Innovation in the dry-eye space has taken off over the last few decades, and now ophthalmologists have more options than ever before for treating patients’ dry-eye disease. “It’s an amazing time to be a specialist in this area because there are so many different therapeutic options available to handle the complexity and variety of the ocular surface issues we encounter on a day-to-day basis in the clinic,” says Christopher Starr, MD, FACS, a cornea and cataract/refractive specialist at Weill Cornell Medicine in New York. “As new treatments get FDA approved and become available, I try to incorporate them into my personal algorithm.”
While it’s an exciting time, the plethora of options might feel overwhelming. What’s the best way to incorporate all these into your practice? We spoke with several dry-eye experts to learn about their specific approaches and to find out how they’re using the newly approved treatments.
A DED Roadmap
Treating patients’ dry eye can be as complex as the disease itself. Many clinicians find dry-eye treatment algorithms—such as DEWS II, CEDARS and the ASCRS Preoperative Ocular Surface Disease algorithm—helpful because they remove some of the mental load when it comes to deciding next steps based on diagnosis or severity.
“It’s a balance—that’s why it’s called the Art of Medicine,” says Sabrina Mukhtar, MD, a cornea specialist at the University of Pittsburgh Medical Center. “I use the ASCRS algorithm since I’m in a referral practice and many of my patients are referred to me for procedures. Even if you go through the algorithm and have a list of treatments for the patient, I work with them to address the high-impact things.”
 |
“I look at the ASCRS algorithm, but I don’t always follow it exactly,” says Amy Lin, MD, a cornea specialist at the Moran Eye Center in Salt Lake City. “It’s nice to see what all the options are at each step, and it can be good to perform things in a stepwise function. I try to tailor the dry-eye treatment for the patient. For example, ideally, I like to start patients on a long-term topical anti-inflammatory for treatment for dry eye prior to placing punctal plugs. But, if there are insurance or cost issues that prohibit the use of any of the topical anti-inflammatories, then I may go to punctal plugs next. If those fall out but the patient feels relief when they’re in, then I may jump to punctal cautery as the next step after plugs.
“If a patient really doesn’t like eye drops, if they don’t have the means to instill eye drops because of disability or they don’t have anyone who can help them put drops in, then the varenicline nasal spray can be a nice alternative,” she continues. “I have patients who don’t want any prescriptions at all—no drops or any oral medications. They want to keep things natural. For these patients, the nasal spray can be a good option because it stimulates the patient’s own tears. That might be something I introduce early on, maybe right after artificial tears for certain patients.”
Treat the Underlying Cause
Failing to treat the underlying cause of dry eye is one of the biggest challenges of managing this chronic condition. The bread and butter of dry-eye treatment revolves around the diagnosis, Dr. Starr explains. “When we wrote the ASCRS Preoperative Ocular Surface Disease algorithm, treatment decisions hinged on accurate diagnoses. To this day, many clinicians lump any symptoms of ocular surface disease together and call it ‘dry eye’ and treat it as if it were simple ‘dry eye.’ That’s what led to a lot of the frustration for both doctors and patients, because without a careful diagnosis, the treatment’s not going to be right.”
An ocular surface disease diagnosis is often multifactorial. “There are multiple ocular surface disease subtypes, all of which might contribute simultaneously to the constellation of symptoms that a patient might be having. So, it behooves us to spend a little extra time during the exam on symptom identification. This is where questionnaires come in and talking to the patients about exactly what their symptoms are. If you just treat based off a remark like, ‘my eyes are irritated,’ you’re going to mistreat many, many times. These patients are going to take a little bit longer than, say, the average cataract patient, where the presence or absence of a significant cataract isn’t much of a diagnostic challenge. That said, in the era of modern medicine, time constraints and reimbursements are a significant challenge, and it’s often difficult to secure this additional chair time for complex dry-eye disease/ocular surface disease patients.”
 |
Dr. Mukhtar agrees. “We often don’t have time in our busy clinics to sit down and truly talk to the patient and understand why they’re having their symptoms,” she says. “To address this challenge, the University of Pittsburgh Medical Center established a dry eye center of excellence. We see fewer patients each day, but they have a longer visit. They’re typically referred to us from our other colleagues in the department.
“Whenever you see a patient, it’s a snapshot in time and can be difficult to figure out all the potential factors contributing to their dry-eye disease,” she continues. “We have this questionnaire called CSI Dry Eye that uses machine learning to compute reasons why a patient may have dry eye based on lifestyle, diet, treatments, medications, medical problems, and so on. This makes it a lot easier for the eye-care provider because it helps us target our therapy. We can’t fix everything at one visit, but we can focus on the top one or two things that bother patients.”
When speaking with patients, Dr. Starr and Dr. Mukhtar say a useful questions to ask is, “What is the thing that bothers you most about your eyes?” Dr. Starr says, “Usually, these patients have a long list of complaints, and but usually one symptom is at the top of the list, and this helps me prioritize what symptom I’m going to try to control first, whether that’s a vision-related thing or discomfort, itching, crusting or redness, etc.”
