Researchers in Japan studied patient records to analyze the factors related to the development of epiretinal membranes after pars plana vitrectomy surgery for the repair of retinal detachment.
The investigators reviewed 2,239 cases treated with PPV for RRD repair registered in the Japan Retinal Detachment Registry between February 2016 and March 2017. They used univariate analysis to analyze associations of 13 baseline characteristics and eight surgical procedures with ERM formation. The researchers report that ERM had developed in 104 cases (4.6 percent) by six months.
They found that drainage retinotomy was significantly associated with ERM (odds ratio: 2.22 [95% confidence interval: 1.50-3.31]; p<0.001). In the propensity score-matched analysis (n=492 in each group), the researchers confirmed a significant difference in the incidence of ERM after six months of vitrectomy (8.3 percent and 2.6 percent in cases with and without drainage retinotomy, respectively; OR 3.35 [95% CI 1.77-6.33]; p<0.001).
The researchers say that, though a drainage retinotomy is now less frequently used because of the increased use of microincision vitrectomy surgery with a wide-angle viewing system, and the availability of perfluorocarbon liquid, 677 cases (30.3 percent) still underwent drainage retinotomy between 2016 and 2017 in the J-RD Registry. They say that knowledge of the increased risk of macular pucker after a drainage retinotomy may help surgeons reconsider its application and case selection. In addition, they say, prophylactic ILM peeling may be necessary in the cases that undergo drainage retinotomy, to avoid a reoperation for ERM removal.
Am J Ophthalmol 2022;234: 20–27.
Ishikawa K, Akiyama M, Mori K.
Predicting the Outcome of SLT
Researchers in New Delhi, India, sought to evaluate whether the presence of angle dysgenesis—defined as the absence of Schlemm’s canal and/or the presence of a hyperreflective membrane over the trabecular meshwork, as determined on anterior segment optical coherence tomography (ADoA)—could be a predictive factor in determining the outcome of selective laser trabeculoplasty treatment.
They conducted a prospective clinical cohort study involving 35 patients with juvenile-onset open-angle glaucoma and uncontrolled intraocular pressure, who didn’t show angle dysgenesis on gonioscopy. After evaluation for ADoA using AS-OCT, the subjects underwent SLT. Successful SLT treatment was defined as a reduction of IOP by 20 percent or more from the pre-laser value at six-month follow-up, without any further IOP-lowering medication or surgery. (One repeat SLT during the six-month period was admissible.)
A successful reduction in IOP at six-month follow-up was then correlated with the extent of ADoA. Furthermore, the number of AS-OCT B-scans in which Schlemm’s canal was identified as present were quantified.
Findings included:
- In comparison to pre-SLT IOP, 57.1 percent of eyes (20/35) showed a more than 20-percent reduction in IOP at six months, with a mean reduction of 7.6 ±1.8 mmHg (29.6 percent).
- When all three observers agreed, SC was identified in 90 percent of eyes that were succesfully treated (18/20), vs. 26.6 percent of eyes that failed (4/15) (p<0.001).
- All five eyes with a hyperreflective membrane showed treatment failure (p<0.001).
- All 19 eyes in which SC was present in more than 50 percent of ASOCT B scans showed treatment success (p<0.001).
- On a bias-reduced regression analysis, the identification of SC on any two consecutive scans increased the chances of SLT treatment success at six months by 8.3 times. The identification of SC in more than 50 percent of AS-OCT scans was associated with a 21.4 times greater chance of success.
The authors concluded that the presence of SC on AS-OCT is a strong predictor for successful IOP reduction after SLT in JOAG eyes.
Am J Ophthalmol 2022;234:126-137.
Varshney T, Azmira K, Gupta S, et al.
Vision After Macula-off vs. Macula-on Detachment Repair
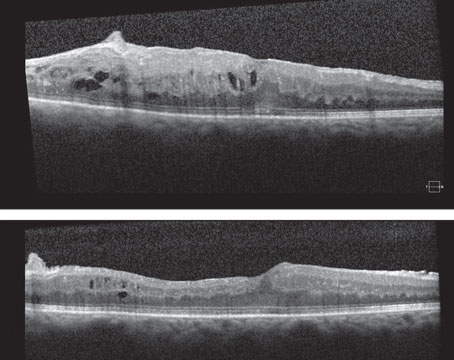
Researchers in the United Kingdom recently investigated the relationship between retinal anatomic characteristics, visual acuity and perimetric retinal sensitivity in patients following retinal reattachment surgery, finding that the central outer nuclear layer and outer retinal segment thinning correlated with decreased retinal sensitivity and may be explained by rhegmatogenous retinal detachment photoreceptor death. They noted there was greater thinning following macula-off RRD compared with macula-on RRD.
