REFRACTIVE SURGEONS HAVE been hard at work over the past year since the 2005 ARVO meeting, researching ways to improve outcomes, avoid complications and evaluate corneas. This year's refractive surgery presentations run the gamut from studies on the IntraLase and the best way to make a flap, to the use of low-dose mitomycin-C and the most accurate corneal thickness measurement devices. For a summary of these studies and how they may impact your practice, read on.
Studying Flaps
Investigators from both the United States and the Netherlands say the modification of laser parameters used with the IntraLase Pulsion femtosecond laser can reduce the incidence of postoperative glare.
The surgeons performed a retrospective review of 571 eyes of 301 patients on whom the Pulsion was used to make their LASIK flaps. They divided the eyes into two groups: Group I (403 eyes of 215 patients) consisted of patients treated with the Pulsion using a spot separation of 9 to 11 µm, line separation of 9 µm and raster energies from 1.3 to 2.6 µJ; Group II (168 eyes of 86 patients) consisted of patients treated with spot and line separation of 9 to 10 µm and a raster energy of 1.3 µJ.
At follow-up, 164 of the 215 Group-I patients were available (76 percent). Thirty-one patients, representing 58 operated eyes, reported symptoms of spectral starbursts around lights (called rainbow glare by the researchers), for an incidence of 19 percent. None of the patients in Group II reported these symptoms. The researchers say the spectral pattern most closely represented six to 12 radiating lines of rainbow-colored light, which was noted immediately after surgery and in some eyes diminished over time. They determined these lines to be caused by light scattering from the back surface of the flap, causing a constructive interference, and that they match the approximate raster spot separation and pattern of the Pulsion pulses. In Group II, however, there were no spectral lines because there was a tighter focus of the laser's optics, minimizing the light-scattering phenomenon.4330
An independent, small-scale, prospective, randomized study from the Mayo Clinic College of Medicine in Minnesota says there are only slight differences between the IntraLase and the Hansatome (Bausch & Lomb).
The researchers randomized one eye each of 20 patients to have a flap made by the femtosecond laser, with their fellow eyes undergoing Hansatome flap creation. The intended flap thickness was 120 µm with the IntraLase and 180 µm with the microkeratome.
The investigators found that corneal backscattered light, or the reflection of incoming light back in the direction it came from, was higher after the IntraLase than the Hansatome at one month, three months and six months. Backscatter was higher in both treatment groups at one and three months after LASIK compared to before.
High-contrast acuity, corrected and uncorrected, and contrast sensitivity didn't differ between treatments at any time. Flap thickness at one month was 142 ±16 µm for the IntraLase and 139 ±22 µm for the Hansatome.
At three months, seven patients preferred the microkeratome eye, five preferred the IntraLase eye and eight had no preference. Ocular preference didn't correspond to ocular dominance or better uncorrected visual acuity.
In the end, researchers say that though corneal backscatter is greater with the IntraLase during the first six months postop, patients don't perceive a difference in their vision.4331
In the same Mayo Clinic study, the researchers also looked at the Hansatome and IntraLase's effects on corneal nerves.
The investigators found that subbasal nerve density didn't differ between the treatments at any time postop, but was decreased at one, three and six months (p<0.001) compared to preoperative baseline. The corneal sensitivity, as measured by a Belmonte esthesiometer, didn't differ between the treatments at any time postop. The average sensitivity threshold to mechanical stimulation by a two-second puff of air was elevated a non-significant 30 to 31 percent at one month after both treatments compared to baseline (p>0.14).
The researchers concluded that the anatomical loss of subbasal nerves doesn't correspond to changes in mechanical corneal sensitivity.516
Vision Correction
Researchers from Virginia and Canada say that a prolate-shaped LASEK ablation increased contrast sensitivity scores in patients.
The physicians enrolled 194 eyes of 108 patients in a prospective trial. All eyes received LASEK with a prolate ablation using the Carl Zeiss Meditec MEL-80 excimer laser.
Using the Wilcoxon rank-sum analysis, the investigators compared the preop and postop contrast-sensitivity measurements. In both mesopic and scotopic conditions, they found contrast sensitivity to improve significantly at one year postop. Specifically, mesopic contrast sensitivity improved from 0.175 log units (SD ±0.108) to 0.128 log units (SD ±0.124; p<0.001). Scotopic contrast scores improved from 0.340 log units (SD ±0.114) to 0.224 log units (SD ±0.104; p<0.001). The study's findings run contrary to most of the conventional refractive surgery literature, in which there is usually no improvement or a loss in contrast after LASIK and PRK. The researchers contend their outcomes are the result of the combination of a prolate ablation and a surface treatment.518
A prospective study from Mexico says that though the Artisan phakic IOL (Ophtec; Verisyse in the United States) is an effective treatment for high myopia, the surgeon must watch the patient's endothelial cell count closely during follow-up.
