Cataract surgery and oculoplastics are interconnected. It’s important that we respect each other’s skills and specialties because the eyelids are, frankly, the protectors of the globe. What’s happening to the eyelids plays a huge role and impact on the health of the eyeball itself. The surface of the eye is directly affected by how well the eyelids close and how well they hug the surface in order to protect it from the external elements. There are many facets of oculoplastics aside from the eyelids, including lacrimal drainage and thyroid eye disease, which are also sometimes interwoven in cataract surgery patients.
There’s a joke that the eyelids get in the way of cataract surgeons operating on the eyeball, but for us as oculoplastic surgeons, the globe gets in the way of operating in the orbit. It’s important for cataract surgeons to be aware of the status of the eyelids when discussing surgery with their patients. If the eyelids aren’t in optimal position or shape, or if the patient has complaints of tearing, it’s important to consider an evaluation to see if there’s an obstruction of the nasolacrimal drainage system, which should be addressed before cataract surgery.
In this article we’ll cover some of the most common oculoplastic presentations, such as eyelid malpositions, eyelid lesions, lacrimal drainage and TED, and whether they should be addressed before or after cataract surgery.
Ptosis
Ptosis is one of the most prevalent eyelid malpositions and it can also occur post-cataract surgery.
If you’re evaluating a patient for cataract surgery and they have a significant amount of ptosis, this may affect your IOL calculations (i.e., if the lid is pressing down on the eye to a degree that’s actually changing the curvature of the cornea).
 |
|
One of the most common eyelid malpositions, ptosis can typically wait to be addressed until after cataract surgery, however, some research suggests that significant ptosis may induce astigmatism, leaving patients with a refractive surprise after eyelid surgery. |
A recent paper in the oculoplastics literature looked at the degree of astigmatism change with keratometry after lifting an eyelid with ptosis surgery (not involving cataract). According to the study, the mean axial change of corneal astigmatism was 17.4 degrees after ptosis surgery, and the average axial change of corneal astigmatism in a cohort with severe blepharoptosis after surgery was 22.7 degrees.1 So it turns out that a good amount of astigmatism can be induced by the eyelid.
The common teaching has been to proceed with cataract surgery before eyelid surgery (ptosis repair, blepharoplasty) because cataract surgery can sometimes induce ptosis from 1 to 20 percent of the time. Usually it’s a wait-and-see approach to prevent the patient from needing two eyelid surgeries, but I think what this new paper shows is that some of these patients might end up with a refractive surprise after lid surgery if their IOLs were calculated based on the astigmatism that might have been induced by the severely ptotic lid.
Therefore, there are cases of severe ptosis covering the pupil where I might recommend that ptosis surgery occur first to optimize accuracy of IOL measurements. It would be important to counsel the patient that ptosis may recur after cataract surgery, however.
Ptosis following cataract surgery is not uncommon in my practice. There are different thresholds of when cataract surgeons will refer these patients to me. Sometimes it’s only a couple of months after their cataract removal because patients are significantly bothered. Unfortunately, if they come too early postop, I might tell the patients to wait a little longer as the height of the eyelid may improve gradually over time—similar to traumatic ptosis. I have seen post-cataract ptosis go away after a few months and if a surgical decision was made too early, the patient may have undergone unnecessary surgery. In the meantime, I do like to offer patients the possibility of prescription eye drops to help elevate the eyelid temporarily.
Some other factors also play into the determination of addressing ptosis before or after cataract surgery, including:
• Vision impairment. How impaired are they by their vision vs. their ptosis? If the patient is in their 90s, they may not want to undergo multiple surgeries. With ptosis surgery in particular, it’s prudent to suspend all blood thinners, which temporarily increases the risk of heart attack or stroke. The benefits of ptosis surgery may not outweigh the risks of suspending all anticoagulation in some patients. In that case, it would be best to proceed with the cataract surgery just to enable the patient to get around and successfully complete their activities of daily living.
• Creating or aggravating dry eye. I’m very conservative when it comes to eyelid surgery in the setting of dry eye. If a patient has background dry eye that isn’t optimized, then I almost always turn them away from ptosis surgery or even blepharoplasty because any upper eyelid-elevating surgery has the potential to make dry eye worse. I usually send them back to their ophthalmologist to work on helping their ocular surface and once the clinical signs and symptoms of dry eye have improved, I can proceed with upper eyelid surgery.
