Ocular trauma represents a significant cause of visual morbidity associated with both individual loss of quality-of-life and a societal health burden. Annually, over 15,000 workers are injured in the United States alone due to eye trauma, with an associated $300-million dollar per year cost in treatment and lost productivity.1,2 Among the most devastating forms of ocular trauma are intraocular foreign bodies, which occur secondary to penetrating eye injury by a high-velocity object.3,4 IOFBs constitute one of a handful of ophthalmic emergencies and even with prompt identification and treatment can lead to devastating vision loss or blindness.3,4 Here, we’ll discuss the nature of various IOFB injuries and provide diagnostic and management tips to help you achieve the best outcomes.
IOFB Injury Background
The morbidity associated with IOFBs is closely tied to several characteristics including the mechanism of injury and material composition of the foreign body. The most ubiquitous cause of IOFB reported globally is hammering, especially metal-on-metal, followed closely by use of power tools and weapons or explosives.5–8 These mechanisms of injury typically introduce metallic IOFBs which can often lead to secondary chronic inflammatory responses such as chalcosis or siderosis bulbi in the case of copper or iron foreign bodies respectively.9,10 Organic IOFBs such as animal hairs, vegetable matter, or insect parts, in contrast, introduce contaminants and lead to higher rates of fulminant endophthalmitis.8,11,12 Other characteristics such as object shape, size, and trajectory can also impact prognosis. Sharp, regularly shaped foreign bodies tend to cause less damage to the eye than those that are irregularly shaped or blunt.13,14 Similarly, those that travel shorter distances within the eye are less harmful than those that ricochet or penetrate further posteriorly.15
Several studies have explored the evolving socioeconomic burden of IOFBs on a regional and international scale. Despite increasing awareness and actionable policies in countries such as the United Kingdom and Hong Kong, which have mandated protective eyewear in the workplace, the overall incidence of IOFB has been increasing since 2008, and the disability-adjusted