A randomized, single-blind noninferiority clinical trial, PERCEPOLIS, aimed to determine whether subluxation supracapsular phacoemulsification techniques were inferior to a reference endocapsular (divide-and-conquer) technique regarding postoperative corneal endothelial cell loss.
Patients (ages 18 years or older) with greater than +0.2 logMAR best spectacle-corrected visual acuity, and normal-to-severe density cataract were randomized to subluxation or divide-and-conquer phacoemulsification in 2015 and 2016. Follow-up with ophthalmic tests was conducted on day four; and months one, three and 12. The primary study outcome was ECL at all time points. Secondary study endpoints were operative variables, including effective phaco time and procedure duration. A clinically relevant noninferiority ECL limit was established based on the literature. Here are some of the findings:
- In total, 292 patients (mean age, 73 years; 59 percent female) were randomized and underwent subluxation (n=148) or divide-and-conquer (n=144).
- Day four, and months one, three and 12 data were available for 243, 270, 275 and 198 patients, respectively.
- The unexpectedly high dropout at 12 months meant that the 12-month ECL data could only be assessed qualitatively.
- Surgery was successful in all patients.
- Subluxation was noninferior to divide-and-conquer in ECL.
- Effective phaco times were similar, but subluxation was associated with shorter procedure duration.
Scientists found the subluxation technique was noninferior to divide-and-conquer regarding postoperative ECL, at least in the first three months, and was associated with reduced intervention time. They added that subluxation techniques may be suitable alternatives to endocapsular techniques.
Cornea 2021; Nov 3. [Epub ahead of print]
Perone JM, Ghetemme C, Zevering Y, et al.
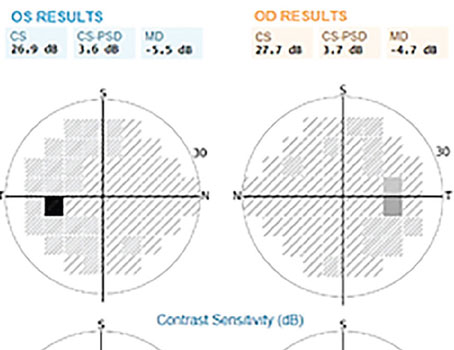
Symptoms Associated with VF Damage in Glaucoma
Researchers studied which patient-reported symptoms best distinguished patients with and without glaucoma, and which explained the most variance in visual field damage. They also compared the amount of variance that can be explained by symptoms vs. retinal nerve fiber layer thickness, as part of a cross-sectional study. Participants included adults diagnosed with glaucoma or suspicion of glaucoma (controls).
Worse-eye VF damage was defined by perimetric testing; RNFL thickness was defined by OCT imaging. Patients rated their visual symptoms on questions collated from several published questionnaires, rating the frequency and severity of 28 symptoms on a scale of one (never/not at all) to four (very often/severe). Multivariable regression models identified patient-reported symptoms that were associated with the highest variance in VF damage.
Main outcome measures included patient-reported symptoms that explained the most variance in VF damage and RNFL thickness.
A total of 170 patients (mean age=64; 58 percent female; 47 percent employed) completed testing, including 95 glaucoma suspects and 75 glaucoma patients. Here are some of the findings:
- In glaucoma patients, median mean deviation of VF damage in the worse eye was -19.3, and ranged from -5.3 to -34.7 dB.
- Symptoms more common among glaucoma patients compared to glaucoma suspects included:
- better vision in one eye;
- blurry vision, glare;
- sensitivity to light;
- cloudy vision; and
- little peripheral vision.
- Worse severity ratings for the symptom “little peripheral vision” explained the most variance in VF damage (43 percent).
- A multivariable model including the frequency of cloudy vision, severity of having little peripheral vision, missing patches of vision, one eye having better vision and vision worsening, plus sociodemographic features, explained 62 percent of the variance in VF damage.
- Comparatively, a multivariable model of worse-eye RNFL thickness and sociodemographic features explained 42 percent of the variance in VF damage, while a model including only sociodemographic features explained 8 percent of the variance in VF damage.
Researchers found that five patient-reported symptoms explained a significant amount of the variance in VF damage. They suggested that asking patients about their symptoms may optimize patient-physician communication and be a useful adjunct to clinical testing in some patients to estimate disease severity.
Ophthalmology 2021; Oct 27. [Epub ahead of print]
Shah YS, Cheng M, Mihailovic A, MS, et al.
