There appears to be a disconnect between the data researchers are gathering about pupil size and how this data is actually put to use by refractive surgeons in the field. Several papers have found no correlation between a patient's preoperative pupil diameter and his risk for qualitative vision complaints such as glare and halos postop. Still, many surgeons take pupils seriously, or counsel certain large-pupil patients more intensely for a variety of reasons ranging from fear of litigation to gut instinct. Here is a look at how several refractive surgeons have let this data change, or not change, the way they deal with patients.
Where the Pupil Fits In
"I've never excluded a patient with large pupils from refractive surgery," says Steven Schallhorn, MD, a refractive surgeon at the Naval Medical Center in San Diego. He's performed several studies looking into the factors that might predispose a patient toward having night-vision complaints after refractive surgery. "I also don't adjust the ablation-zone diameter based on the pupil size," he says. "The studies we've conducted over the years have shown that the size of the pupil isn't predictive of those who will have symptoms after surgery, so we've never excluded certain patients because of their pupils, and I don't give extra counseling to patients with large pupils about them being at an increased risk, because that's not been borne out by our studies."
In one of Dr. Schallhorn's studies aimed specifically at pupils and LASIK, patients with large pupils had more quality-of-vision problems at the first month visit, but there was no correlation at the six-month visit. The factors that he and his colleagues found to be related to quality-of-vision symptoms included the preop level of myopia, the preop contrast acuity, the postop uncorrected vision and residual cylinder. They found that most of the visual quality variability wasn't explainable by preoperative or clinical outcome measures, including the diameter of the pupils.1
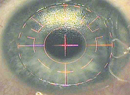
 |
| The higher-order aberration coma can cause postop qualitative vision complaints. Photo: David Hardten, MD. |
In a similar study from Canada, researchers found the risk factors for night-vision complaints after LASIK showed a 2.8-times increase if the initial myopia was greater than 5 D, a 2.5-times increase if the optical zone was 6 mm, and a 2.9-times increase if the postop spherical equivalent was outside ± 0.5 D of emmetropia.2 After regression analysis of six- and 12-month data, the attempted spherical correction and optical zone were the most predictive factors of night-vision complaints, the researchers found. However, they stressed that pupil size at any postop point wasn't statistically predictive of night-vision complaints.
The Research in Practice
Though surgeons acknowledge the mounting scientific evidence that says pupils don't have anything to do with qualitative vision complaints, their instincts tell them there still may be something to pupil size, and these instincts influence the way they treat patients.
"In the beginning days of refractive surgery, people didn't measure pupil size," says Wills Eye corneal specialist Christopher Rapuano. "It was not on the radar. Then patients started experiencing glare and halos, and we thought they were related to pupils, so the pendulum started swinging the other way, and it was almost a situation where surgeons were saying, 'Pupil size is the only factor in glare and halos, and a normal size is 6 or 6.5 mm. If it's above that and you operate on that patient, you're doing malpractice.'
"Now, doctors are absorbing the new data that's out there and saying, 'Well, pupil size isn't the big factor we thought it was.' " He says that whether it's a factor at all is still unclear to him, but that he thinks it probably is. "Whether it's a 1-percent risk, a 25-percent risk or a 50-percent risk, that's unclear," he says. "So, I think what surgeons are saying to all their patients is, 'Look, there are lots of factors that go into causing glare and halos after surgery. Many of these factors we probably don't even know about, but there are some that we do know: High myopia is associated; high astigmatism is associated; and pupil size is associated. So, just to let you know, if you've got high myopia and high astigmatism you're at higher risk for glare and halos. If you've got huge pupils too, you're probably at somewhat higher risk.' "
Minneapolis refractive surgeon David R. Hardten thinks the data is reliable, and that pupil size has little to do with most patient complaints.
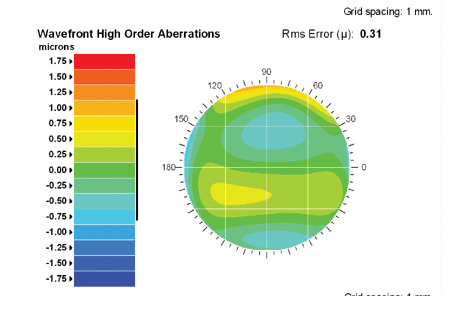
"Probably, pupil size as a sole factor for quality of vision complaints has been, in essence, overplayed," he says. "Most night vision complaints are multifactorial. At least in my practice, anecdotally, symptomatic patients present postop because they have an asymmetric response to the laser that results in significant irregular astigmatism or higher-order aberrations that aren't solely related to pupil size. In fact, I've seen quite a few patients consultatively who have very small pupils yet have qualitative problems."
He says that, when it comes to screening patients preoperatively for the possibility of night vision complaints postop, pupil size is just part of the equation. "I think some other factors are the level of correction, the degree of dryness that they'll experience postop, which can be predicted in some cases, but not always; and whether they'll have an under- or overcorrection." Both Drs. Rapuano and Hardten counsel all patients that they may be at risk for postop glare and halo.
One of the strongest factors influencing surgeons' attitudes toward preop pupil size is the need to practice "defensive medicine," or an informed consent that may protect a surgeon later if he's sued for malpractice by a patient with qualitative vision complaints.
Even Stanford surgeon Edward Manche, who performed his own study of pupil size and found that it wasn't a factor, still emphasizes it with certain patients.
"Even though our study didn't show any correlation, we use pupillometers," he says. "We measure the pupils preoperatively and counsel patients that, if they have larger-than-average pupils, they may be at some risk for glare and halos. We do this for two reasons: First, there's been a lot in the non-peer reviewed press that pupil size matters, and if you don't address pupil size with patients you may find yourself facing expert testimony against you in court. Second, there probably is some effect of pupil size, even though our study and others didn't show it. So, I think you have to warn patients."
Stephen Pascucci, MD, of Wilkes-Barre, Pa., agrees. "I think those surgeons who do a fair amount of surgery still look seriously at pupil diameter as a factor, particularly here in the United States, and in the robust medico-legal environment we practice in," he says. "Even though we may not be speaking as scientists to patients, we're speaking as physicians who are trying to protect ourselves legally to some degree by looking at pupil size. There will be someone, someday who will say in court, 'Your patient's pupils are too large for the procedure, and I wouldn't have operated on him.' "
Dr. Schallhorn hopes that, even if surgeons are speaking to patients about pupil size despite what his and other reports found, that they don't exclusively warn patients with larger pupils.
"What is required is counseling of all patients that they're at risk for quality of vision symptoms and even not being able to drive at night, regardless of whether they have large pupils or not," he asserts. "It's wrong to say that someone with 5-mm pupils isn't at risk, because that patient can have the same level of symptoms as a patient with larger pupils. That's the danger about the emphasis on pupil size, and in practicing defensive medicine: You may be neglecting to adequately counsel patients with small pupils who are at an equal risk for problems."
1. Schallhorn SC, Kaupp SE, Tanzer, DJ, et al. Pupil size and quality of vision after LASIK. Ophthalmology 2003;110:1606-14.
2. Pop M, Payette Y. Risk factors for night vision complaints after LASIK for myopia. Ophthalmology 2004;111:3-10.