Pseudoexfoliation has long been known to be a concern when performing cataract surgery. The likelihood of a problematic iris, weakened zonules, postop glaucoma and serious problems occurring years later are issues a cataract surgeon needs to address before, during and after surgery.
Here, surgeons share their experience and advice for making sure these patients have the best outcomes possible.
The Warning Signs
Although surgeons agree that it’s possible to be surprised by the presence of pseudoexfoliation when you get to the operating room, most cases can be discovered by noting warning signs during the preop exam.
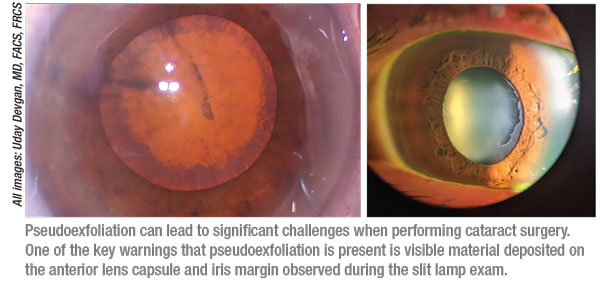
• Look for material on the lens capsule and iris. “An eye that has pseudoexfoliation will usually present with pseudoexfoliation material on the pupil margin and the anterior lens capsule that’s visible during the slit lamp exam,” notes Uday Devgan, MD, FACS, FRCS, chief of ophthalmology at Olive View UCLA Medical Center, an associate clinical professor at the UCLA School of Medicine, and in private practice at Devgan Eye Surgery in Los Angeles.
Amy D. Zhang, MD, a clinical assistant professor of ophthalmology at the Kellogg Eye Center, University of Michigan in Ann Arbor, notes that this material isn’t always obvious. “The edges of the iris may have a white fibrillary appearance,” she says. “This is most prominently seen at the pupillary border. These can be subtle indications that may be missed on a cursory exam.”
• Check to see whether the other eye has had zonular issues in the past. “If the other eye has already had surgery and there was a problem, my guard will be up,” says JoAnn Giaconi, MD, a clinical professor of ophthalmology at the Jules Stein Eye Institute and chief of ophthalmology at the Veterans Administration in Los Angeles.
 |
• Note the extent of pupil dilation. “Pseudoexfoliation patients don’t dilate as well as other patients do,” notes Dr. Devgan. “Notably, it turns out that the ones who are dilating more poorly tend to have weaker zonular support during surgery, while the pseudoexfoliation patients who dilate better tend to have somewhat better zonular support.”
• Be alert for a relatively shallow anterior chamber. “Another clue, which is a little more subtle, is the anterior chamber depth relative to the axial length,” Dr. Devgan points out. “An average eye with an average axial length should also have an average anterior chamber depth. If you have an average axial length but a very shallow, crowded anterior chamber, that means that the entire zonular support is so weak that the cataract and the iris are being pushed forward into the anterior chamber.”
“An anterior chamber depth of less than 2.5 mm has been associated with four-fold increased risk of zonular instability and/or vitreous loss,” notes Dr. Zhang. “Also, compare the anterior chamber depth to that of the fellow eye. Pseudoexfoliation may be unilateral, so a difference between the eyes could indicate a problem.”
“The other part of this,” adds Dr. Devgan, “is that when you get to the OR and the patient lies down, gravity will pull the bag and iris back and the anterior chamber will become really deep. That’s because the zonules are so loose that the lens moves forward and back.”
• Watch for iridodonesis when the eye moves during the slit lamp exam. Dr. Giaconi notes that this is another sign of loose zonules.
• Look for elevated IOP and optic nerve damage. “In many cases of pseudoexfoliation, glaucoma or ocular hypertension are present,” Dr. Zhang points out. “So, noticing whether there’s an elevation in IOP or signs of optic nerve damage is important.”
• Consider performing gonioscopy. “Not everyone does this, but if you do, check the angle for fibrillary deposits,” advises Dr. Zhang. “As a glaucoma specialist, I do this routinely.”