Most of the dry-eye patients Dr. Starr sees are referred to him after trying multiple medications. “Their frustration levels are pretty high because they’re still suffering,” he says. “These patients tend to be more challenging and complex and require an upfront discussion to attempt to isolate symptoms and talk about what has worked and what hasn’t, or when the symptoms occur. You have to always be thinking about the corneal nerves too. Corneal neuropathic pain and neurotrophic keratitis are often misdiagnosed, diagnosed late or not diagnosed at all.”
“Neurotrophic keratitis patients may have decreased corneal sensation,” Dr. Lin says. “These are challenging patients to treat because have little to no clinical signs yet have very severe symptoms. Oxervate may be prescribed for even as low as stage one NK, but certainly should be entertained for stages two or three. These patients may actually fall into the neuropathic pain category, which is very difficult to treat.”
“If a patient tells me they feel worse at the beginning of the day and wake up with gritty eyes, that tells me they have a little bit of lagophthalmos or possibly floppy eyelid syndrome, where their eyes are drying out overnight,” Dr. Mukhtar says. “So, that’s what we’ll target, whether it’s through lubricating ointments or nighttime goggles. If the patient tells me their eyes feel worse as the day goes on, especially while at work, that tells me it might be incomplete blink and likely meibomian gland dysfunction.”
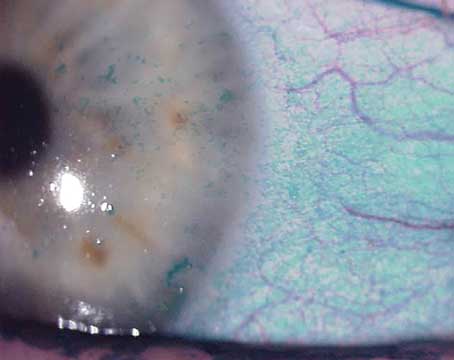
Dr. Mukhtar performs a full review of the patient’s medical issues and medications. “We want to make sure we have an understanding of what’s contributing [to the dry eye],” she says. “It’s pretty in-depth. Dry eye is quite medical. Because we’re a referral center, we see a lot of autoimmune conditions. In fact, we have a dedicated Sjögren’s clinic where a rheumatologist and one of our cornea partners co-manage patients because their systemic treatment is really important. In the dry-eye clinic, we also see a lot of long-term chemotherapy patients, since that can cause dry eye too. I’ve diagnosed many sleep apnea cases since I examine patients’ eyelids. Thyroid disease may also be identified since there’s a specific staining, which is important to do.”
Unfortunately, reimbursement and coverage for many dry-eye treatments including those newly approved remain persistent challenges for both providers and patients. “The reality of the situation is the accessibility of new treatments is sometimes hindered by insurance coverage,” says Beeran Meghpara, MD, a cornea and cataract/refractive specialist at Wills Eye Hospital in Philadelphia. “Often, the paperwork that’s required on the part of the practitioner to get these medications to patients is cumbersome, and despite us doing all the paperwork, co-pays may be extremely high. This is by far one of the biggest challenges when it comes to getting new treatment options into the hands of patients.”
Three Things First
Dr. Mukhtar gives every dry-eye patient a homework sheet with a few things she says every patient should do, regardless of why they have dry eye:
1. A warm compress. “Incomplete blink is one of the most common causes of dry eye that then contributes to meibomian gland dysfunction,” she says. “I compare this to brushing your teeth every day. It’s important to take care of your eyelids as well.
2. Blinking exercises. “Going off the 20/20/20 rule, I tell patients to blink actively 20 times to stimulate the lacrimal and meibomian glands.
3. Environmental modifications. Some of these include using larger text when working on the computer, using an anti-glare monitor and ensuring active air isn’t moving into the eyes.”
