These are a couple of the revelations in this month’s survey of surgeons about their cataract techniques. The e-mail survey was opened by 1,742 of 11,600 subscribers to Review’s electronic mail service (15 percent open rate) and 181 filled in their answers. To see how your cataract technique compares to the surgeons on the survey, read on.
Burgeoning Technology
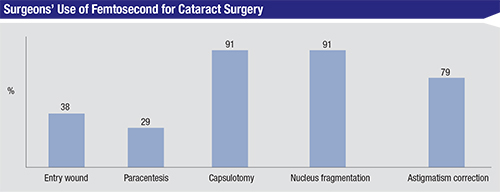
Cataract surgeons seem to be warming up to the idea of femtosecond cataract, with the percentage saying they use it for some aspect of cataract surgery growing from 23 percent on last year’s survey to 31 percent this year. The steps the laser is used for most often are the capsulotomy (91 percent of respondents) and nuclear fragmentation (91 percent). The percentage who say they use it for the entry and paracentesis incisions actually decreased from last year, however. Last year, 64 percent used it for the entry wound and 55 percent used it for the paracentesis, compared to just 38 percent and 29 percent, respectively, this year. The full results appear in the graph on p. 46.
The surgeons who currently use the technology appreciate many of the things it does for them, but note that it’s not perfect. John Sheppard, MD, of Norfolk, Va., is one of these physicians. “I enjoy the procedure,” he says. “It’s an excellent marketing tool, and has outstanding advantages for capsulorhexis and LRIs. I’m enjoying newer nucleus fragmentation techniques like the ‘ice cube.’ The paracentesis and primary incisions don’t yet have a clear-cut advantage, though. It’s still costly, but our fastest growing single segment of premium surgery is the LenSx.”
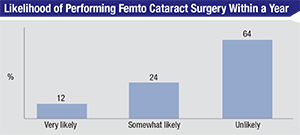 |
Looking ahead, 12 percent of the surgeons say they’re very likely to perform femtosecond cataract surgery in the next year, and 24 percent say they’re somewhat likely to do so. The main reasons given are, “it’s the future,” or “patient demand.” On the other hand, 64 percent say they’re unlikely to do it, though this percentage is down from last survey’s 73 percent. The main reason given by many of the uninterested surgeons is the cost/benefit ratio. “It works OK but is too cumbersome to align the patient,” says an Ohio surgeon who tried the technology but is unlikely to go back to it. “There’s too much of a reliance on the technician, too many extra steps where things can go wrong or out of your control, it takes too long and is expensive without any clear advantage to the patient. The technology is not currently advanced enough to be worth the hassle.”
Richard Erdey, MD, of Columbus, Ohio, also says he’s unlikely to use femtosecond for his cataract surgeries. “There’s no peer-reviewed paper demonstrating any advantage of it versus a very efficient two-handed phaco chop technique,” he avers. “There’s also no peer-reviewed report demonstrating the long-term predictability and stability of vertical corneal incisions made with the femto versus those made with steel or diamond blades. I prefer lamellar AK techniques such as bilateral clear cornea incisions. I like scleral tunnel on the steep, with-the-rule axis (scleral recession) and LVC when a toric IOL isn’t indicated or is unaffordable.”
 |
 |
 |
The other technology in contention for cataract surgeons’ attention is intraoperative wavefront aberrometry. Twelve percent of the surgeons say they use it, which is up slightly from last year’s 9 percent, and 34 percent say they’re either very likely or somewhat likely to use it in the coming year, which is an increase over last year’s 26 percent. However, this means 88 percent of the respondents don’t use it, and two-thirds say they’re unlikely to using doing it this year.
Sacramento, Calif., surgeon Richard Meister says he appreciates the technology. “It yields good readings on post-refractive patients and those that we can’t do the IOLMaster on,” he says. “It’s good for acquiring the astigmatism and the axis.” Robert Lehmann, MD, of Nacogdoches, Texas, also feels it helps him in the OR. “My outcomes are closer to the target,” he says. “I’m also able to adjust the cylinder and the toric IOL position at the expense of a little extra time and cost.” Another surgeon from Texas warns that it might not be perfect for all cases, though, when he says, “It’s sometimes finicky for low-power toric IOL alignments.” A New York surgeon thinks it comes in handy for patients who are usually difficult to pin down on biometry. “It gives me an accurate intraocular lens measurement in the post-LASIK patient,” he says. Nick Mamalis, MD, of Salt Lake City, however, thinks the technology plays a key role in some cases. “It’s essential to have this technology for patients who have had previous refractive surgery and/or have astigmatism,” he says, “especially with toric IOLs.”