The surgeons implanted the Artisan lens in 44 patients, 21 of whom received bilateral implantation. The average preop SE was -15 D, with an average astigmatism less than 3 D. The average anterior chamber depth was 3.13 mm.
Postop, all patients gained an average of six or more lines of uncorrected acuity, and one line of best-corrected acuity (p<0.01). There was no statistically significant difference in intraocular pressure. The average SE was reduced to -1.5 D from -15 D preop at one year, and the average anterior chamber depth postop was 3 mm.
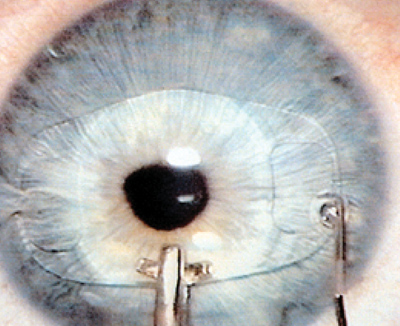 |
| Researchers advise to monitor endothelial cell counts closely after implanting the Artisan (Verisyse) lens. |
The researchers say that the decrease in endothelial cell density was statistically significant at a year, going from 2,640 preop to 2,741 at six months and then to 2,227 at a year (p<0.05). Iris atrophy occurred in 36 percent of cases, and decentration in 6 percent.318
Researchers from two military medical centers in San Antonio have taken a look at PRK compared to LASEK in moderate myopia in an independent study. The physicians reviewed the charts of 50 PRK and 50 LASEK eyes. The corrections ranged from -4 D to -8 D, with an average correction of -5.75 D for the PRK group and -6 D for LASEK. They defined visual recovery as an uncorrected acuity of 20/40 vision or better. No mitomycin-C was used.
Using a one-to-10 pain scale, the surgeons found pain to be similar between the two groups. There was corneal haze in six out of 60 eyes in the PRK group, and 16 out of 50 in the LASEK group. The PRK group had more eyes at 20/40 or better on postop days one and four than the LASEK group, though final uncorrected visual outcomes were similar between the two groups at six months. The investigators say that LASEK with alcohol, though effective, shouldn't be considered superior to standard PRK for the moderate myope.531
Surgeons at the U.S. Air Force Refractive Surgery Center at Lackland Air Force Base in Texas have performed the largest comparison study to date on LASEK vs. LASIK.
There were 1,310 eyes of 655 total patients in the independent study. Of these, 668 eyes of 324 patients underwent LASIK and 662 eyes of 331 patients had LASEK. Surgeons used the Visx Star S3, S4 and CustomVue lasers. The average preop manifest SE refraction was -4.69 D for the LASEK group, and -4.26 D for LASIK.
At 12 months, the LASEK group had statistically significantly better uncorrected visual acuity, 20/19.3 vs. 20/20.6 (p<0.001), while LASIK had significantly better best-corrected acuity: 20/16.5 vs. 20/17.6 (p<0.005). The LASEK patients had an average MSE of +0.026 D, compared to LASIK's -0.127, which was also statistically significant (p=0.006). There were no complications in the LASEK group, compared to two cases of diffuse lamellar keratitis in the LASIK patients.56
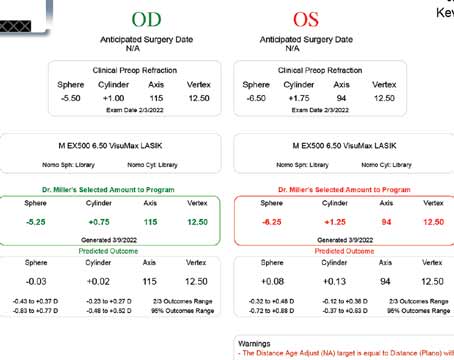
Researchers from the University of Rochester in New York, one of them a consultant for Bausch & Lomb, say a nomogram they've developed can improve outcomes with custom myopic LASIK with the Zyoptix system.
