision (18.7 percent) used contact lenses;
• Contact lens use was highest among teens aged 10 to 18 (39 percent) and young adults aged 18 to 40 (37.1 percent). Use decreased to 5.7 percent in adults over age 50.
• Non-Hispanic whites accounted for the majority of contact lens wearers (77 percent). Within-ethnic-group analysis showed that contact lens use was highest (21.3 percent) among those identified as Mexican-American and those not classified as white, Hispanic or African American (21.3 percent). Usage was lowest among African Americans (14.6 percent).
• Females were more frequent users of CLs at all ages, and there were
more than twice as many female wearers in the population over age 50.1516
Mitigating Myopia Progression
In a study funded by the Institute for Eye Research, CIBA Vision and the Australian Government, researchers in Sydney, Australia, Guangzhou, China and Dallas, Texas, found that Chinese children wearing silicone hydrogel contact lenses experienced less myopia progression than those using single-vision spectacles, over a six-month period.
In the study, 33 children wore spectacles and 43 wore Lotrafilcon B lenses (CIBA Vision) on a daily-wear basis. Subjects were 7 to 14 years of age with a baseline spherical refraction between -0.75 D and -3.50 D and cylinder ≤0.50 D. Inves-tigators measured cycloplegic central autorefraction, peripheral refraction along the horizontal meridian (20-, 30- and 40-degree nasal and temporal fields) and axial length. They analyzed the relationship between myopia progression and peripheral refraction at each field angle.
After adjusting for parental myopia, gender, age and prescription, myopia progression was 38 percent less for SHCL wearers (-0.37 ±0.29 D) than spectacle wearers (-0.60 ±0.29 D) (p<0.001). Similarly, axial length increase was 44 percent less for SHCL (0.14 ±0.12 mm) than spectacle wearers (0.25 ±0.12 mm) (p<0.001). Spectacles produced greater peripheral hyperopic defocus than SHCLs for all field angles except for 40 degrees nasal field (temporal retina). (Myopia progression was significantly affected by baseline age [p=0.031] but not by prescription or gender [p>0.05]).
The study authors conclude that the faster myopia progression observed in spectacle wearers may have been due to higher amounts of relative peripheral hyperopia.2198
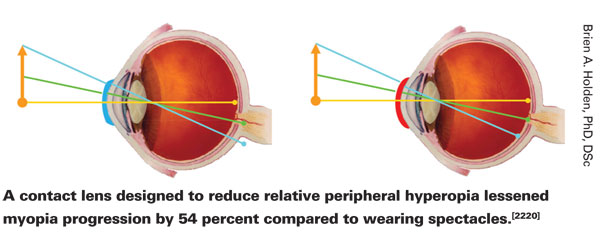
A related set of findings came from a separate study sharing many of the same authors as the previous study, with partial funding from CIBA Vision. The authors set out to determine whether a silicone hydrogel contact lens (referred to as AMCL) designed to maintain clear central vision while reducing relative peripheral hyperopia would reduce the rate of myopia progression over a six-month period. Sixty-five Chinese children aged 7 to 14 years with baseline spherical myopia between -0.75 to -3.50 D and cylinder ≤0.50 D, wearing AMCL, were compared to 50 children wearing normal spectacles.
Investigators measured the change in spherical equivalent refractive error (using cycloplegic auto-refraction) and axial length.
• Children wearing AMCL experienced significantly less myopia progression (-0.26 ±0.25 D), than children wearing spectacles (-0.60 ±0.29 D) (p<0.01). Similarly, axial length increase was less with AMCL (0.08 ±0.11 mm) than with spectacles (0.25 ±0.12 mm) (p<0.01).
• After adjusting for lens type, parental myopia, gender, age and baseline spherical equivalent values, estimated progression in spherical equivalence was -0.29 D wearing AMCL (SE 0.04), compared with -0.63 D wearing spectacles (SE 0.04).
• Axial length changed 0.10 mm with AMCLs (SE 0.02 mm), compared with 0.25 mm for spectacle wearers (SE 0.02).
The authors note that the AMCL lessened the progression of myopia by 54 percent compared to wearing standard spectacles.2220
Researchers at the
Forty children with progressing myopia, 11 to 14 years old, wore a DF lens in one randomly assigned eye and a SVD lens in the fellow eye for 10 months. Lens assignment was then swapped between eyes and lenses were worn for an additional 10 months. Control group subjects wore single-vision distance lenses. (Visual acuity and log contrast sensitivity were not significantly different between the two lens types.)