Preparing for Trouble
Once you’ve determined that pseudoexfoliation is present, these strategies can help ensure successful cataract surgery:
• Let the patient know that the surgery has a slightly higher risk because of the pseudoexfoliation. “I do spend a little time explaining this to the patient, but I’m careful not to dissuade the patient from having cataract surgery,” says Dr. Zhang. “You don’t want to have to explain the impact of pseudoexfoliation to a skeptical patient after something has gone wrong. Even if a patient already knows that they have pseudoexfoliation, they may not realize that it could impact their cataract surgery.”
• If pseudoexfoliation is present, consider implanting an anterior chamber lens, and plan accordingly. “If the eye has pseudoexfoliation and the patient is older and the lens is denser, I’ll plan for the possible use of an anterior chamber lens,” Dr. Giaconi explains. “Because these lenses aren’t used that often today, our OR doesn’t stock all of the options. So, I’ll measure the white-to-white distance and calculate the power, and ask the OR to pre-order the appropriate lens so it’s available if needed.”
• Make sure pupil expansion tools will be available in the OR. “I make sure we’ll have an iris expansion ring on hand, and iris hooks,” says Dr. Giaconi. “That way the nurses won’t have to go searching for things in the middle of surgery.”
• Make sure you’re comfortable performing an anterior vitrectomy and are prepared to do so. “When the patient has pseudoexfoliation, a vitrectomy may be necessary,” notes Dr. Zhang. “The incidence of vitreous loss tends to be higher, especially in those patients that have much narrower anterior chambers.”
Dr. Giaconi agrees. “Surgeons are often surprised by vitreous in these patients,” she says. “You always need to have vitrectomy equipment on hand.”
• If you think the lens may need to be sutured in, consider referring the patient to someone with extensive experience doing that. “I prefer not to suture IOLs in place, even if the lens is obviously loose preoperatively,” says Dr. Giaconi. “I only suture a lens once or twice a year, so it may not be in the patient’s best interest for me to spend an extra hour and a half doing that. Some high-volume cataract surgeons do this fairly often. If I know of a surgeon who can do it quickly, safely and efficiently, I’ll simply refer the patient to that individual.”
Surprise PXF in Surgery
 |
Although it’s not good to be surprised by pseudoexfoliation in the OR, it can happen. Dr. Devgan notes that it’s sometimes easier to see pseudoexfoliation on the operating table than it is to see it in the clinic. “The patient may not be as dilated in the exam room as in the OR,” he notes. “The strength of the dilating drops is very different. Also, when I shine a bright light in the patient’s eye in the clinic, many patients become squeamish, so it’s harder to evaluate. In the OR the patient has sedation on board, so you can shine that bright microscope light in their eye and they’re very cooperative. As a result, you may see pseudoexfoliation signs on the table that you missed during the exam.”
One sign that unexpected pseudoexfoliation is present is a change in anterior chamber depth when the patient is lying down. “Most surgeons won’t compare the anterior chamber depth with the patient sitting up vs. lying down during the preop exam,” notes Dr. Giaconi. “Often the first time you see the patient in a reclined position is in the OR. If you realize the anterior chamber is deeper when the patient is on the table, you know the patient has zonulopathy and you’ll need to proceed with caution.”
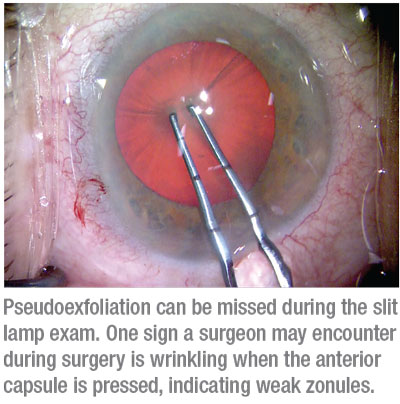
Another sign is that the anterior capsule wrinkles when pressed. “Suppose the pupil dilation is acceptable, so you start the capsulorhexis,” Dr. Devgan says. “If pseudoexfoliation is present, when you poke into the anterior capsule to begin your capsulorhexis, you may notice a lot of radial wrinkles. That tells you right away that you’re dealing with loose zonules. In a healthy eye, the anterior capsule is like a trampoline with strong springs; it will be flat and taut, and if you push on it, it will be springy. But if the springs of the trampoline are very loose, poking on the surface causes wrinkles.”
