There are few instances in life in which you can enhance something without suffering a trade-off elsewhere; if you want a more powerful car, for example, you'll probably have to sacrifice gas mileage. Bong-Hyun Kim, MD, of
Dr. Kim's apparatus, the Near Infrared Operating Microscope, consists of a Zeiss microscope, a halogen lamp, two charge-coupled device cameras that provide a stereoscopic image and an optical filter mount that includes a filter that transmits near-infrared wavelengths greater than 850 nm and a visible light-reflecting filter. The surgeon can use a selector knob to choose whether NIR or visible light is used for the surgery.
"As the human eye cannot see the NIR that is a light source of the NIOM, I used the NIR-sensitive [stereoscopic CCD] cameras to obtain images," explains Dr. Kim. "To display images, I used a head-mounted display. The surgeon can see the eye images through the HMD instead of binocular tubes of the conventional microscope." The resolution of the image is 800 x 600, displaying 1.4 million pixels.
Dr. Kim says the main benefits of using NIR instead of the usual visible-light lamp are a complete elimination of the "high-risk" wavelengths from 400 to 500 nm that can cause phototoxic retinopathy,1,2 as well as an elimination of the light-induced retinal bleaching that can impede patients from achieving their best vision in the immediate postop period.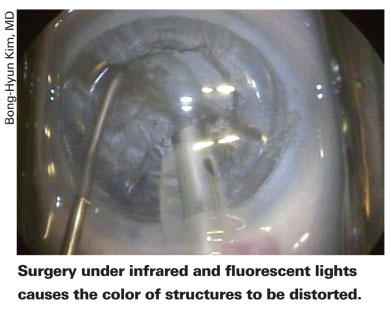
In a study of 70 patients in whom Dr. Kim used the NIOM, 40 percent could see 20/20 to 20/40 uncorrected 30 minutes postop. There was a posterior capsule rupture in one patient (1.4 percent) and iris damage in another two (2.9 percent). In a small initial study in which he compared surgery with the NIOM to that using conventional illumination in four patients, the NIOM patients recovered their vision faster, while the other patients complained of pink or yellow color distortions. The color distortions eventually resolved.
Dr. Kim says the system can reduce mydriatic drug-related complications, since the system depends on physiologic pupil dilation under ambient lighting. It might be helpful for teaching as well, since the system lets four others see the same stereoscopic image as the surgeon vs. a conventional microscope, which allows only two other viewers. The surgeon can also assume a more comfortable position while doing the surgery, since he gets the same view of the surgical site via the head-mounted display regardless of his position or posture.
In practice, using the system can take some adjustment, according to Dr. Kim. "When the scope was used in the dark, the operative field appeared black and white," he says. "The intraocular tissues were not clearly distinguishable from each other. Under fluorescent room lighting [but still without the conventional microscope light], there was color, but it was distorted. The brown iris appeared as blue, the lens as transparent blue and red reflex as blue. The conjunctival vessels and bleeding from the vessels were also less apparent." In addition to the differently colored ocular structures, Dr. Kim says the learning curve also involves getting used to the unfamiliar feel of wearing the head-mounted display.
"I'm testing different types of display apparatus such as the 3-D LCD monitor with and without glasses," says Dr. Kim. "If the monitor is good enough, we don't need to wear the head-mounted display. So far, though, my opinion is that the head-mounted display is superior to the monitor."
Though the system has certain benefits, it also has some shortcomings, in addition to the unfamiliar head-mounted display and color distortion of intraocular structures as they appear under fluorescent lighting. For one, Dr. Kim says though the resolution is good, the image quality of the conventional microscope is still better. The NIOM's resolution currently isn't high enough to allow a surgeon to properly perform such maneuvers as an anterior vitrectomy and scleral fixation of an intraocular lens, for example. He adds, however, "Resolution will improve as the technology improves."
The viewing system also reduces the view of the operating field, so the surgeon must frequently adjust the x, y and z axes to view the procedure. Dr. Kim adds that, to enjoy the benefits of a fast visual recovery, topical anesthesia is necessary.
Looking to the future, Dr. Kim plans on further improving the system with an eye toward eventually marketing it.
"I'd like to improve the image quality by using upgraded cameras," he says. "The current image resolution of SVGA 800 x 600 and 1.44 million pixels is sufficiently good to do cataract surgery, but isn't yet better than the conventional microscope."
1. Kleinmann G, Hoffman P, Schechtman E, et al. Microscope-induced retinal phototoxicity in cataract surgery of short duration. Ophthalmology 2002;109:2:334-8.
2. Long VW, Woodruff GH. Bilateral retinal phototoxic injury during cataract surgery in a child. J AAPOS 2004; 8:3:278-9.