The Rochester nomogram integrates the preoperative manifest refraction's and higher-order aberrations' effects on postop sphere and cylinder results. In the study, 265 myopic eyes with an average spherical equivalent error of -4.7 ±2.02 D and an average higher-order root mean square value of aberrations of 0.53 ±0.14 µm were treated on the Bausch & Lomb Zyoptix system using the Rochester nomogram. One hundred seventy-five eyes were treated following a pharmacologically dilated wavefront measurement and 90 were treated based on non-pharmacologically dilated wavefront data. The one-month acuity and refractive error data from the surgeon's Zyoptix FDA trial results were used as a control (112 eyes; average SE: -3.41 ±1.44 D; RMS: 0.45 ±0.18 µm).
At one month, 94 percent of the study group and 91.5 percent of the FDA control group saw 20/20 or better (p<0.05). The rest of the results, including a nearly 13-fold decrease in overcorrections, appear in Table 1.
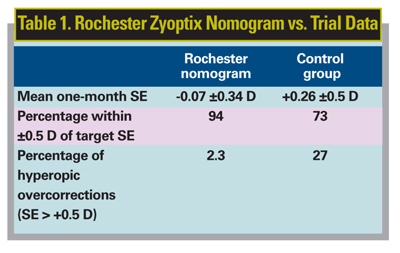
For the comparison of pharmacological dilation to non-pharmacological dilation, 93 percent of the pharmacologically dilated eyes and 95 percent of the non-pharmacologically dilated eyes attained uncorrected acuities of 20/20 or better. Ninety-seven percent of the non-pharmacologic eyes were within ±0.5 D of the target SE refraction, compared to 91 percent of the pharmacologic eyes. The average one-month SE was -0.11 ±0.34 D and -0.08 ±0.23 D for pharmacologically dilated and non-pharmacologically dilated treatments, respectively.3623
The same group also studied the effect that correcting spherical aberration has on refractive outcome after Zyoptix ablation, helping explain why the Rochester nomogram cuts down on hyperopic overcorrections.
The researchers measured the wavefront aberration and manifest refraction of 340 myopic eyes up to six months post LASIK. The average preop sphere and cylinder were -3.32 ±1.54 D and -0.68 ±0.59 D, respectively. They assessed theoretical retinal image quality by calculating the optical modulation transfer function in order to study interactions between lower and higher-order aberrations.
Seventy-four eyes (22 percent) had postop hyperopia greater than 0.5 D. On average, positive spherical aberration at six months postop was increased (0.17 ±0.15 µm for a 6-mm pupil) relative to preop levels. Eyes with larger amounts of preop positive spherical aberration had a smaller increase in positive spherical aberration but suffered larger hyperopic overcorrections. The researchers say that this smaller induced spherical aberration had a statistically significant correlation with the degree of postop hyperopia (p<0.001). They say this is because positive spherical aberration causes a myopic shift in refraction.
Conventional ablation algorithms, the researchers say, tend to overcorrect myopia and empirically compensate for the myopic shift. Custom algorithms, however, that reduce some of the positive spherical aberration, cause this interaction to become smaller, resulting in the postop hy-peropic overcorrection. By adjusting the nomogram so spherical aberration is taken into account, as with the Rochester nomogram, surgeons can improve the predictability of refractive outcomes.59
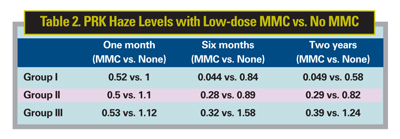
Researchers from the United States and India say that if you're concerned about the possible side effects of mitomycin-C in your surface ablation patients, you may want to try their low-dose regimen, which is 10 times less concentrated than the usual dose.
The researchers compared the results of PRK in 100 eyes in which mitomycin-C wasn't used to a similar number of eyes in which a low-dose (0.002%) was used. They varied the exposure times based on the severity of preop myopia: 45 seconds for -3 to -6 D (group I); 90 seconds for -6 to -9 D (group II); and two minutes for myopes over -9 D (group III).
The haze scores in each group were significantly less in the MMC groups at each postop time point, say researchers. (See Table 2, above) They add that the average uncorrected acuities were also better in the low-dose MMC eyes at one month (0.82 vs. 0.71; p=0.011), one year (0.84 vs. 0.75; p=0.032) and two years (0.82 vs. 0.69; p=0.014).526
Researchers from Detroit's Kresge Eye Institute say that laser vision correction can work successfully in patients with limbal stem-cell insufficiency.
In a retrospective fashion, the researchers reviewed the charts of three patients with limbal stem-cell insufficiency who underwent laser vision correction due to contact lens intolerance.
All patients were female with an average age of 38 years. The preoperative uncorrected visual acuity ranged from 20/60 to 20/400, and best-corrected visual acuity ranged from 20/20 to 20/30. Three eyes underwent LASIK, two had LASEK and PTK/PRK was performed on one eye with Salzmann's nodules. The average follow-up was 10 months (range: four to 24 months).