Entropion and Ectropion
Cataract surgeons are more likely to refer entropion patients for correction before surgery because in these cases, the lower eyelid has become so lax that it’s actually rolling inward, causing that skin and the eyelashes to rub across the surface of the eye. It’s very irritating. However, one of the biggest risks with this is endophthalmitis. When you think about the amount of bacteria on our lashes and if that were to be wiping across or near a cataract incision or the wounds, it’s very unnerving.
With that said, one study showed a four-times higher risk of developing entropion of the lower eyelid in eyes that had undergone cataract surgery, compared with the fellow unoperated eye.2 I’ve heard anecdotally from colleagues that they’ve seen new onset entropion happen even within the first week or month postop.
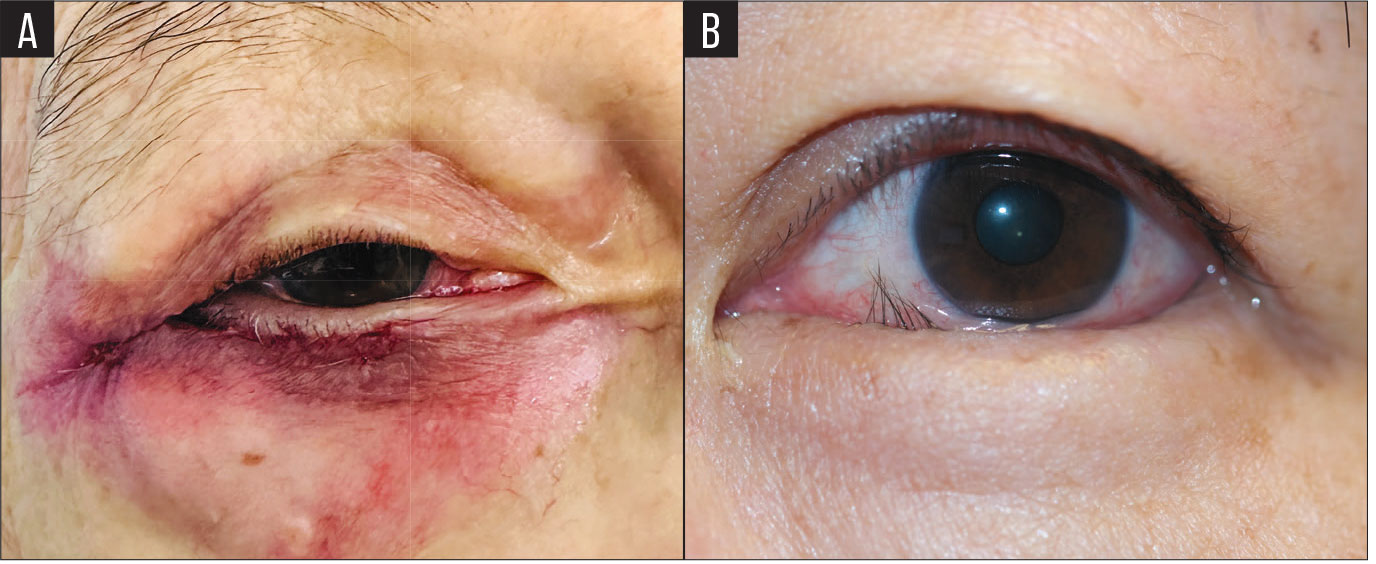 |
|
Entropion (A) and ectropion (B) surgery should occur ahead of cataract surgery due to their interference with the ocular surface. It’s recommended to wait at least three to four months before proceeding with cataract surgery to ensure accurate IOL calculations. |
One caution with entropion is that sometimes it’s not always there. Sometimes it’s the way that the patient moves their eye around or squeezes their eyes shut that causes or induces the entropion. Applying the speculum for cataract surgery can cause worsening of pre-existing looseness or laxity of the eyelid and that might theoretically generate the entropion or even ectropion later on.
In the case of ectropion, if the lid is loose and flipped inside out and you can see the inside of the eyelid facing out into the air, then you’re probably not going to have a healthy ocular surface or maintain important eye drops that are required after cataract surgery to prevent infection and inflammation. This could decrease the efficacy of post-cataract eye drops and it’s probably best to have the ectropion corrected prior to cataract surgery.