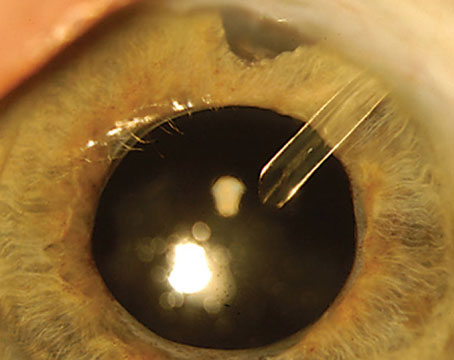
Trapezoid vs. Conventional 2.2-mm Clear Corneal Incisions
Scientists compared the incidence of incision-related Descemet’s membrane detachment among eyes undergoing modified vs. conventional 2.2-mm incision phacoemulsification for hard nuclear age-related cataract.
The double-masked, parallel randomized clinical trial was conducted from July 22, 2019, to January 22, 2020, at Zhongshan Ophthalmic Center, Sun Yat-sen University in Guangzhou, China. The study included patients with age-related cataract and nuclear opalescence grade of 4.0 or greater based on the Lens Opacities Classification System III. Patients were enrolled in this study according to the following inclusion criteria: age between 65 to 90 years; pupil size of 6 mm or greater after dilation; Lens Opacities Classification System III nuclear opalescence grade of 4.0 or more; and corneal endothelial cell density greater than 1,500 cells/mm2.
Main outcomes and measures included incidence of incision-related DMD at postoperative day 1.
A total of 130 eyes of 130 patients were randomized into the conventional group (n=65) or the modified group (n=65). The mean age of participants was 74.5 ±5.9 years and 74.3 ±6 years in the conventional and modified groups, respectively. A total of 26 participants in the conventional group (40 percent) and 27 in the modified group (42 percent) were men. Here are some of the findings:
- Compared with eyes in the conventional group, the incidence of DMD in eyes in the modified group was significantly lower at postoperative day one (difference, 26.15; CI, 9.60 to 42.71; p=0.003).
- The difference at postoperative day seven was 16.92 (CI, 2.91 to 30.94; p=0.02).
- The length of DMD (postoperative day one: difference, 0.188; CI, 0.075 to 0.301; p=0.002) and maximal corneal thickness at incision site (postoperative day 1: difference, 0.032; CI, 0.006-0.057; p=0.02; postoperative day 7: difference, 0.019; CI, 0.003 to 0.035; p=0.02) were lower in the modified group, while visual quality parameter modulation transfer function (postoperative day one: difference, -0.033; CI, -0.064 to -0.001; p=0.04) was higher.
- No difference was observed between the two groups in best-corrected visual acuity, central corneal endothelium loss or surgically induced astigmatism at any follow-up time.
- No intraoperative complications were reported in either group.
Scientists wrote that the findings suggested that modified 2.2-mm trapezoid incision phacoemulsification reduced the incidence of DMD for hard nuclear age-related cataract at postoperative day one and might be considered in patients at high risk of incision-related DMD, although they added that the clinical relevance couldn’t be determined with certainty from this trial.
JAMA Ophthalmol 2021; Oct 14. [Epub ahead of print]
Dai Y, Liu Z, Wang W, et al.
Vascular Issues and Low-tension Glaucoma
Researchers from the Mayo Clinic Department of Ophthalmology undertook a retrospective, case-control study designed to identify patients seen at the clinic between 2005 and 2015 with low-tension glaucoma, and an age- and sex-matched control group, each containing 277 patients.
The low-tension glaucoma group had more myopic refractive errors in diopters (-1.6 vs. -1.0, p<0.001), lower intraocular pressure (14.2 vs. 15.2 mmHg, p<0.001), and a higher cup-to-disc ratio (0.7 vs. 0.3, p<0.001).
The low-tension glaucoma group was significantly less likely to be obese (BMI >30, p=0.03). They had a significantly higher prevalence of systemic hypertension (OR: 1.64, p=0.004), diabetes mellitus (OR 3.01, p≤0.001), peripheral vascular disease (OR 2.61, p=0.009), migraine headache (OR 2.12, p=0.02), anemia (OR 2.18, p=0.003), systemic hypotension (OR 4.43, p≤0.001), Raynaud’s Syndrome (OR 3.09, p=0.05), angiotensin converting enzyme inhibitor (OR 1.64, p=0.01), and calcium channel blocker use (OR 1.98, p=0.004).
After adjusting for systemic hypertension, calcium channel blocker use remained significant (OR 1.70, p=0.03). No significant difference was found with respect to hyperlipidemia, obstructive sleep apnea, coronary artery disease, carotid stenosis, stroke, or use of statins, ACE inhibitors, angiotensin receptor blockers, beta blockers or metformin.
Multiple vascular-associated conditions were associated with low-tension glaucoma, including systemic hypertension, diabetes mellitus, peripheral vascular disease, migraine headaches, Raynaud’s Syndrome, anemia, systemic hypotension, and calcium channel blocker use. The researchers say that this study strengthens evidence for the vascular hypothesis of low-tension glaucoma.
Journal of Glaucoma; Nov. 03. [Epub ahead of print]
Funk RO, Hodge DO, Kohli D, et al.