Many of the 88 percent who don’t use intraoperative aberrometry say that they’re concerned it will slow them down during surgery without giving them a commensurate benefit. Will Sawyer, DO, of New Braunfels, Texas, says, “The benefit is the ability to recheck your IOL calculations intraoperatively. The cons are cost, the time spent in surgery and the fact there’s not a 100-percent guarantee that the residual refractive error will be gone.” A surgeon from Nashville says he isn’t yet convinced. “My IOL predictions are sufficient, and studies have not yet shown significant result changes of greater than 1 D on a regular basis,” he says. “I don’t use it at this time. A true drawback would be that these lenses have to be ordered ahead of time. How do I know that my surgery center is going to have what I need at all times?”
A California surgeon is open to using the technology down the road. “It’s about affordability,” he says. “Someone has to fund the new technologies, so if the patients will pay for it—i.e., if enough of my practice’s patients will monetarily endorse intraoperative aberrometry—then we will invest in it.”
Managing Astigmatism
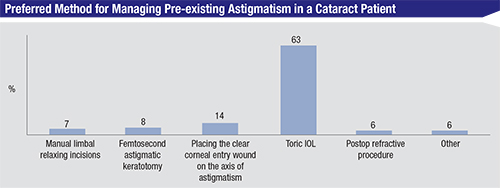
Surgeons also weighed in on their usual method for treating pre-existing astigmatism in their cataract patients.
The most popular option is a toric IOL, chosen by 63 percent of the respondents. In second-place is the practice of putting the entry wound on the steep axis (14 percent). “The toric IOL works reasonably well, is easy to implant and is profitable,” says New Jersey’s Dr. Liva. “The toric lens is a perfect example of capitalism working well: The industry benefits with increased profits for research, the physician benefits with increased reimbursement to compensate for the unfairly low cataract surgery compensation and the patient benefits with improved uncorrected vision without significant risk. It’s a triple win.” A Texas surgeon says that in most cases he uses the placement of the entry wound to control the cylinder. “I like to go on-axis for low-power cylinder,” he says. “Anything greater will require an additional AK or a toric lens. I like to reduce the power requirement of the toric IOL by operating on-axis.”
Phaco Technique
In terms of breaking up the cataractous lens, the most popular option on the survey is quadrant division, chosen by 48 percent of respondents.
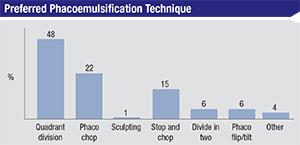 |
As for other techniques, 22 percent prefer phaco chop and 15 percent do stop-and-chop. Bettendorf, Iowa, surgeon Lisa Arbisser, explains why she prefers phaco chop: “The size of the rhexis is always tailored to the optic, not to the nucleus,” she says. “With vertical chop one stays in view within the rhexis and only requires a 5- to 6-mm pupil. One is never pushing on subincisional zonules. It’s the most ultrasound-sparing technique. One can adjust the number of sections split based on lens density so there is never a large chunk brought near endothelium. The posterior capsule is protected by the remaining nuclear sections in the bag until the last fragment is removed.”
A String of Pearls
Surgeons also took the time to share their favorite surgical techniques.
Kevin Dinowitz, MD, of Bloomfield, Conn., says to pay attention to the use of your viscoelastic. “I find it better to leave the viscoelastic under the toric IOL and not remove it as stated in the normal convention,” he says. “When it’s removed, the IOL actually is more likely to spin and move out of position.” Virginia’s Dr. Sheppard provides both conventional and femtosecond cataract advice: Use the primary blade to make the initial nick in the anterior capsule,” he says. “For femtosecond, be sure to complete your hydrodissection; it makes sub-incisional cortex removal much easier, and it’s much safer now, with smaller bubbles created by the lower laser energy and shorter treatment times.”
Ohio’s Dr. Erdey likes a scleral recession technique. “I perform scleral recession—a scleral tunnel placed on the steep corneal meridian with its length titrated to astigmatism magnitude—as a long-term, stable, reversible technique for correction of with-the-rule cylinder less than 2.5 D,” he explains. “I routinely perform scleral recession when a patient can’t afford a toric IOL or when it’s indicated because of mild corneal asymmetry or warpage.” Dr. Riego modifies his capsulorhexis for certain cases. “I make a bigger capsulorhexis for diabetics with retinopathy,” he says, “or for diabetics who are most likely going to develop retinopathy. I use it also for high myopes.” Thomas Castillo, DO, from Beaver Dam, Wis., says it pays to hit the film room. “Record every case,” he says. “You never know what you may learn by watching an instance when things don’t go perfectly.”
Ligaya Prystowsky, MD, of Nutley, N.J., shares a sentiment that most surgeons adhere to in the operating room and the clinic: “There’s always room for improvement.” REVIEW