In five eyes, the postoperative uncorrected acuity was the same as the best-corrected acuity, 20/20 to 20/25. In the sixth eye, a central stromal divot was discovered after epithelial debridement during PTK/PRK. In this eye at one month, uncorrected vision was 20/200 and best-corrected vision was 20/25. At three months postop, this sixth eye underwent LASIK, which brought the uncorrected vision to 20/25. Signs of limbal stem-cell insufficiency had resolved in one patient by her two-year follow-up visit.561
Odds and Ends
Researchers from Glasgow Caledonian University say that, though Bausch & Lomb Orbscan's acoustic correction factor is helpful in determining central corneal thickness, clinicians shouldn't blindly rely on it when assessing more peripheral corneal locations.
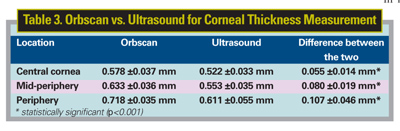
In an independent study, the investigators performed corneal pachymetry on 50 eyes of 25 healthy subjects. They extracted Orbscan II data at the geometric center, two mid-peripheral locations 2.5 mm to either side of the center, and peripheral locations 4.5 mm from the center along the horizontal meridian. They also obtained ultrasound readings from the same locations as Orbscan, after instillation of a drop of topical anesthetic. They took three readings at each location and averaged the measurements for each cornea. (Their findings appear in Table 3.)
The differences between the two modalities were statistically significant at all corneal locations, and the researchers add that the customary acoustic correction factor of 0.92 didn't correct them. Because of this, the researchers recommend using great caution when interpreting Orbscan depth measurements, especially in areas farther away from the corneal center.1326
In an independent study, researchers from Montreal and Paris say the Oculus Pentacam produces very accurate corneal thickness measurements when compared to ultrasonic pachymetry.
The clinicians tested both eyes of 22 normal subjects. At one visit, an observer acquired three Pentacam elevation maps, then measured corneal thickness in nine different locations with ultrasonic pachymetry: central; superior; nasal-superior; nasal; nasal-inferior; inferior; temporal-inferior; temporal; and temporal-superior. They obtained three successive ultrasonic measurements in each location. At another visit, within one to six weeks of the first, two observers acquired three more Pentacam maps. The order of the visits, observers and eyes were all randomized.
The researchers say that repeatability of the three successive measurements performed during the same visit ranged from substantial to almost perfect. The average intraclass correlation coefficient values, which measure the reliability/reproducibility of a measurement (with a value of 1 being perfect), were 0.94 for right eyes and 0.948 for left eyes. The lowest ICCs were obtained for the superior location measurements.
Compared to ultrasound's "true" values, the clinicians say the Pentacam's accuracy was almost perfect for all locations. ICCs ranged from 0.863 to 0.993 with an average of 0.933 for OD and from 0.891 to 0.988 with an average of 0.936 for OS. Central pachymetries yielded the highest values.
Inter-observer agreement was almost perfect, with ICCs above 0.985 for both eyes at all locations. Reproducibility over the two visits was also almost perfect, with ICCs ranging from 0.900 to 0.988 (average: 0.96) for OD and from 0.930 to 0.980 (average: 0.936).
Researchers say that accuracy at this level means the Pentacam could be used in place of ultrasonic pachymetry.1329
 |
| The Pentacam performed well when compared to ultrasonic pachymetry, according to an independent study. |
Researchers from Tennessee say a single Intacs segment is more effective than two in managing astigmatism due to causes like keratoconus and pellucid marginal degeneration.
The physicians reviewed the charts of 40 eyes of 36 patients who underwent Intacs placement. Twenty-one eyes received double segments and the rest got single segments. Twenty-five patients were being treated for keratoconus, six for PMD, four for irregular astigmatism and one for myopia.
The average follow-up was 27 weeks. The single group showed a statistically significantly greater reduction in astigmatism (1.75 D; p=0.006) compared to 0.75 for the double group.
The two groups were similar in terms of best-corrected acuity, with the double group improving from 20/60 to 20/30 on average, compared to an improvement from 20/60 to 20/40 in the single group. The single group had a slightly greater reduction in myopic spherical equivalent refraction (3.5 D vs. 2.5 D), but researchers say this wasn't statistically significant.4334
Dr. Probst is in private practice, and is the Chicago-land regional medical director for TLC Laser Centers.