 |
 |
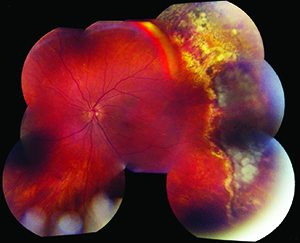
| Figure 1. Following primary retinal detachment repair, this patient initially had a good result (A). Several weeks later, following a decline in vision, a proliferative vitreoretinopathy re-detachment was noted, with membranes seen temporally and inferiorly (B). (See p. 66 for Figures 1C and D.) |
The pathogenesis is far from being completely understood. In general, processes that increase vascular permeability are more likely to increase the probability of PVR formation. Specific risk factors that have been identified include: uveitis; large, giant, or multiple tears; vitreous hemorrhage, preoperative or postoperative choroidal detachments; aphakia; multiple previous surgeries; and large detachments involving greater than two quadrants of the eye.1,2
The PVR process is thought to be analogous to the anomalous wound healing that leads to skin keloid formation.3 It is thought the most important cell types in PVR pathogenesis are the retinal pigment epithelial cells, which are believed to migrate through retinal breaks, de-differentiate and proliferate on the retinal surface. Retinal glial cells and macrophages may also play important roles, perhaps by providing a scaffold for membrane formation and/or by releasing trophic factors.3,4 This process appears to be driven by and modulated by numerous growth factors5 (e.g., platelet-derived growth factor,6 vascular endothelial growth factor,7 tumor growth factor-beta, epidermal growth factor, tumor necrosis factor-alpha and fibroblast growth factor8) and cytokines (e.g., interleukin-1, -6, -8 and -10, and interferon-gamma9). Despite a growing understanding of the molecular underpinnings of PVR, prevention of the clinical phenomenon is still not possible.
Surgery
The mainstay of the management of PVR is surgical, with pars plana vitrectomy with membrane peeling being the primary procedure.
The surgical approach for PVR is generally the same for primary retinal detachments without membranes. The principal difference is that there is significantly more retinal traction in PVR, which is caused by membranes and bands rather than vitreous gel alone. As such, different techniques may be employed to dissect these membranes to allow the retina to flatten.
Additionally, if a scleral buckle was not used at the time of the primary retinal detachment repair, it can be advantageous to place one during the PVR vitrectomy procedure. However, if an extensive inferior retinectomy is likely to be performed, a scleral buckle is likely not needed.
 |  |
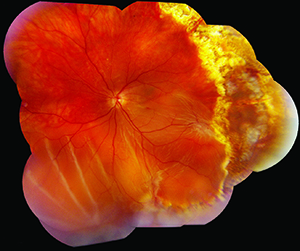
| Figure 1. (See p. 65 for Figures 1A and B.). Immediately following re-operation, the retina is flat under silicone oil tamponade. Note the margins of the retinectomy temporally and inferiorly (C). Several months later the retina is still attached under oil (D). | |
 |  |
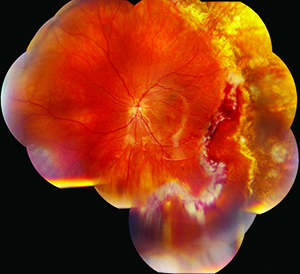
| Figure 2. A typical example of a fixed “star” fold preoperatively (A). Postoperatively, the retina is flat under silicone oil (B). | |
Medical Prevention/Treatment
Significant basic science and animal research effort has been directed towards elucidating the pathobiology of PVR with the aim of preventing retinal re-detachment. Unfortunately few human studies conclusively provide guidance on the optimal means of doing so. Historically, three main categories of pharmacologic prevention have been explored: anti-inflammatory; anti-proliferative/neoplastic; and anti-growth factor.9
Corticosteroids were among the first agents tested in the prevention of PVR. The rationale for their utility stems from the observation that PVR seems to be an inflammatory event clinically, and this has been validated with proteomic analysis.12 Their effectiveness was suggested in animal experiments,13 but this has not translated to long-term success in humans.14,15 A randomized controlled trial of systemic steroids for the prevention of epiretinal membrane following primary RD repair showed a lower rate of ERM in the experimental group, but no difference in visual acuity outcomes.16 One retrospective series that achieved good outcomes involved 2 mg triamcinolone acetate administered intravitreally at the end of vitrectomy surgery with silicone oil tamponade.17 However, a randomized trial in eyes with at least Grade C PVR that compared 4 mg triamcinolone injection following silicone oil infusion with no triamcinolone found no significant difference in anatomic success rate, visual acuity or PVR recurrence at six months.18 If access to compounded medication becomes more restricted, the dexamethasone intravitreal implant might be another experimental option.19
Anti-proliferative agents also seem to be good candidates for activity against PVR given the de-differentiation of mature cell lines and proliferation of the cellular membranes. One of the most tested compounds for PVR has been 5-fluorouracil.9 5-FU is frequently used in glaucoma surgery to prevent the scarring associated with filtration procedures, so it has a pre-existing safety profile, albeit externally. Two prospective, randomized studies have been conducted of 5-FU in combination with low molecular weight heparin,20,21 which were then the subject of a meta-analysis given their differing results.22 A benefit was shown in subjects at higher risk of PVR,23 but not in an unselected population,21 which led the authors of the meta-analysis to urge that further research be conducted only in high-risk individuals.22
Retinoic acid, in the form of 13-cis-RA (isotretinoin), has also been tested in several trials. While commonly used by dermatologists for the treatment of acne, isotretinoin was originally developed as an anti-proliferative agent for the treatment of basal cell carcinomas. In a prospective randomized trial of 35 patients,24 those who received 20 mg daily had higher rates of retinal re-attachment, lower rates of epiretinal membrane formation and higher rates of ambulatory vision after at least one year of follow-up. Additionally, a randomized, placebo-controlled trial is currently under way at the Wills Eye Hospital evaluating the use of isotretinoin for the prevention of PVR in eyes with a primary retinal detachment at high risk for developing PVR as well as in eyes that have already failed primary surgery due to the development of PVR.