life-years lost to IOFBs have also increased by nearly 50 percent since the early 1990s.16,17 Greater than 90 percent of patients who present with IOFBs are young working class males between the ages of 21 and 35, coinciding with previously described increased rates of trauma in this age group as well as a higher prevalence of manual labor and military service.5,16–18 Estimates of protective eye equipment use among workers in high-risk occupations such as construction varies from as low as 6 percent up to 20 percent, representing a significant proportion of potentially preventable injury.3,4,19 The development of practical policy changes is crucial to address this rising incidence of IOFBs.
A significant percentage of IOFBs are located in the posterior segment of the eye (reports place the incidence at between 42 and 69 percent).5,20 Posterior IOFBs require vitreoretinal surgical intervention for removal of IOFB, prevention of complications such as sympathetic ophthalmia and siderosis, and globe salvage.21,22
 |
|
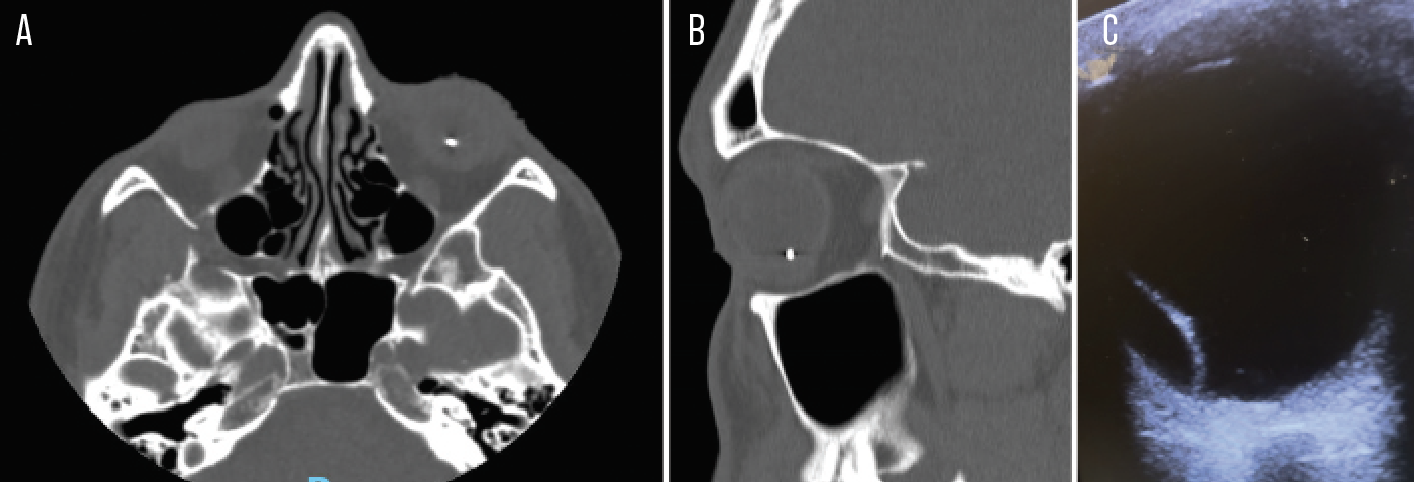
Figure 1. A case of an occult IOFB. A 28-year-old man presented 11 days after “feeling something get in [his] eye” while hammering wood and metal at work. On day one after injury, he had undergone dilated fundus exam at another facility and was diagnosed with vitreous hemorrhage and choroid rupture. A CT scan wasn’t performed. Ten days later, he presented to our emergency room with severe pain and vision loss, and underwent CT orbits which showed a metallic IOFB in the left eye (A, axial view; B, sagittal view; C, axial ultrasound scan showing hyperechoic area representing IOFB). By the time of presentation, he had developed Bacillus thuringiensis endophthalmitis. Despite systemic and intravitreal antibiotics, as well as attempted vitrectomy with IOFB removal, the eye was enucleated. |
Diagnostic Evaluation
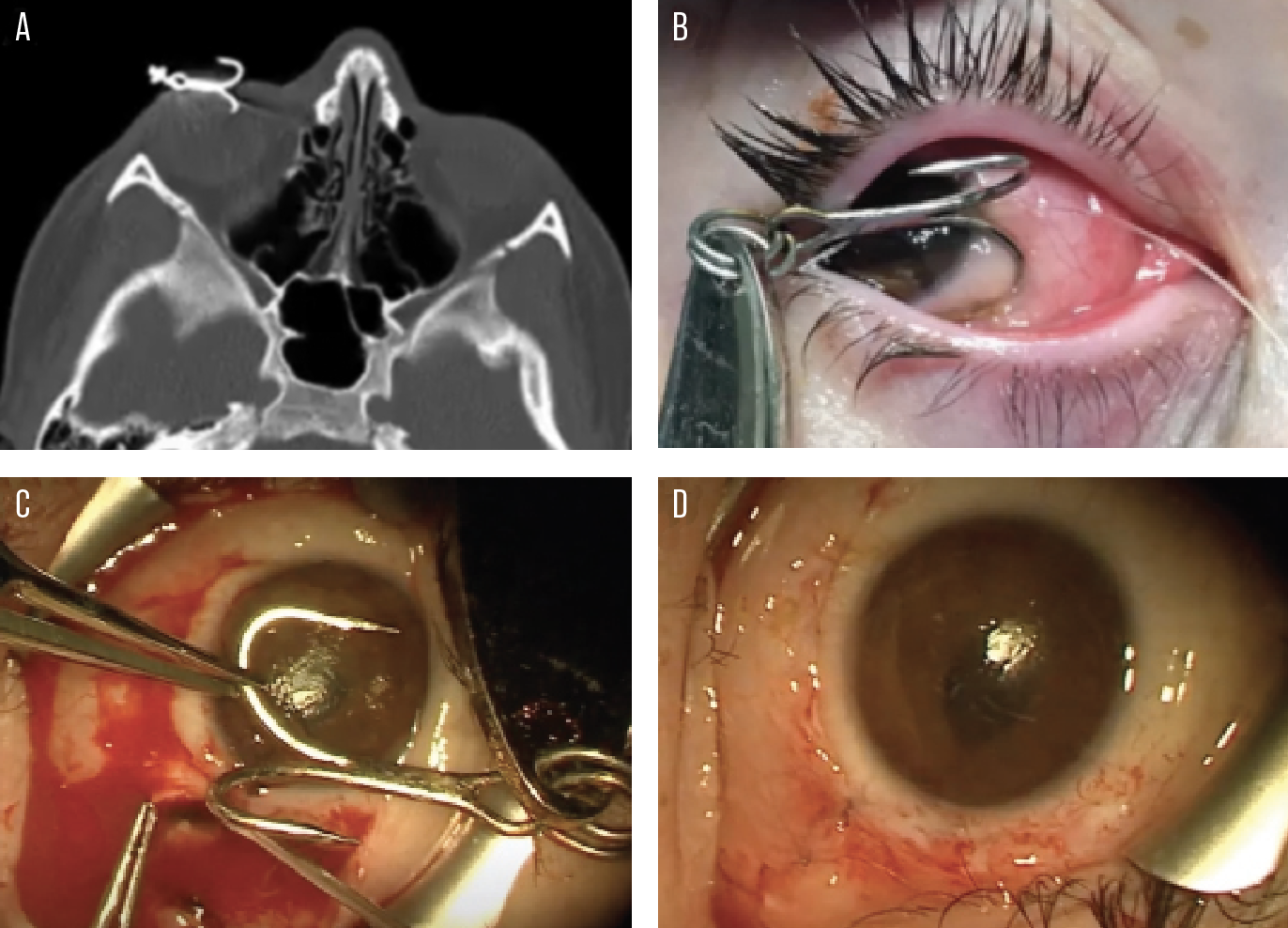
Posterior IOFB can present as an obvious penetrating injury, with or without concurrent open globe injury (OGI), or as an occult injury.8,13,15 See Figure 1 for an example of occult IOFB, and Figure 2 for an obvious penetrating injury. Urgent ophthalmic examination of any patient with concern for IOFB is appropriate.