In order to correct entropion or ectropion, we sometimes over-tighten the eyelid knowing that in a few months or a few years, it’s likely to loosen back up again. In this over-tightening, it’s possible that the lower eyelid could push against the cornea—similar to ptosis—to a degree that causes an irregular astigmatism. I’d recommend waiting at least three or four months before cataract surgery just to make sure that the eyelid isn’t so taut up against the globe that it’s causing irregular astigmatism when IOL calculations are performed.
Lagophthalmos and Floppy Eyelid Syndrome
In facial palsy/lagophthalmos, the eyelids don’t close so they’re not protecting the globe. First, the patient should get worked up, and when the workup is complete, it may be necessary to improve the position of the eyelids with surgery. As oculoplastic surgeons, we perform any of the following surgeries: placement of an eyelid weight into the upper eyelid to weigh down the eyelid and improve closure; we can also tighten up the paralyzed lower eyelid to aid with closure. It’s also important to know the tempo of recovery—is this permanent or will it eventually improve? If temporary, eyelid surgery may not be necessary.
Floppy eyelids are highly correlated with sleep apnea. If the patient doesn’t know if they have sleep apnea, it’s imperative that they have a sleep study test to make sure it’s diagnosed and treated before having cataract surgery. When a person has sleep apnea, they tend to toss and turn and some people actually sleep on their face. This could lead to rubbing their eyelids and their face which continues to stretch them out. We do hesitate to perform floppy eyelid surgery unless the patient is controlled with their sleep apnea, uses a CPAP machine and is able to get a full night’s sleep without tossing and turning.
 |
|
In cases of lagophthalmos/facial palsy, oculoplastics surgeons will perform a workup to determine if the condition is temporary or permanent. If temporary, eyelid surgery may not be necessary. |
 |
|
Floppy eyelid syndrome is highly correlated to sleep apnea, often unbeknownst to the patient. A sleep study is recommended and if sleep apnea is confirmed, it should be under accurate management before proceeding with any surgery. |
Lesions: Benign and Suspicious
I see a good number of referrals for benign lesions that occur right on the edge of the eyelid at the waterline or margin, which can cause distortion in the ocular surface tear film. Benign lesions don’t always need to be removed before cataract surgery, but I have excised them to help cataract surgeons achieve more accurate calculations.