Dr. Zhang notes that in terms of surprises, the most common may be a case in which the pupil starts out big on the table but suddenly becomes small. “That leaves you wondering whether you’re dealing with pseudoexfoliation,” she says. “In that situation, if you weren’t prepared to deal with pseudoexfoliation, you have to take each step more slowly. Perform the cataract surgery as you would any other case, but be alert for any sign of vitreous prolapse and zonular laxity. The chance of vitreous loss will be higher in those patients.”
Managing a Small Pupil
Because a common effect of pseudoexfoliation is a pupil that fails to expand sufficiently, the surgeon has to decide how to compensate. Many surgeons choose to enlarge the iris with iris hooks, a device such as the
Malyugin ring, or a pharmaceutical option such as Omidria (phenylephrine and ketorolac, Omeros).
Dr. Giaconi notes that in terms of a mechanical device, both iris hooks and a pupil expander have pros and cons. “Cosmetically, either option can distort the pupil a little bit postop,” she says. “I use the Malyugin ring more often just because it’s quicker, but if you plan to prolapse the nucleus through the capsulorhexis and the iris, the ring can sometimes prevent it from prolapsing through. Iris hooks avoid this problem, and they can do a better job of controlling pupil size and shape, but they take longer to use.”
Dr. Zhang says she’s more inclined to use iris hooks. “If things start dropping, iris hooks are much easier to remove than an entire Malyugin ring,” she points out.
Dr. Devgan says he prefers not to use any device or pharmaceutical at all. “I think most surgeons who’ve done a large volume of cataract surgeries will probably just stretch the pupil to open it up a little further, and then do the capsulorhexis underneath the iris, viewing through the pupil,” he says. “We can create a 5.5-mm capsulorhexis, even if the pupil is only 4.5 mm. We don’t have to visualize the entire edge directly.”
Dr. Devgan adds that he doesn’t think a pupil expander is any safer. “I think it may be more traumatic, and more likely to cause damage to the iris than pupil stretching,” he says. “In one of my online educational videos I did a comparison; I did one eye using a Malyugin ring and did the other using my [no-device] approach. The capsulorhexis was fine in both eyes, but the iris looked better after using my approach.” (You can watch the video at cataractcoach.com/2018/10/31/pupil-stretch-using-capsulorhexis-forceps/)
During the Surgery
These strategies can help the cataract surgery go well and produce a good result:
• Iris hooks can be used for capsule support if capsule hooks are not available. “In cases of pseudoexfoliation you’ll see some areas of zonular laxity,” says Dr. Zhang. “Capsule hooks would be ideal to provide capsular support, but when capsule hooks aren’t available, I’ve used iris hooks. They get the job done, although they’re not approved for that. When you’re using iris hooks for this purpose, aim for a slightly steeper angle, so the pivot of the hook can capture the capsule. The thing that’s great about iris hooks is that you can place them anywhere, and use as many or as few as you like.”
• Make a large capsulorhexis. “When zonular support is weak, pseudoexfoliation patients tend to develop capsular phimosis three, six or even 12 months after surgery,” Dr. Devgan explains. “That causes the anterior capsule rim to shrink and pull toward the center. A 4-mm capsulorhexis may become fibrotic and scar up, shrinking to 2 or 3 mm. This can even dislodge the lens. To prevent that, you want to create at least a 5-mm or 5.5-mm-diameter capsulorhexis. This minimizes the impact of any shrinkage.”
Dr. Giaconi points out a second reason to make a large capsulorhexis. “A small capsulorhexis can make it more difficult to get the lens out of the bag in an already challenging case.”
Dr. Giaconi adds that making paired postop anterior capsular incisions in the capsulorhexis can help with potential phimosis. “This may enlarge the capsulorhexis a little bit and distribute the tension, offsetting contraction from postop phimosis,” she says.
• Consider using a capsular tension ring. Dr. Zhang says she finds these helpful when managing a pseudoexfoliation patient. “That raises two questions,” she notes. “When during the procedure should you insert it? And in which situations is it not likely to be helpful?