First, obtain a thorough history, including details on how, where and when the initial injury occurred. Review the patient’s baseline vision, history of ocular disease and surgery, and medical history. Perform visual acuity testing, pupillary examination, extraocular movement examination, non-contact tonometry, slit lamp examination and dilated fundus examination, taking care to avoid any exertion of pressure on the globe, as IOFB is frequently associated with OGI.
 |
|
Figure 2. Case of fishhook IOFB. A 12-year-old girl presented immediately after a multi-pronged fishhook flew into her right eye. CT appearance of fishhook (A). Preoperative appearance of the fishhook IOFB (B). Intraoperative appearance of IOFB with inferior scleral laceration (C). Immediate postoperative appearance of eye (D). On postoperative day two, the visual acuity in this eye was 20/70, pinholing to 20/25. Luckily for her, the fishhook prong entered at the limbus and exited at the pars plana, sparing both the cornea and retina. Amazingly, she entered and won a golf chipping tournament just two weeks after the injury! Visual acuity at POM1 returned to 20/20. |
Obvious signs of OGI such as full-thickness corneal or scleral laceration, positive Seidel test or expulsion of uveal contents should prompt urgent surgical exploration, as delay in primary repair is associated with worse visual outcome and a higher risk of endophthalmitis.23–25 Though you should consider the possibility of IOFB in any patient with OGI, some mechanisms of OGI are associated with higher risk of IOFB than others: Patients with mechanisms of injury involving high-velocity projectile objects (e.g., gunshots, explosive devices, blast injuries and motor vehicle accidents), grinding or hammering of metallic or organic objects, or shattering of objects close to the face are considered at higher risk of IOFB.13,15,26,27
Patients aren’t always aware that they’ve experienced a penetrating ocular injury, and there’s not always an obvious entry wound or globe rupture.13 Many cases of delayed diagnosis of posterior IOFB have been reported,28,29 often with poor visual outcome due to siderosis30 or endophthalmitis.31 Clinicians should maintain a high index of suspicion of IOFB in patients who report any history of injury involving the high-risk mechanisms described above on their initial evaluation. In the setting of a high-risk injury, presence of focal traumatic cataract, peaked pupil, focal iris transillumination defect, positive Seidel test, hemorrhagic chemosis, fresh hyphema or vitreous hemorrhage, or fresh retinal tear or detachment suggest the presence of IOFB, even in the absence of globe rupture.8,21,27
Orbital imaging can be critical in establishing IOFB diagnosis, especially in cases where IOFB is suspected but there’s no globe rupture or clinically visible IOFB. Computed tomography of the orbits, in thin slices (less than 1.5 mm), is preferred for IOFB and OGI diagnosis, as it’s readily available in the emergency setting, requires little cooperation from the patient, and doesn’t require handling of the globe.21,32 Orbital CT imaging is highly sensitive for IOFB, and can detect metallic IOFBs larger than 0.06 mm3 and glass IOFBs larger than 1.8 mm.3,33 Organic IOFBs, such as wood, plastic or clay, are more difficult to detect on CT than metallic IOFBs, but CT still surpasses other modalities in ability to detect these.34 Magnetic resonance imaging isn’t recommended for acute evaluation of IOFB because of the preponderance of IOFBs are metallic, with vastly different ferromagnetism depending on composition. MRIs are also difficult to obtain in a timely manner in the emergency setting.
If CT imaging is unavailable, plain radiographs of the orbit can detect metallic IOFBs in 70 to 90 percent of cases, with a reported sensitivity of 96 percent and specificity of 99 percent.35 Plain X-rays are limited by their inability to detect any non-metallic IOFB. Ultrasonography, including high-frequency ultrasound biomicroscopy, can be considered as an adjunctive or alternative method of evaluation for IOFB if there’s low concern for globe rupture.
Surgical Management
Following are the main considerations at the various stages of surgery for IOFBs:
• Surgical timing. Timing of IOFB removal remains controversial and inconsistent, with conflicting results in the literature.25,36–40 The most important factor in timing of IOFB removal is the presence or risk for endophthalmitis. In the presence of endophthalmitis, immediate IOFB removal is recommended at the time of primary globe repair. Organic IOFBs are highly associated with endophthalmitis, while high-velocity projectiles infrequently lead to endophthalmitis, owing to sterility from the heat they generate.37 Multiple other ocular and systemic factors can affect the optimal timing for surgical intervention. Factors related to general health status of the patient, such as the presence of life-threatening injuries and the ability to tolerate surgery, may prohibit operating immediately. Furthermore, in cases where resources aren’t available for concurrent IOFB removal and globe repair, a reasonable alternative is to temporize with primary globe repair and intravitreal antibiotics until the patient is transferred for IOFB removal.25
The location of the IOFB in the posterior segment may also affect timing of removal. There’s an obvious indication for prompt removal if the IOFB was associated with vitreous hemorrhage, retinal break or retinal detachment. In cases without endophthalmitis or vitreoretinal pathology, delaying repair by a few days after primary closure may not adversely affect visual outcomes; however, there remains an increased risk of proliferative vitreoretinopathy development with prolonged exposure to the IOFB. Hence, even in eyes with a low risk of endophthalmitis, there’s been an increasing trend for early vitrectomy within a few days after injury.25,41 Outside of combat scenarios where a majority of IOFBs are sterile, high-velocity projectiles, the composition and sterility of IOFBs are challenging to predict. Therefore in our institution, we prefer to remove the IOFB as soon as possible after the inciting trauma.