The approach is much different if the lesion is suspicious. I believe ophthalmologists are very good at identifying the warning signs. They look for madarosis (loss of lashes); they can look at ulceration; and they look at the telangiectasias. The most common suspicious lesion is basal cell carcinoma followed by squamous cell carcinoma, sebaceous carcinoma, and melanomas. These should be biopsied and diagnosed and treated before their cataract surgery.
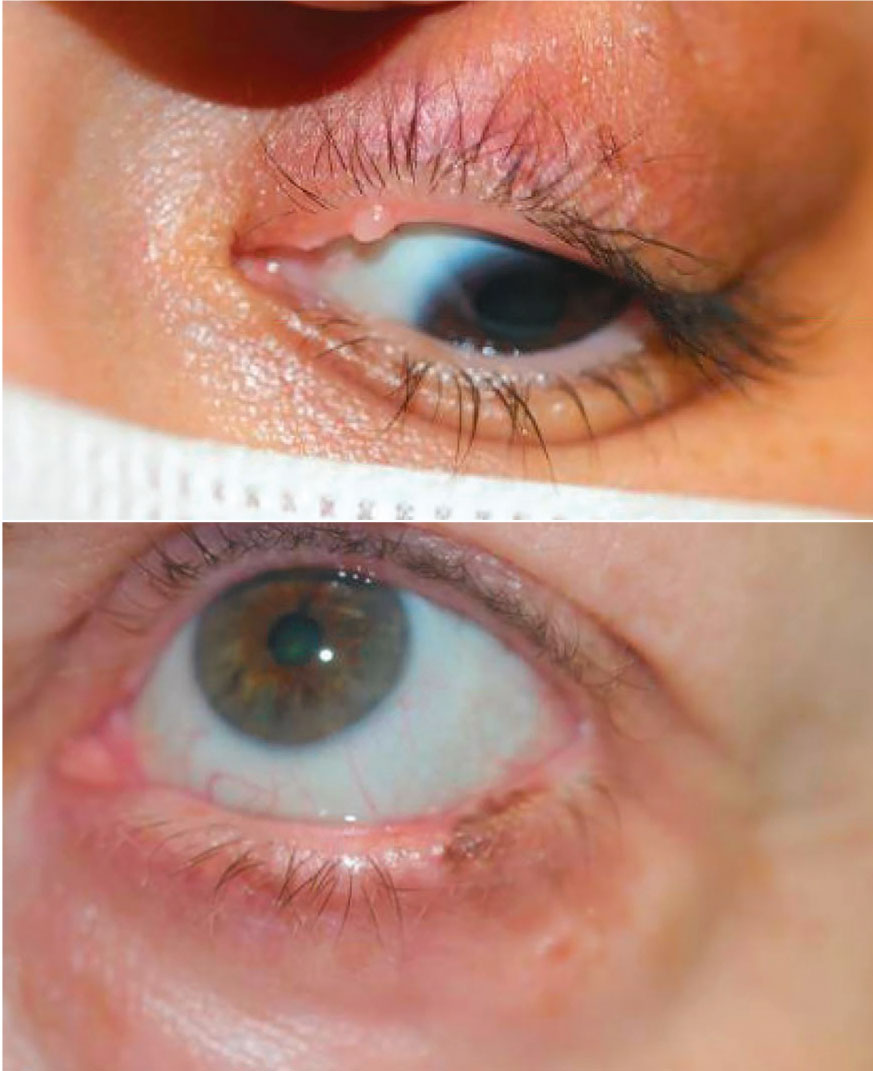 |
|
Benign lesions (top) don’t always need to be removed before cataract surgery, but doing so may help in IOL calculations. Alternatively, suspicious lesions (bottom) such as basal cell carcinoma, should be biopsied, diagnosed and treated ahead of time. |
Lacrimal Drainage Issues
These often get underdiagnosed and overlooked. In the case of dacryocystitis, an infection of the lacrimal sac, that would clearly need to be treated because the patient has an abscess near the eye that excretes pus. Obviously cataract surgery should be placed on hold until the infection is cleared. We would treat this with systemic and topical antibiotics followed by definitive DCR (dacryocystorhinostomy) surgery with stent placement. This stent is typically left in place for two to three months, but it shouldn’t interfere with cataract surgery.
Now, if the patient doesn’t have an infection and has simply an acquired nasolacrimal duct obstruction, the risk of dacryocystitis is still on my mind. The lacrimal sac is accumulating tears and harboring all of the blinked-off bacteria. Even if it’s not an overt infection, I wonder if there must be an in-and-out seeping of potential organisms.
In this instance, it’s probably a better idea to at least have a discussion with the patient regarding whether they want to proceed with an oculoplastic surgery first or if they want to accept the risks of potential infection. I think in some countries they do preoperative antibiotic drops and potentially oral antibiotics if they have a confirmed nasolacrimal duct obstruction, and they continue that through perioperative and postoperative courses. You could also consider DCR surgery prior to cataract surgery.
Thyroid Eye Disease
Thyroid eye disease is challenging because there’s such a wide spectrum. You may see a TED patient who has just a little bit of dry eye and may see another TED patient who has so much proptosis and compression of the optic nerve that they’re actively losing vision. Sometimes there’s some mild eyelid retraction.