Daunorubicin, which inhibits DNA and RNA synthesis, has been tested in a large multicenter, prospective, randomized trial. Anatomical success rates were similar between the Daunorubicin and control groups, and there was no difference in best-corrected visual acuity.25 Some animal studies suggested a benefit of colchicine in models of PVR, but this was not borne out in a clinical trial in humans.26 Ribozymes are small RNA molecules that bind and cleave specific target mRNA sequences. One such molecule, VIT100, was tested in a trial of 134 patients with Grade C PVR undergoing vitrectomy, but it was not found to be effective.27
Perhaps the most vibrant current research involves attempting to inhibit growth factor pathways, though few human trials have been published.9 Ranibizumab, well-known to retinal specialists in angiogenic disease processes, has been shown to prevent PVR in rabbit models of disease.7 Kinase inhibitors work downstream at the intracellular signaling level and may block PVR processes caused by various upstream signals. In the near term, viral vectors may be able to insert genes for soluble receptors to block factors, and commonly used medications like N-acetlycysteine (NAC) may help block indirect platelet-derived growth factor activation through its antioxidant activity,28 though human data is lacking as yet.
We have learned a great deal about the pathogenesis of PVR over the past decades, but are still unable to reliably prevent its occurrence. At the current time, surgery is our only option for dealing with PVR; we do not have any proven surgical adjuvants or medical therapies. Many drugs have been tested and some clinical studies are ongoing, but we have a lot of ground to cover to more effectively treat this devastating disease process. REVIEW
Dr. Brady is an assistant professor of ophthalmology at the Wilmer Eye Institute, Johns Hopkins University School of Medicine in Baltimore.
Dr. Kaiser is on staff at Wills Eye Institute; is an assistant clinical Professor at Jefferson Medical School of Thomas Jefferson University Hospital; and practices at Mid Atlantic Retina, Philadelphia. Contact him at Wills Eye Institute, 840 Walnut St., Suite 1020, Philadelphia, Pa. 19107. Phone (215) 928-3300.
1. Pastor JC. Proliferative vitreoretinopathy: An overview. Surv Ophthalmol 1998;43:3-18.
2. Pastor JC, de la Rua ER, Martin F. Proliferative vitreoretinopathy: Risk factors and pathobiology. Prog Retin Eye Res 2002;21:127-44.
3. Garweg JG, Tappeiner C, Halberstadt M. Pathophysiology of Proliferative Vitreoretinopathy in Retinal Detachment. Surv Ophthalmol 2013;58(4):321-9.
4. Moysidis SN, Thanos A, Vavvas DG. Mechanisms of inflammation in proliferative vitreoretinopathy: From bench to bedside. Mediators Inflamm 2012;2012:815937.
5. Wladis EJ, Falk NS, Iglesias BV, Beer PM, Gosselin EJ. Analysis of the molecular biologic milieu of the vitreous in proliferative vitreoretinopathy. Retina 2013;33:807-11.
6. Lei H, Rheaume MA, Kazlauskas A. Recent developments in our understanding of how platelet-derived growth factor (PDGF) and its receptors contribute to proliferative vitreoretinopathy. Exp Eye Res 2010;90:376-81.
7. Pennock S, Kim D, Mukai S, et al. Ranibizumab is a potential prophylaxis for proliferative vitreoretinopathy, a nonangiogenic blinding disease. Am J Pathology 2013;182:1659-70.
8. Lei H, Velez G, Hovland P, Hirose T, Gilbertson D, Kazlauskas A. Growth factors outside the PDGF family drive experimental PVR. Invest Ophthalmol Vis Sci 2009;50:3394-403.
9. Sadaka A, Giuliari GP. Proliferative vitreoretinopathy: Current and emerging treatments. Clin Ophthalmol 2012;6:1325-33.
10. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: Results of a randomized clinical trial. Silicone Study Report 2. Arch Ophthalmol 1992;110:780-92.
11. Vitrectomy with silicone oil or sulfur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: Results of a randomized clinical trial. Silicone Study Report 1. Arch Ophthalmol 1992;110:770-9.
12. Yu J, Peng R, Chen H, Cui C, Ba J. Elucidation of the pathogenic mechanism of rhegmatogenous retinal detachment with proliferative vitreoretinopathy by proteomic analysis. Invest Ophthalmol Vis Sci 2012;53:8146-53.
13. Hui YN, Liang HC, Cai YS, Kirchhof B, Heimann K. Corticosteroids and daunomycin in the prevention of experimental proliferative vitreoretinopathy induced by macrophages. Graefe’s Arch Clin Exp Ophthalmol 1993;231:109-14.
14. Cheema RA, Peyman GA, Fang T, Jones A, Lukaris AD, Lim K. Triamcinolone acetonide as an adjuvant in the surgical treatment of retinal detachment with proliferative vitreoretinopathy. Ophthalmic Surg Lasers Imaging 2007;38:365-70.
15. Bali E, Feron EJ, Peperkamp E, Veckeneer M, Mulder PG, van Meurs JC. The effect of a preoperative subconjuntival injection of dexamethasone on blood-retinal barrier breakdown following scleral buckling retinal detachment surgery: A prospective randomized placebo-controlled double blind clinical trial. Graefe’s Arch Clin Exp Ophthalmol 2010;248:957-62.
16. Koerner F, Koerner-Stiefbold U, Garweg JG. Systemic corticosteroids reduce the risk of cellophane membranes after retinal detachment surgery: A prospective randomized placebo-controlled double-blind clinical trial. Graefe’s Arch Clin Exp Ophthalmol 2012;250:981-7.
17. Chen W, Chen H, Hou P, Fok A, Hu Y, Lam DS. Midterm results of low-dose intravitreal triamcinolone as adjunctive treatment for proliferative vitreoretinopathy. Retina 2011;31:1137-42.
18. Ahmadieh H, Feghhi M, Tabatabaei H, Shoeibi N, Ramezani A, Mohebbi MR. Triamcinolone acetonide in silicone-filled eyes as adjunctive treatment for proliferative vitreoretinopathy: A randomized clinical trial. Ophthalmology 2008;115:1938-43.
19. Reibaldi M, Russo A, Longo A, et al. Rhegmatogenous Retinal Detachment with a High Risk of Proliferative Vitreoretinopathy Treated with Episcleral Surgery and an Intravitreal Dexamethasone 0.7-mg Implant. Case Rep Ophthalmol 2013;4:79-83.
20. Asaria RH, Charteris DG. Proliferative vitreoretinopathy: Developments in pathogenesis and treatment. Compr Ophthalmol Update 2006;7:179-85.
21. Wickham L, Bunce C, Wong D, McGurn D, Charteris DG. Randomized controlled trial of combined 5-Fluorouracil and low-molecular-weight heparin in the management of unselected rhegmatogenous retinal detachments undergoing primary vitrectomy. Ophthalmology 2007;114:698-704.
22. Sundaram V, Barsam A, Virgili G. Intravitreal low molecular weight heparin and 5-Fluorouracil for the prevention of proliferative vitreoretinopathy following retinal reattachment surgery. Cochrane Database Syst Rev 2013;1:CD006421.
23. Asaria RH, Kon CH, Bunce C, et al. Adjuvant 5-fluorouracil and heparin prevents proliferative vitreoretinopathy: Results from a randomized, double-blind, controlled clinical trial. Ophthalmology 2001;108:1179-83.
24. Chang YC, Hu DN, Wu WC. Effect of oral 13-cis-retinoic acid treatment on postoperative clinical outcome of eyes with proliferative vitreoretinopathy. Am J Ophthalmol 2008;146:440-6.
25. Wiedemann P, Hilgers RD, Bauer P, Heimann K. Adjunctive daunorubicin in the treatment of proliferative vitreoretinopathy: Results of a multicenter clinical trial. Daunomycin Study Group. Am J Ophthalmol 1998;126:550-9.
26. Berman DH, Gombos GM. Proliferative vitreoretinopathy: Does oral low-dose colchicine have an inhibitory effect? A controlled study in humans. Ophthalmic Surg 1989;20:268-72.
27. Schiff WM, Hwang JC, Ober MD, et al. Safety and efficacy assessment of chimeric ribozyme to proliferating cell nuclear antigen to prevent recurrence of proliferative vitreoretinopathy. Arch Ophthalmol 2007;125:1161-7.
28. Lei H, Velez G, Cui J, et al. N-acetylcysteine suppresses retinal detachment in an experimental model of proliferative vitreoretinopathy. Am J Pathology 2010;177:132-40.