• Antibiotic prophylaxis and choice of anesthesia. In all cases, start intravenous antibiotics emergently. Also, because of the high risk of endophthalmitis associated with posterior IOFB, administer intravitreal vancomycin and ceftazidime. Coverage for pathogens typically encountered in IOFB such as staphylococcus, streptococcus, Bacillus, Clostridium and Pseudomonas species is crucial.36 Be sure to obtain cultures, and determine and update the patient’s tetanus status. Traditionally, general anesthesia has been preferred over local anesthesia for open globe injuries primarily to avoid the risk of extrusion of ocular contents due to factors that can increase the transmural and intraocular pressure, such as the volume of the local anesthetic, the instrumentation used for the local anesthesia and potential orbital hemorrhage. However, induction of general anesthesia can also elevate the intraocular pressure, and any bucking or coughing during intubation may elevate the intraocular pressure to a greater extent than local anesthesia. Therefore, local anesthesia with monitored anesthesia care (MAC) is becoming more frequent with IOFB surgery.
• Surgical approaches and considerations. The goals of surgery are to restore ocular integrity, remove the IOFB, address any retinal pathology and treat or prevent endophthalmitis. While no two cases will be alike, planning ahead for the surgical approach and any potentially required instrumentation is key to a safe and successful surgery intraoperatively. The external approach using electromagnets for removal of posterior-segment IOFBs has mostly become obsolete, and pars plana vitrectomy has become the preferred technique. The instrument size for PPV depends on surgeon’s preference, and 23- or 25-gauge are commonly used.
When repairing the entry wound, place the infusion line where you can easily see it. A 6-mm infusion cannula or an anterior-chamber maintainer can be helpful in cases of poor visualization of the infusion cannula due to choroidal detachment, vitreous hemorrhage or lenticular opacity. In cases with small entry wounds, the infusion line can be cautiously opened and closed to maintain intraocular pressure. In larger, irregular wounds, however, we typically restore IOP and anatomy with viscoelastics and wound control before opening the infusion. Corneal wounds are typically closed with 10-0 nylon suture, limbal wounds with 9-0 nylon and scleral wounds with 8-0 nylon. A conjunctival peritomy and exploration may be necessary to determine the extent of the laceration. Care must be taken to prevent extrusion of intraocular structures during open globe repair. At this point, you can place an encircling scleral buckle in cases of concurrent retinal detachment, or can consider placing one as prophylaxis against retinal detachment or PVR.
Next, address any media opacity in the anterior segment due to the injury. Wash out hyphema, if present. In the case of traumatic cataract, perform phacoemulsification or pars plana lensectomy, either with the vitrector for soft lenses (as is the case in many young IOFB patients) or with the fragmatome. Often, the patient may be left aphakic with plans for a staged secondary intraocular lens placement.38
When proceeding to vitrectomy for IOFB removal, consider the need for the optimal placement of additional sclerotomies for the fragmatome or for IOFB removal. Perform a complete vitrectomy with induction of posterior vitreous detachment, if necessary. Use triamcinolone to visualize the vitreous, if needed. Free the IOFB from vitreous traction, and shave the vitreous base. Remove any membranes or scar tissue overlying the IOFB. Then, depending on the size and shape of the IOFB, fashion the route of removal; this may be an existing sclerotomy, a separate pars plana sclerotomy or a scleral tunnel in aphakic eyes. Using the initial entry wound is typically not an ideal exit strategy. Instead, it’s preferable to create a separate exit wound that’s usually larger than what would appear to be required for the size of the IOFB. A common point of failure in IOFB removal is making too small an exit wound. In these cases, the IOFB may become dislodged from the forceps and fall back upon the retina, causing further damage. You can preplace sutures around sclerotomies to augment rapid closure of the wound immediately after the removal of IOFB.
It’s worth considering the use of perfluorocarbon liquid to protect the macula from slippage and dropping of the IOFB or to allow the IOFB to float anteriorly. This strategy may be helpful with non-metallic IOFBs; however, metallic IOFBs are typically denser than perfluorocarbon liquid and usually don’t float. PFCL shouldn’t be used in these circumstances.