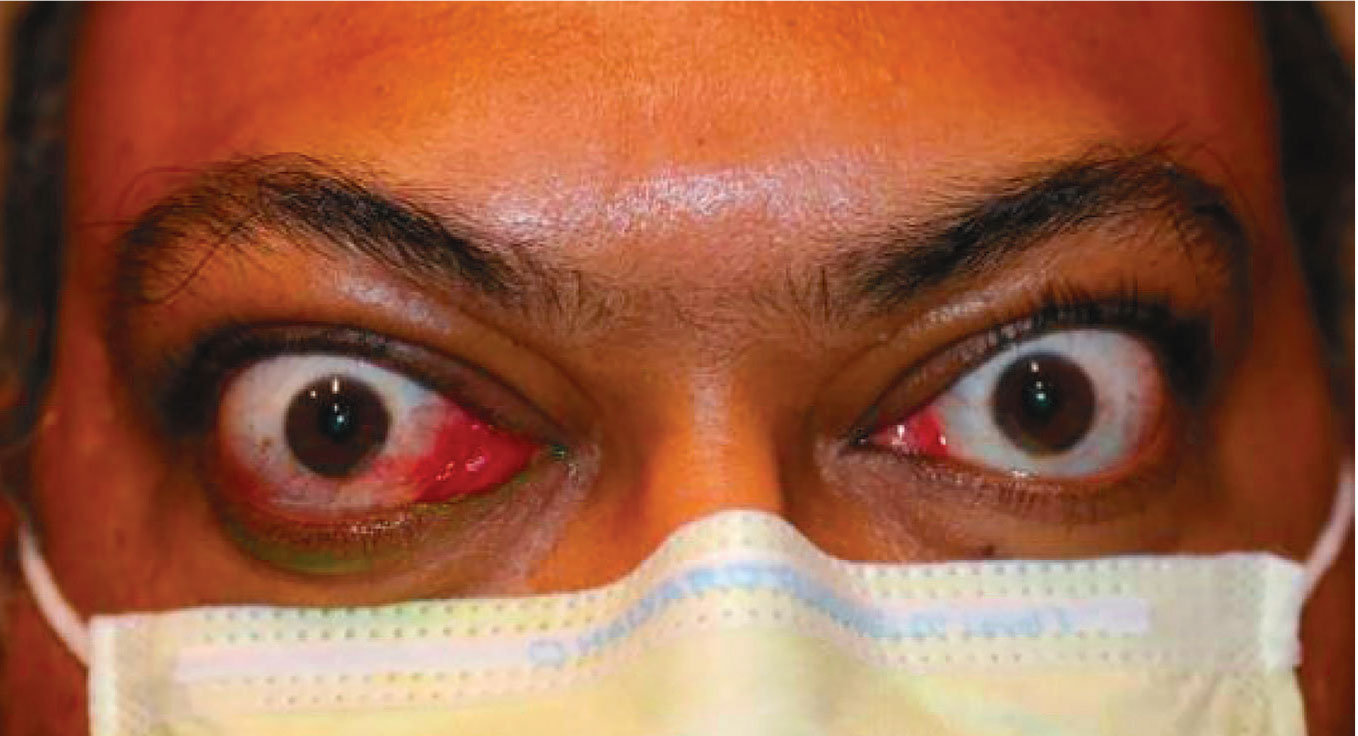 |
|
Thyroid eye disease runs a wide gamut of presentations among patients. If in its active state with fluctuating amounts of orbital pressure, TED should first be stabilized before proceeding with cataract surgery. |
Recently, a study that I came across looked at the refractive surprise in TED patients.3 They analyzed more than 5,000 eyes that underwent cataract surgery in their cohort, of which 1.1 percent had TED. Postoperatively, 13.8 percent of patients with TED had a refractive prediction error greater than ±1 D. The study didn’t specify if these patients had active or inactive TED, proptosis and orbital congestion, any eyelid signs or just dry eye—TED is a big bucket term—so it’s unclear what exactly was happening. I’d take that study with a grain of salt.
Theoretically, if there was significant pressure in the orbit and the globe from active inflammation of TED, your measurements of the length of the globe can be distorted. In the active state, TED is volatile and patients can have fluctuating amounts of orbital pressure, which could affect your IOL calculations. If TED isn’t in the active state, cataract surgery can very rarely reactivate TED.
In Summary
When facing oculoplastics issues in cataract patients, keep these points in mind:
• Upper eyelid malpositions can usually wait until after cataract surgery unless ptosis is very severe and can impact keratometry or corneal topography
• Laxity of the lower lids (entropion or ectropion) should generally be addressed before cataract surgery as the position of the lower eyelids impacts the health of the ocular surface
• Malignant or suspicious lesions should undergo biopsy and treatment before cataract surgery.
• Consider repairing lacrimal drainage problems before cataract surgery.
• Consider counseling TED patients about refractive surprise after cataract surgery.
• In general, allow two to three months of healing from oculoplastic surgery before scheduling cataract surgery.
1. Chen PJ, Lee YK, Lai CC. Significant changes of corneal astigmatism after levator muscle surgery for acquired blepharoptosis. Ophthalmic Plast Reconstr Surg. March 21, 2024. Epub ahead of print.
2. Schulz CB, Fallico M, Rothwell A, Siah WF. Lower eyelid involutional entropion following cataract surgery. Eye (Lond) 2022 Jan;36:1:175-181.
3. Strong Caldwell A, Patnaik JL, Ackerman M, Christopher KL, Lynch AM, Singh JK. Risk of refractive prediction error after cataract surgery in patients with thyroid eye disease. Clin Ophthalmol 2021;11:15:4431-4438.