Investigators monitored spherical equivalent refraction, axial length and accommodation every five months.
There was significantly less myopia progression and eye elongation in eyes wearing dual-focus lenses compared to single-vision lenses. Mean reductions in myopia and eye elongation during the first 10 months were: 0.252 ±0.273 D and 0.107 ±0.080 mm (p<0.0001). During the second 10 months reductions were 0.204 ±0.338 D and 0.115 ±0.099 mm (p<0.001). The ratio of progression with DF lenses vs. single-vision lenses was approximately 0.55:1 for control progression rates between 0 and -1.50 D in each of the 10 month periods.2232
New Data on Orthokeratology
Researchers in
At the initial visit, the mean K- reading at the flat meridian was 42.73 D (r: 39.50 to 45.25); by the final visit, this was reduced to 41.25 D (r: 37.75 to 44.25). Initial mean refraction was: spherical -3.20 D (r: 0 to -9.50) and cylinder -0.59 D (r: 0 to -1.75). This was reduced to: spherical +0.03 D (r: +1.50 to -1.50) and cylinder -0.50 D (r: 0.00 to -2.00). Mean logMAR visual acuity improved from 1.12 (r: 0.1 to 1.7) to -0.01 (r: -0.2 to 0.7). Eighty-five percent of subjects came within ±0.50 D of the target spherical correction.
In patients under 18 years old, OK patients stayed with their initial correction. In contrast, myopia correction required tended to increase yearly for others; observed increases were -0.18 D for soft lenses, -0.42 D for hard lenses, and -0.31 for spectacles.
Complications observed during the five-year period included: OK patients—14 percent experienced slight-to-moderate superficial punctate keratitis; 9 percent, allergic conjunctivitis; and 3 percent, dry eye. Among control subjects, 3 percent, 9 percent and 3 percent of those wearing soft lenses, and 5 percent, 6 percent and 2 percent of those wearing hard lenses, respectively, experienced the same complications.1528
In a study funded by the Australian government, researchers at the University of New South Wales investigated the effect of wearing orthokeratology lenses on axial length in 14 East Asian children (ages 10 to 17 years) with progressive myopia. The subjects were fitted with reverse geometry lenses (BE; Capricornia) for overnight orthoK in one eye, and conventional rigid gas-permeable lenses (J-Contour; Capricornia) for daily wear in the contralateral eye. Lens/eye combinations were randomly assigned; lens fittings and adaptation to rigid lenses were optimized prior to the study. The lenses were worn for six months; then, after a two-week washout without lens wear, the lens-eye combinations were reversed and lens wear continued for six more months. Axial length was monitored at baseline and three-month intervals.
At the outset, axial length was 24.96 ±1 mm and 24.97 ±0.95 mm in the orthoK and conventional GP lens-wearing eyes, respectively. After six months of lens wear there was a significant difference in axial length between the eyes (RM-ANOVA, F=3.049, p=0.012).
Axial length in-creased by 0.06 ±0.09 mm in the RGP eye (p=0.014), but showed no significant change (-0.02 ±0.08 mm) in the OrthoK eye (p=0.348). During the second six months, axial length in the RGP eye increased by 0.11 ±0.11 mm (p=0.002); in the orthoK eye there was no significant change in axial length (-0.02 ±0.12 mm; p=0.460).
Interestingly, during both lens-wearing periods axial length decreased significantly at three months in the orthoK lens-wearing eye (p<0.038), followed by apparent return to baseline values. In contrast, the RGP eyes showed progressive axial length growth.1721
A related study, also designed to observe the effect of orthokeratology on axial length, was conducted by researchers at the
Changes in axial length during a two-year period were compared. Axial length in the orthoK group increased by 0.39 ±0.27 mm; axial length in the control group increased by 0.61 ±0.24 mm, a significant difference (p<0.0001). The study authors concluded that orthoK did suppress axial length elongation and might be an effective means to reduce myopia progression in myopic children.2195
Dr. Asbell is a professor of ophthalmology and the director of cornea and refractive surgery at the Mount Sinai School of Medicine.