A variety of instrumentation is available to grasp and remove an IOFB, depending on its size, shape and ferromagnetic properties. You can use a magnet to lift the IOFB from the retinal surface, but this usually requires passing the IOFB in a handshake maneuver to forceps in order to grasp it more securely. The straight diamond-dusted forceps are the most widely available and, hence, most commonly used forceps. The Wilson, Machemer, Rappazzo and basket forceps are also useful instruments, but aren’t widely available. For irregularly-shaped IOFBs that may not be easily grasped with forceps, consider using a lasso device, such as the FlexLoop, or one fashioned from Prolene suture threaded as a loop through a cannula. Whatever the tool used to remove the IOFB, the goal should be to remove the IOFB successfully on the first attempt.
Once the IOFB is removed, suture the exit wound immediately and perform a careful peripheral retinal exam, particularly in the sector of removal. Secure any retinal defect at the site of the IOFB embedment with laser retinopexy, which may also be performed prior to removal of the foreign body. If the IOFB has impacted deeper tissues, i.e. the retinal pigment epithelium/choroid, a retinochoroidectomy may be performed to limit scarring and PVR. Depending on the number and location of any retinal breaks and the risk for PVR, you can pursue tamponade with gas or silicone oil. At the end of the case, antimicrobial prophylaxis with intravitreal vancomycin, ceftazidime and amphotericin (especially in cases of organic matter) is recommended.
Postoperative follow-up is focused on monitoring for sequelae of posterior segment IOFB including endophthalmitis, retinal detachment and PVR. With demonstrated stability, further visual rehabilitation with silicone oil removal, secondary lens implantation and refraction can be considered.
 |
Outcomes and Prevention
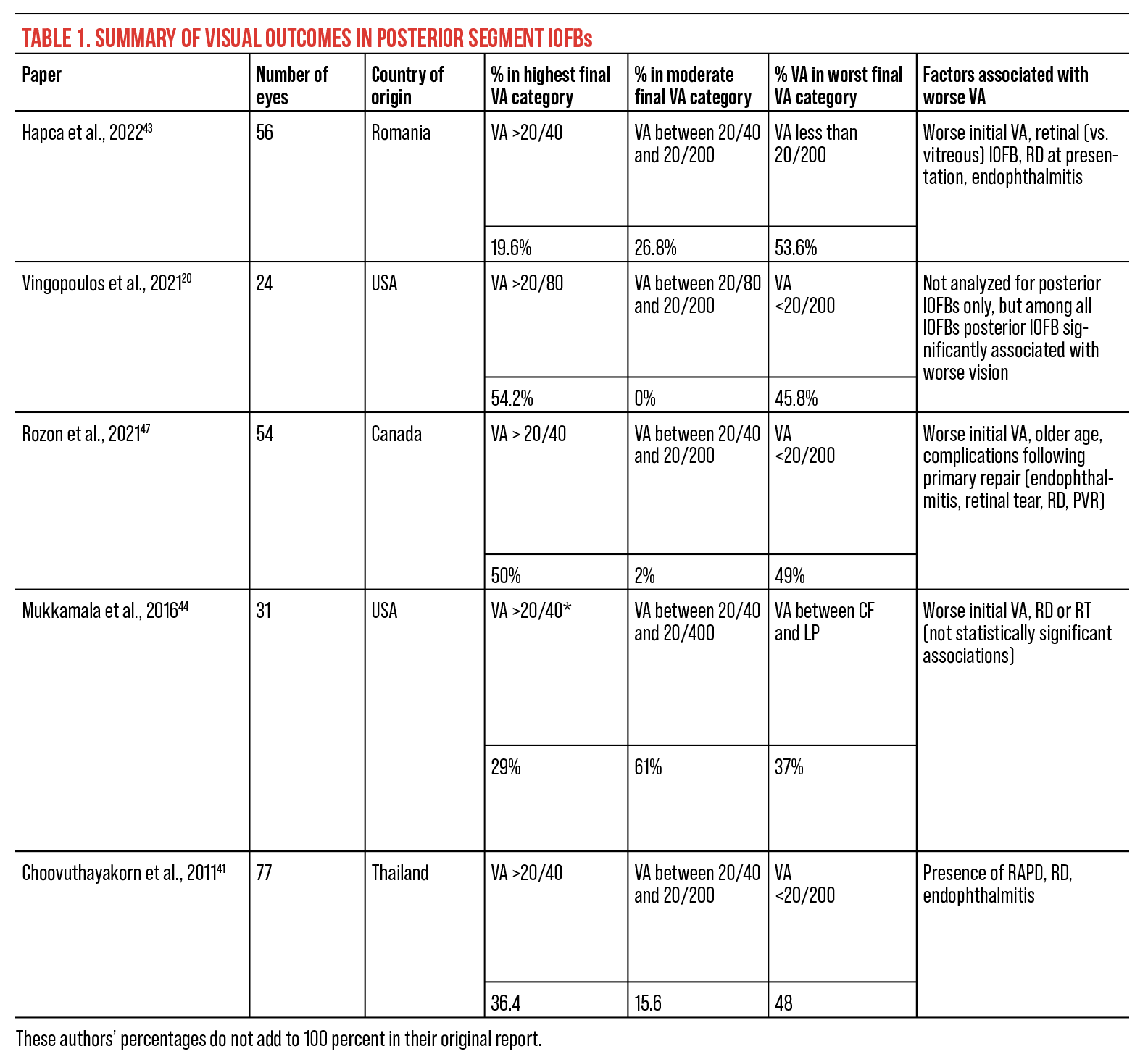
Among all patients with IOFB, posterior IOFB is significantly associated with higher risk of endophthalmitis, higher rate of RD and reduced final VA as compared to anterior segment IOFB.20,42 Among those with posterior IOFB, the most consistent factor predictive of functional final VA is presenting VA.3,4,12,19,20,26,43,44 In posterior IOFB, larger IOFB size is also associated with worse final visual outcome, possibly because a more massive IOFB has higher kinetic energy as it enters the eye and is more likely to cause retinal injury.45 Unsurprisingly, the presence of relative afferent pupillary defect, endophthalmitis, RD or PVR concomitant with IOFB or following primary posterior IOFB removal are associated with worse final visual outcome.12,41,46,47 Table 1 summarizes recent case series of posterior segment IOFBs and final visual outcomes, as well as factors associated with worse final visual outcomes.
Given the significant morbidity associated with IOFBs, the best way to improve outcomes is actually to prevent and/or reduce the incidence of such injuries. The development of policies such as those mandated by the Occupational Safety and Health Administration in the United States or the UK Health and Safety at Work Act were important initial interventions to increase the availability of protective eye equipment for workers; however, despite these policy changes in the 20th century, the incidence of IOFBs has increased, and many injured patients still report not using protection.16,17,48 This suggests that additional education and prevention should be emphasized on both a regional and institutional level. Several studies have evaluated potential educational approaches with mixed results; approaches included the distribution of educational brochures, personal safety glass fittings, group meetings and both positive reinforcement and discipline.49–51
