Over the past few years, the spectrum of neovascular age-related macular degeneration has been expanded beyond the binary classic and occult choroidal neovascularization classification. These terms, classic and occult CNV, are clinical, morphological descriptions defined by fluorescein angiography characteristics.
To date, the spectrum of occult CNV has expanded to include entities like polypoidal choroidal neovascularization and retinal angiomatous proliferation (RAP).1 The term RAP describes a distinct form of occult CNV associated with proliferation of intraretinal capillaries in the paramacular area and a contiguous telangiectatic response that has a progressive vasogenic sequence.1
The distinct CNV entity, RAP, was first recognized and described in 1992 as a deep retinal vascular anomalous complex.2 In 1995, researchers modified the concept to include retinal choroidal anastomoses, particularly in the setting of pigmented epithelial detachments,3 and further modified the description in 1996 by describing RAP as deep retinal vascular anomalous complexes.4 In 2000, another group noted the presence of retinal-retinal anastomoses in RAP, but emphasized that this variant can occur without the presence of pigment epithelial detachments.5 The concepts were unified when the term RAP was coined in 2001.
The term RAP established, for the first time, a three-stage logical vasogenic sequence for this entity.
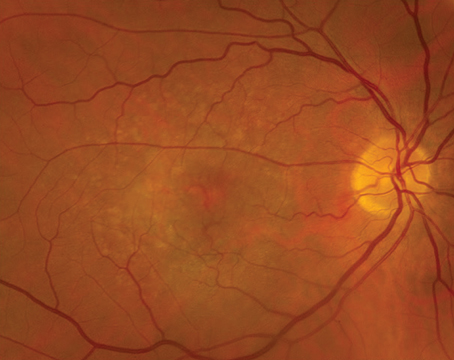
• Stage I, intraretinal neovascularization (IRN), describes the capillary proliferation within the retina that originates from the deep capillary plexus in the paramacular region. This stage is often accompanied by intraretinal hemorrhages and edema (See Figure 1).
 |
| Figure 1: Retinal angiomatous proliferation (RAP) Stage I: intraretinal neovascularization. |
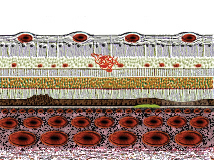
• Stage II consists of subretinal neovascularization (SRN) that occurs when the IRN extends posteriorly, beyond the photoreceptor layer of the retina into the subretinal space. A localized, neurosensory retinal detachment develops with increasing intraretinal edema, intraretinal and preretinal hemorrhages, as well as an associated serous pigment epithelial detachment (serous-PED) (See Figure 2).
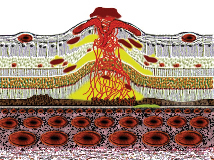 |
| Figure 2: RAP Stage II: subretinal neovascularization with a retinal-retinal anastomosis. |
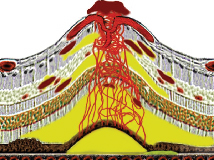
• Stage III describes choroidal neovascularization seen clinically and angiographically, sometimes in association with a vascularized pigment epithelial detachment (vascularized-PED) (See Figure 3). During the evolution of this vascularized process, an axonal communication between the retinal and choroidal circulation forms a retinal-choroidal anastomosis (RCA) (See Figure 4).
 |
| Figure 3: RAP Stage II: subretinal neovascularization with a serous pigment epithelial detachment. |
 |
| Figure 4: RAP Stage III: Choroidal neovascularization with a vascularized pigment epithelial detachment and a retinal-retinal anastomosis. |
Although it's the standard diagnostic adjunct for fundus imaging, fluorescein angiography is often of limited value in the diagnosis, evaluation and classification of RAP. It can, however, aid in the detection of IRN and other intraretinal abnormalities.