“In terms of timing, if you put it in early in the procedure, you’re going to have trouble removing some of the cortex or nuclear material,” she says. “If you still have a lot of nucleus present you’ll have a harder time visualizing where you’re placing it. However, you don’t want to wait until late in the procedure to insert it, when you’ve lost the support of the bag. I usually place it when I’ve removed most of the cortical material.
“I wouldn’t insert a capsular tension ring if there’s more than four clock hours of zonular laxity,” she adds. “A CTR isn’t really designed to support that many clock hours. In that situation you may have to think about other options, such as suturing in an Ahmed segment, or using multiple segments to provide more coverage.”
Dr. Devgan agrees. “I wouldn’t put a CTR in a pseudoexfoliation patient with 360-degree zonular weakness,” he says. “There may not be a benefit there. For those with 360-degree weakness, my preference is getting a three-piece lens, putting the haptics in the sulcus and capturing the optic behind the capsulorhexis so the optic is in the bag. That’s great for long-term stability, and it will prevent any phimosis, because the tissue can’t clamp down on the lens.”
• If the zonulopathy is serious, consider implanting an anterior chamber lens. “In these eyes there’s a pretty good chance the lens will decenter postoperatively,” says Dr. Giaconi. “Putting in a capsular tension ring may delay a problem, but it’s not going to prevent the bag from falling. So, if I find a lot of zonulopathy, I’d probably go ahead and put in an anterior chamber lens.”
• Use a phaco technique that won’t stress the zonules. “For me, that means avoiding a technique like divide-and-conquer and using something like a quick-chop technique instead,” says Dr. Devgan. “An even better option is to bring the nucleus
partially out of the capsulorhexis bag, which eliminates any zonular stress.” (You can watch a video of this technique at cataractcoach.com/2020/03/21/review-pseudo-exfoliation-cataract-surgery/)
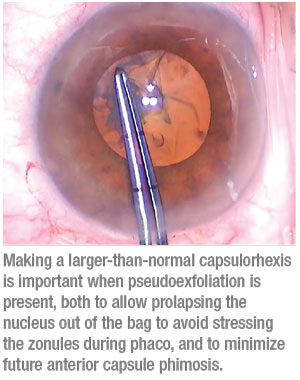 |
Dr. Zhang says she typically uses horizontal chop in these cases. “I also make my rhexis a little larger so I can partially prolapse the lens out of the bag and further chop the nucleus in that manner,” she explains. “My only concern is that sometimes the anterior chamber is very narrow, and if you prolapse the entire lens out, it could cause damage to the endothelium.”
“In reality, different techniques are going to work better in different surgeons’ hands,” notes Dr. Giaconi. “Some surgeons have a very light touch; they may be able to get away with more than other surgeons can.”
Dr. Zhang adds that in pseudoexfoliation cases it’s good to slow everything down to some extent. “We use Alcon’s Centurion system, which lets us set the intraocular pressure we’d like to maintain,” she says. “In addition, I slow down the fluid dynamics compared to a normal cataract surgery, in case vitreous does present itself.”
• Remove excess capsule epithelial cells after phaco—carefully. “When you’ve taken out the cataract and the cortex and you’re cleaning up the capsular bag, you may see some hazy lens cells left on the capsule,” says Dr. Devgan. “Removing those can help prevent phimosis and capsular contraction. Being thorough is important, but you have to balance that with not damaging the capsule, which is already weak. Remember the first rule of medicine: First, do no harm.”
Dr. Giaconi notes that the studies looking at the value of removing these cells have produced mixed results. “Nevertheless, if there’s a lot of material on the anterior capsule, I like to use a tool to scrape the cells away,” she says. “If you use a tool designed for this purpose, I don’t think you’ll have a problem in terms of damaging the capsule.”
• Securing the lens in place has pros and cons. “I don’t routinely scleral-fixate the lens, although I know some of my colleagues do,” says Dr. Zhang. “Normally I wait until a problem has occurred and then fixate the lens. Doing this at the time of the cataract surgery is a lot of extra work to prevent a problem that may or may not occur. It will make the initial surgery take longer and impact patient comfort as well.”
• Remember: If a big problem occurs, you don’t have to solve it that day. “Suppose you’re trying to remove the cortex and the whole capsular bag comes out of the eye,” says Dr. Devgan. “It’s OK to close the eye up and come back in a few days or a month to fixate a lens in the eye. Or, have your colleague who’s really good at it do it later. You don’t have to do it at the same time.”