Ophthalmologists, optometrists and emergency medicine providers who often treat these patients also play a significant role in the prevention of injury, both through education and the prescription of polycarbonate glasses in high-risk patients.16 Notably, behavioral studies demonstrated that a prior history of occupational eye injury drastically increased the use of full-time eye protection from 20 percent to 100 percent, suggesting workers may also be able to educate their peers regarding the necessity of eye protection.52
Besides the prevention of IOFB-associated injury, the improvement of surgical outcomes is contingent upon the early recognition and treatment of IOFBs, which typically involves a multidisciplinary team consisting of ophthalmologists, optometrists, emergency room personnel and primary care providers. Education of non-ophthalmic personnel by the ophthalmology community can increase awareness of concerning signs and symptoms and ultimately reduce time to appropriate care.53 Finally, the training of the next generation of ophthalmic surgeons, as well as refinement of surgical techniques and technology, remain crucial to increase the availability and success of surgical care.
In conclusion, posterior IOFB is an ophthalmic emergency requiring urgent evaluation, early diagnosis and timely vitreoretinal intervention. CT imaging of the orbits is the most sensitive and specific imaging modality for identifying posterior IOFB. Initial intervention should include administration of intravitreal and systemic antimicrobial prophylaxis, including tetanus vaccination. When available, most vitreoretinal specialists now favor early PPV with removal of posterior IOFB, as this is likely associated with lower rates of endophthalmitis and PVR.
Outcomes after posterior IOFB are highly variable. Better presenting visual acuity, a smaller IOFB, lack of retinal detachment or injury, and lack of endophthalmitis are predictive of better final visual outcome.
The vast majority of posterior IOFB injuries, as well as OGIs, result from work-related or combat-related injuries among young men. Education of the public, as well as individuals at high risk of IOFB, and encouragement to enact worker eye safety protocols may reduce the incidence of IOFB.
Chloe Y Li, MD, MA, and Jin Kyun (Luke) Oh, MD are ophthalmology residents at Columbia University Medical Center.
Jennifer Adeghate, MD, and Ahmet Hondur, MD, are fellows in vitreoretinal surgery at Columbia University Medical Center.
Royce W.S. Chen, MD, is an associate professor of ophthalmology at Columbia University Medical Center.
1. S. Bureau of Labor Statistics. Survey of occupational injuries and illnesses data. In: U.S. Bureau of Labor Statistics; 2020.
2. Forrest KYZ, Cali JM. Epidemiology of lifetime work-related eye injuries in the U.S. population associated with one or more lost days of work. Ophthalmic Epidemiology 2009;16:3:156-162.