Indocyanine green angiography is an essential diagnostic adjunct in the accurate diagnosis of RAP. With this dye, the choroidal circulation can be better imaged than with fluorescein dye. RAP lesions can be identified best in the mid or late phases of the ICG angiogram. They are focal areas of hyperfluorescence, so-called "hot-spots," which increase in intensity as the ICG dye leaks into the surrounding intraretinal and subretinal spaces.6 Some series have suggested that the prevalence of RAP ranges from 10 to 15 percent. One study reported the incidence of RAP to be 21 percent, with 22 percent of the patients presenting with RAP and serous PED and 13 percent of patients presenting without a serous PED.5
Other work reported an incidence of 20.8 percent with the following stage division: Stage I, 1.7 percent; Stage II, 6.1 percent; Stage III, 7 percent with 6 percent indeterminate.7
The patients with RAP are clinically similar to patients with AMD. However, these patients tend to be slightly older (80) than the patients with both classic and occult CNV. The condition tends to be bilateral, with lesions presenting juxtafoveally. The most common clinical features of RAP include retinal and preretinal hemorrhages as well as pigment epithelial detachments. The intraretinal blood in this form of CNV is often small in nature and may be in multiple locations.
Accurate and early diagnosis of RAP is important when considering the available treatment modalities. Conventional thermal laser photocoagulation seems to work well in treating some Stage-I and early Stage-II RAP lesions outside the fovea. Once RAP exists in association with a PED, however, the treatment success with most therapies decreases dramatically.
While some retina specialists have treated RAP lesions with photodynamic therapy, the current trend seems to combine PDT with an intravitreal injection of triamcinolone. An anti-vasogenic agent, specifically, anecortave acetate, has been injected in the juxtascleral space in a prospective clinical trial. Alone, it has been minimally effective. When combined with PDT, however, the results seem better.
One final treatment option involves surgical excision of the feeder artery and vein with diathermy, when appropriate, for Stage-II RAP lesions with or without serous PED.8 Presently, one therapy does not seem dramatically better than another. Future treatments will likely focus on a combined therapeutic approach to managing RAP lesions.
*Co-authors, from the LuEsther T. Mertz Retinal Research Center, Manhattan Eye, Ear & Throat Hospital, New York, N.Y., include Nicole E. Gross, MD, Antonio Ciardella, MD, Jason S. Slakter, MD, John A. Sorenson, MD, Richard F. Spaide, MD, K. Bailey Freund, MD.
Supported by the Macula Foundation, Inc. The authors have no financial interest in any aspect of this review. Dr. Yanuzzi practices at Vitreous-Retina-Macula Consultants of New York, 519 East 72nd St., Suite 203, New York, NY 10021. Contact him at (212) 861-9797, fax: (212) 628-0698, or e-mail: vrmny@aol.com.
1. Yannuzzi LA, Negrao S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter J, Freund KB, Sorenson J, Orlock D, Borodoker N. Retinal angiomatous proliferation in age-related macular degeneration. Retina 2001;21(5):416-34.
2. Hartnett ME, Weiter JJ, Gardts A, Jalkh AE. Classification of retinal pigment epithelial detachments associated with drusen. Graefes Arch Clin Exp Ophthalmol 1992;230:11–19.
3. Kuhn D, Meunier I, Soubrane G, Coscas G. Imaging of chorioretinal anastomoses in vascularized retinal pigment epithelium detachments. Arch Ophthalmol 1995;113:1392–1398.
4. Hartnett ME, Weiter JJ, Staurenghi G, Elsner AE. Deep retinal vascular anomalous complexes in advanced age-related macular degeneration. Ophthalmology 1996;103:2042–2053.
5. Slakter JS, Yannuzzi LA, Schneider U, et al. Retinal choroidal anastomoses and occult choroidal neovascularization in age-related macular degeneration. Ophthalmology 2000;107:742–754.
6. Fernandes LH, Freund KB, Yannuzzi LA, Spaide RF, Huang SJ, Slakter JS, Sorenson JA. The nature of focal areas of hyperfluorescence of "hot pots" imaged with indocyanine green angiography. Retina 2002;22(5):557-68.
7. Coleman HR, Barbazetto IA, Costa D, et al. Prevalence of retinal angiomatous proliferation in exudative age related macular degeneration within a retinal practice. Manuscript submitted to Ophthalmology.
8. Borrillo JL, Martididis A, Federman JL, Sivalingam A. Surgical management of retinal angiomatous proliferation. Archives Ophthalmol 2003;121:558-561.