The study assessed 13 macula-on and eight macula-off patients before and six months after vitreoretinal surgery. The researchers recorded the OCT thickness of the outer nuclear layer, outer retinal segment, retinal pigment epithelium to the ellipsoid zone, and external limiting membrane to the ellipsoid zone at six months post-op. They then compared their findings with BCVA and retinal sensitivity.
The mean outer nuclear layer thickness was higher after macula-on RRD compared with macula-off (97.7 µm vs. 73.1 µm). Central outer nuclear layer thickness was strongly associated with retinal sensitivity and less strongly with BCVA. In all RRD eyes, every 1-µm decrease in outer nuclear layer thickness correlated with a 0.052-dB decrease in retinal sensitivity, and every 1-µm decrease in outer retinal segment thickness was associated with a 0.062-dB reduction in retinal sensitivity. The other thickness measurements didn’t correlate with BCVA post-retinal reattachment surgery.
The researchers said they believe that retinal detachment causes photoreceptor apoptosis and that foveal cone morphology after reattachment correlates with VA.
“The associations between outer nuclear layer thickness and retinal sensitivity and visual acuity support the hypothesis that photoreceptor apoptosis after macula-off retinal detachment contributes to reduced visual function,” they noted in their paper.
However, because they used clinical examination to distinguish macula-off and macula-on RRD, it’s possible that some macula-on RRD patients might have had subclinical subretinal fluid in the macula. This possibility limits the study’s ability to make distinctions between the relationships in macula-on as opposed to macula-off RRD.
Graefes Arch Clin Exp Ophthalmol 2022, Jan 26. [Epub ahead of print].
Rasool S, Kaushik M, Chaudhary R, et al.
Color-vision Deficiency and Myopia in Children
Scientists explored the relationship between color vision deficiency, myopia progression and axial elongation in Chinese primary school children during a five-year cohort study.
A total of 2,849 grade one students (ages 7.1 ±0.4 years) from 11 primary schools were enrolled and followed for five years. Cycloplegic autorefraction and axial length were measured annually. Color vision testing was performed annually using Ishihara’s test and the City University color vision test.
Here are some of the findings:
- The prevalence of color vision deficiency was 1.68 percent (2.81 percent in boys and 0.16 percent in girls).
- Color-deficient cases consisted of 91.6 percent deutan and 8.3 percent protan.
- The cumulative incidence of myopia was 35.4 percent (17/48) in the color-vision deficiency group, which was lower than 56.7 percent (1,017/1,794) in the normal group (p=0.004).
- The change in spherical equivalent refraction in the color vision deficiency group (-1.81 D) was also significantly lower than that in the normal group (-2.41 D) (p=0.002).
Scientists wrote that the lower incidence and slower progression of myopia in children with color vision deficiency over the five-year follow-up period suggests that color-deficient individuals were less susceptible to myopia onset and development.
IOVS 2022;2;63:2:2.
Gan J, Li SM, Atchison DA, et al.
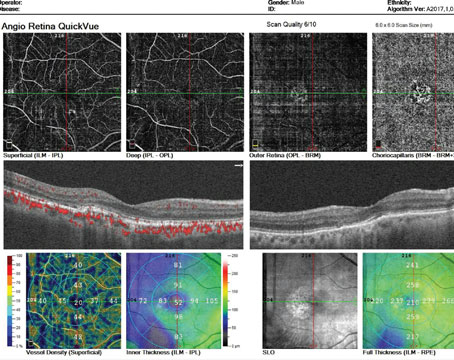
Retinal Imaging May Help Predict Heart-attack Risk
New research suggests retinal imaging may be capable of identifying patients at high risk for heart attack based on retinal biomarkers associated with cardiac function, such as retinal blood vessel density and tortuosity.
To predict incident myocardial infarction, the researchers used a combination of retinal images and patient metadata to estimate left ventricle mass and end-diastolic volume in 5,663 qualifying subjects. Their models employed cardiovascular magnetic resonance imaging (end-diastolic, short-axis view), retinal imaging and demographic data from the U.K. Biobank imaging study.
They found the following, based solely on retinal images and demographic data:
- Mean left ventricle mass was
4.4 g. - Mean left ventricular end-diastolic volume was 3.02 ml.
- Risk of myocardial infarction had an area under the curve of 0.8, a sensitivity of 0.74 and a specificity of 0.71.
“Our results indicate that one could identify patients at high risk of future myocardial infarction from retinal imaging available in every optician and eye clinic,” the authors wrote in their paper. They noted that using cardiac indices and demographic data together (vs. using demographic data alone) can improve the prediction of heart attack incidence.
They tested their method on the AREDS dataset as well, reporting a slightly lower performance, but an overall discrimination capacity similar to that of established cardiovascular disease risk assessment models. “This highlights the potential for our approach to be employed as a second referral tool in eye clinics/opticians to identify patients at risk of future myocardial infarction events,” they wrote.
Nature Machine Intel 2022;4:55-1.
Diaz-Pinto A, Ravikumar N, Attar R, et al.