3. Greven CM, Engelbrecht NE, Slusher MM, Nagy SS. Intraocular foreign bodies. Ophthalmology 2000;107:3:608-612.
4. Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Ho AC, Regillo CD. Metallic intraocular foreign bodies: Characteristics, interventions, and prognostic factors for visual outcome and globe survival. American Journal of Ophthalmology 2008;146:3:427-433.e2.
5. Liu CCH, Tong JMK, Li PSH, Li KKW. Epidemiology and clinical outcome of intraocular foreign bodies in Hong Kong: A 13-year review. Int Ophthalmol 2017;37:1:55-61.
6. Armstrong MFJ. A review of intraocular foreign body injuries and complications in N. Ireland from 1978-1986. Int Ophthalmol 1988;12:2:113-117.
7. Bourke L, Bourke E, Cullinane A, O’Connell E, Idrees Z. Clinical outcomes and epidemiology of intraocular foreign body injuries in Cork University Hospital, Ireland: An 11-year review. Ir J Med Sci 2021;190:3:1225-1230.
8. Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Survey of Ophthalmology 2016;61:5:582-596.
9. O’Duffy D, Salmon JF. Siderosis bulbi resulting from an intralenticular foreign body. American Journal of Ophthalmology 1999;127:2:218-219.
10. Rao NA. Chalcosis in the human eye: A clinicopathologic study. Arch Ophthalmol 1976;94:8:1379.
11. Bhagat N, Nagori S, Zarbin M. Post-traumatic infectious endophthalmitis. Survey of Ophthalmology 2011;56:3:214-251.
12. Jonas JB, Knorr HLJ, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology 2000;107:5:823-828.
13. Kuhn F, Pieramici D. Intraocular foreign bodies. In: Ocular Trauma: Principles and Practice. New York: Thieme, 2002:235-263.
14. Potts AM, Distler JA. Shape factor in the penetration of intraocular foreign bodies. American Journal of Ophthalmology 1985;100:1:183-187.
15. Lit ES, Young LHY. Anterior and posterior segment intraocular foreign bodies. International Ophthalmology Clinics 2002;42:3:107-120.
16. Jin G, Zou M, Zhang Y, et al. Time trends, associations and global burden of intraocular foreign bodies. Br J Ophthalmol 2022;106:3:435-439.
17. Yuan M, Lu Q. Trends and disparities in the incidence of intraocular foreign bodies 1990–2019: A global analysis. Front Public Health 2022;10:858455.
18. Imrie FR, Cox A, Foot B, MacEwen CJ. Surveillance of intraocular foreign bodies in the UK. Eye 2008;22:9:1141-1147.
19. Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in China: Clinical characteristics, prognostic factors, and visual outcomes in 1421 eyes. American Journal of Ophthalmology 2011;152:1:66-73.e1.
20. Vingopoulos F, Wang Y, Grob S, et al. Open-globe injury with intraocular foreign body. Journal of VitreoRetinal Diseases 2021;5:4:288-294.
21. Jung HC, Lee SY, Yoon CK, Park UC, Heo JW, Lee EK. Intraocular foreign body: Diagnostic protocols and treatment strategies in ocular trauma patients. JCM 2021;10:9:1861.
22. Parke DW, Flynn HW, Fisher YL. Management of intraocular foreign bodies: A clinical flight plan. Canadian Journal of Ophthalmology 2013;48:1:8-12.
23. Blanch RJ, Bishop J, Javidi H, Murray PI. Effect of time to primary repair on final visual outcome after open globe injury. Br J Ophthalmol 2019;103:10:1491-1494.
24. Zhang Y, Zhang MN, Jiang CH, Yao Y, Zhang K. Endophthalmitis following open globe injury. British Journal of Ophthalmology 2010;94:1:111-114.
25. Keil JM, Zhao PY, Durrani AF, et al. Endophthalmitis, visual outcomes, and management strategies in eyes with intraocular foreign bodies. Clin Ophthalmol 2022;16:1401-1411.
26. Gopal L, Banker AS, Deb N, et al. Management of glass intraocular foreign bodies. Retina 1998;18:3:213-220.
27. Upshaw JE, Brenkert TE, Losek JD. Ocular foreign bodies in children. Pediatric Emergency Care 2008;24:6:409-414.
28. Yonekawa Y, Qian CX, Patel AV, Kim LA, Eliott D. Occult perforating globe injury caused by intraocular foreign body. Ophthalmic Surg Lasers Imaging Retina 2016;47:12:1162-1163.
29. Kaushik S, Ichhpujani P, Ramasubramanian A, Pandav SS. Occult intraocular foreign body: Ultrasound biomicroscopy holds the key. Int Ophthalmol 2008;28:1:71-73.
30. Casini G, Sartini F, Loiudice P, Benini G, Menchini M. Ocular siderosis: A misdiagnosed cause of visual loss due to ferrous intraocular foreign bodies—epidemiology, pathogenesis, clinical signs, imaging and available treatment options. Doc Ophthalmol 2021;142:2:133-152.