Postop Management
Pseudoexfoliation patients need to be monitored carefully postop:
• Be proactive about a potential postop pressure spike. “For uncomplicated cases, a drop of dorzolamide-timolol in the OR immediately following surgery has been reported to help with IOP in the first 24 hours,” says Dr. Giaconi. “On the other hand, if the surgery was complicated, and there’s no contraindication, I usually give these patients a dose of Diamox in the OR to try to prevent an overnight spike in pressure. I’ll also prescribe a few tablets to take home. I tell them: ‘If you start to feel a headache coming on, take a tablet.’
“I check these patients the morning after surgery,” she adds. “If their pressure makes me uncomfortable, I’ll adjust their medications and see them a few days later. If their pressure is fine, I might just see them a week later. I’d probably check them weekly for the first month.”
|
“I may bring these patients back a little bit sooner than an average patient to make sure they’re not experiencing a postop pressure spike,” agrees Dr. Zhang. “How soon I bring them back depends on their IOP on day one. If it’s borderline—in the mid-20s or so—I’d probably bring them back in a couple of days to reassess, and I might start them on a topical drop for pressure control.”
• Consider keeping your pseudoexfoliation patient on medications longer. “I often put my pseudoexfoliation patients on steroids and NSAIDs for a longer time than I would a routine cataract patient,” says Dr. Zhang.
Dr. Giaconi adds that she increases postop steroids a little bit if the surgery runs long. “A longer surgery will probably lead to more corneal edema,” she notes.
• Monitor these patients for glaucoma. “The material that weakens the zonules also clogs up the trabecular meshwork,” Dr. Devgan points out. “So, you have to be careful to monitor these patients for signs of glaucoma. Check the IOP; look at the optic nerve; do an OCT of the retinal nerve fiber layer. Stay on the lookout.”
• Dilate these patients at postop visits. “For some other patients you wouldn’t dilate at a routine postop visit,” Dr. Devgan notes. “However, when you’re following-up a pseudoexfoliation patient, you won’t be able to see the anterior chamber rim, or any phimosis, unless you dilate. If you see that the anterior capsule remnant has contracted or is phimotic, you can use the YAG laser in the clinic to make some relaxing incisions, for example at 3, 6, 9 and 12 o’clock. That breaks the phimotic ring so it can’t clamp down.”
• Realize that the lens may have problems down the line no matter what you do. “I think the average number of years these eyes take to develop a decentered lens is six or seven,” says Dr. Giaconi. “Right now I’m not aware of any prospective studies that go out 10 years. However, a recent study conducted at Aravind Eye Hospital in India looked at uncomplicated pseudoexfoliation cases—patients with no zonulopathy where the pupils dilated reasonably well. At five years, it made no difference whether you’d put in a one-piece or three-piece lens, or whether you inserted a CTR.”1
“The reality is that pseudoexfoliation is a progressive disease,” says Dr. Devgan. “You’re not stopping its progression by doing the cataract surgery. In some patients, especially those living to 90 or longer, the entire lens and capsular bag may fall back into the vitreous and float there. If it’s still very close to the iris when you see the patient, you may be able to retrieve it by yourself; then you’ll have to suture the lens in place. If the lens has landed back on the retina, you should call a vitreoretinal colleague.”
A Manageable Problem
Dr. Giaconi points out that pseudoexfoliation during cataract surgery isn’t the problem it once was. “Today’s tools make a difference,” she says. “Pseudoexfoliation isn’t a potential disaster, as long as surgeons know what they’re doing. Our outcomes are better than they were 20 years ago. So take your time, use the right tools, and if a problem is beyond your experience, refer to someone who’s accustomed to dealing with it.” REVIEW
Drs. Giaconi, Zhang and Devgan report no financial ties to any product discussed.
1. Haripriya A, Ramulu PY, Schehlein EM, et al. The Aravind Pseudoexfoliation Study: 5-year postoperative results. The effect of intraocular lens choice and capsular tension rings. Am J Ophthalmol 2020;219:253-260.