31. Nicoară SD, Irimescu I, Călinici T, Cristian C. Outcome and prognostic factors for traumatic endophthalmitis over a 5-Year period. Journal of Ophthalmology 2014;2014:1-7.
32. Zhou Y, DiSclafani M, Jeang L, Shah AA. Open globe injuries: Review of evaluation, management, and surgical pearls. Ophthalmology 2022;16:2545-2559.
33. Tate E, Cupples H. Detection of orbital foreign bodies with computed tomography: Current limits. American Journal of Roentgenology 1981;137:3:493-495.
34. Modjtahedi BS, Rong A, Bobinski M, McGahan J, Morse LS. Imaging characteristics of intraocular foreign bodies: A comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina 2015;35:1:95-104.
35. Saeed A, Cassidy L, Malone DE, Beatty S. Plain X-ray and computed tomography of the orbit in cases and suspected cases of intraocular foreign body. Eye 2008;22:11:1373-1377.
36. Ahmed Y, Schimel AM, Pathengay A, Colyer MH, Flynn HW. Endophthalmitis following open-globe injuries. Eye 2012;26:2:212-217.
37. Colyer MH, Weber ED, Weichel ED, et al. Delayed intraocular foreign body removal without endophthalmitis during operations Iraqi Freedom and Enduring Freedom. Ophthalmology 2007;114:8:1439-1447.
38. Jabłoński M, Winiarczyk M, Biela K, et al. Open globe injury (OGI) with a presence of an intraocular foreign body (IOFB)—Epidemiology, management, and risk factors in long term follow-up. JCM 2022;12:1:190.
39. Liu Y, Wang S, Li Y, Gong Q, Su G, Zhao J. Intraocular foreign bodies: Clinical characteristics and prognostic factors influencing visual outcome and globe survival in 373 eyes. Journal of Ophthalmology 2019;2019:1-7.
40. Anguita R, Moya R, Saez V, et al. Clinical presentations and surgical outcomes of intraocular foreign body presenting to an ocular trauma unit. Graefes Arch Clin Exp Ophthalmol 2021;259:1:263-268.
41. Choovuthayakorn J, Hansapinyo L, Ittipunkul N, Patikulsila D, Kunavisarut P. Predictive factors and outcomes of posterior segment intraocular foreign bodies. Eye 2011;25:12:1622-1626.
42. Liang Y, Liang S, Liu X, Liu D, Duan J. Intraocular foreign bodies: Clinical characteristics and factors affecting visual outcome. Journal of Ophthalmology 2021;2021:1-9.
43. Hapca MC, Muntean GA, Drăgan IAN, Vesa Ștefan C, Nicoară SD. Outcomes and prognostic factors following pars plana vitrectomy for intraocular foreign bodies—11-Year retrospective analysis in a tertiary care center. JCM 2022;11:15:4482.
44. Mukkamala LK, Soni N, Zarbin MA, Langer PD, Bhagat N. Posterior segment intraocular foreign bodies: A 10-Year review. Ophthalmology Retina 2017;1:4:272-277.
45. Woodcock MGL, Scott RAH, Huntbach J, Kirkby GR. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology 2006;113:12:2262-2269.
46. Szijártó Z, Gaál V, Kovács B, Kuhn F. Prognosis of penetrating eye injuries with posterior segment intraocular foreign body. Graefes Arch Clin Exp Ophthalmol 2007;246:1:161-165.
47. Rozon JP, Lavertu G, Hébert M, et al. Clinical characteristics and prognostic factors of posterior segment intraocular foreign body: Canadian experience from a tertiary university hospital in Quebec. Journal of Ophthalmology 2021;2021:1-7.
48. U.S. Dept. of Labor, Occupational Safety and Health Administration. Occupational Health OSHA Technical Manual. For sale by the Superintendent of Documents, U.S. Government Printing Office; 1990.
49. Lipscomb HJ. Effectiveness of interventions to prevent work-related eye injuries. American Journal of Preventive Medicine 2000;18:4:27-32.
50. Mancini G. Prevention of work related eye injuries: Long term assessment of the effectiveness of a multicomponent intervention among metal workers. Occupational and Environmental Medicine 2005;62:12:830-835.
51. Shah A, Blackhall K, Ker K, Patel D. Educational interventions for the prevention of eye injuries. Cochrane Injuries Group, ed. Cochrane Database of Systematic Reviews. Published online October 7, 2009. doi:10.1002/14651858.CD006527.pub3
52. Blackburn JL, Levitan EB, MacLennan PA, Owsley C, McGwin G. Changes in eye protection behavior following an occupational eye injury. Workplace Health Saf 2012;60:9:393-400.
53. Gupta A, Tripathy K. Intraocular foreign body. In: StatPearls. StatPearls Publishing; 2023. [online publication] Accessed March 21, 2023. http://www.ncbi.nlm.nih.gov/books/NBK576415/.