 |
Quieting Inflammation
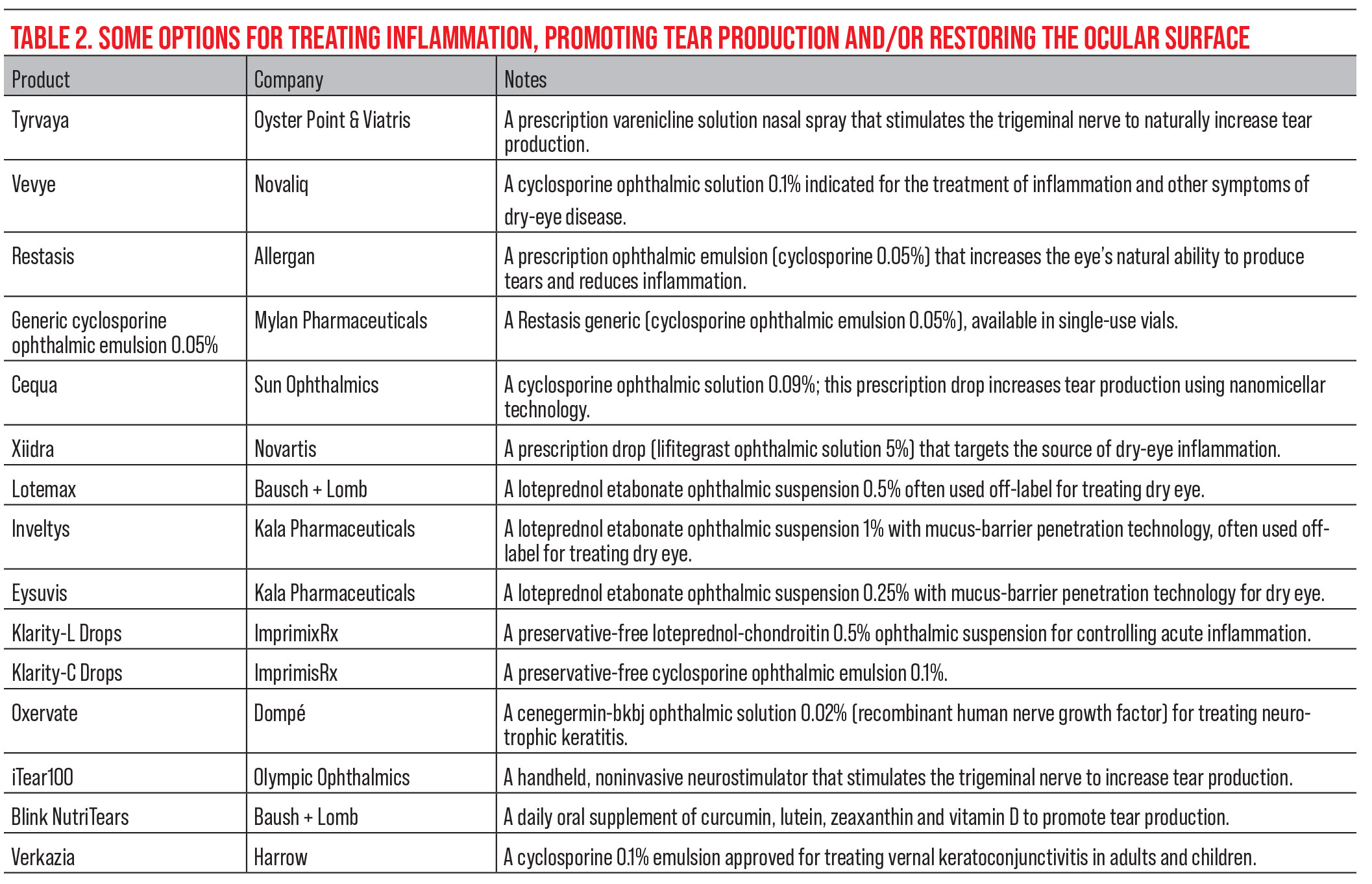
One of the major underlying causes of dry eye is inflammation. “Anti-inflammatory medications include steroid eye drops, some of which are specifically indicated for dry eye while others are used off-label, and steroid-sparing agents or immunomodulators,” Dr. Meghapra says. “Steroid eye drops are a short-term treatment since the long-term side effects may include high pressures and cataract formation. Immunomodulators, on the other hand, are a long-term treatment. There are a handful of these drops available, including Restasis, Cequa and now Vevye, which are all cyclosporine, and Xiidra, which is lifitegrast.
“If a patient isn’t doing well on Restasis, I’ll often switch to Cequa because it has a higher concentration of cyclosporine and a newer vehicle,” he continues. “However, if a patient still isn’t doing well on Cequa or they’re not happy with their symptom control, then I’ll usually switch them to a different class of medication, such as serum tears.”
“Vevye has been a great option for patients with both aqueous deficient and inflammatory dry eye mixed in with evaporative dry eye,” says Soroosh Behshad, MD, MPH, a cornea and cataract/refractive specialist at Emory University School of Medicine. “I find that patients who haven’t tolerated previous options such as Restasis, Cequa or Xiidra, due to symptoms of burning or irritation, do better with Vevye and demonstrate clinical improvement in about two to four weeks.” He adds that his patients have had difficulty with the bottle and report wasting drops.
“I’ve used Vevye for patients who [couldn’t tolerate] the burning and stinging of other cyclosporine drops,” Dr. Mukhtar says. “The limitation, unfortunately, is the cost. It’s just a limitation for a lot of these dry-eye medications. It’s really hard to get them covered for our patients, especially the older patients, who seem to need it the most. If you have commercial insurance, it’s pretty easy to get these medications through specialty pharmacies at a reasonable cost, but the reason I don’t use Vevye much is because my older patients have trouble getting it.”
For patients suffering from this condition, Dr. Mukhtar says that in addition to warm compresses, “I try to get them on some anti-inflammatory medication such as cyclosporine or lifitegrast in addition to a steroid taper to calm things down, since these anti-inflammatories take almost two months to work.
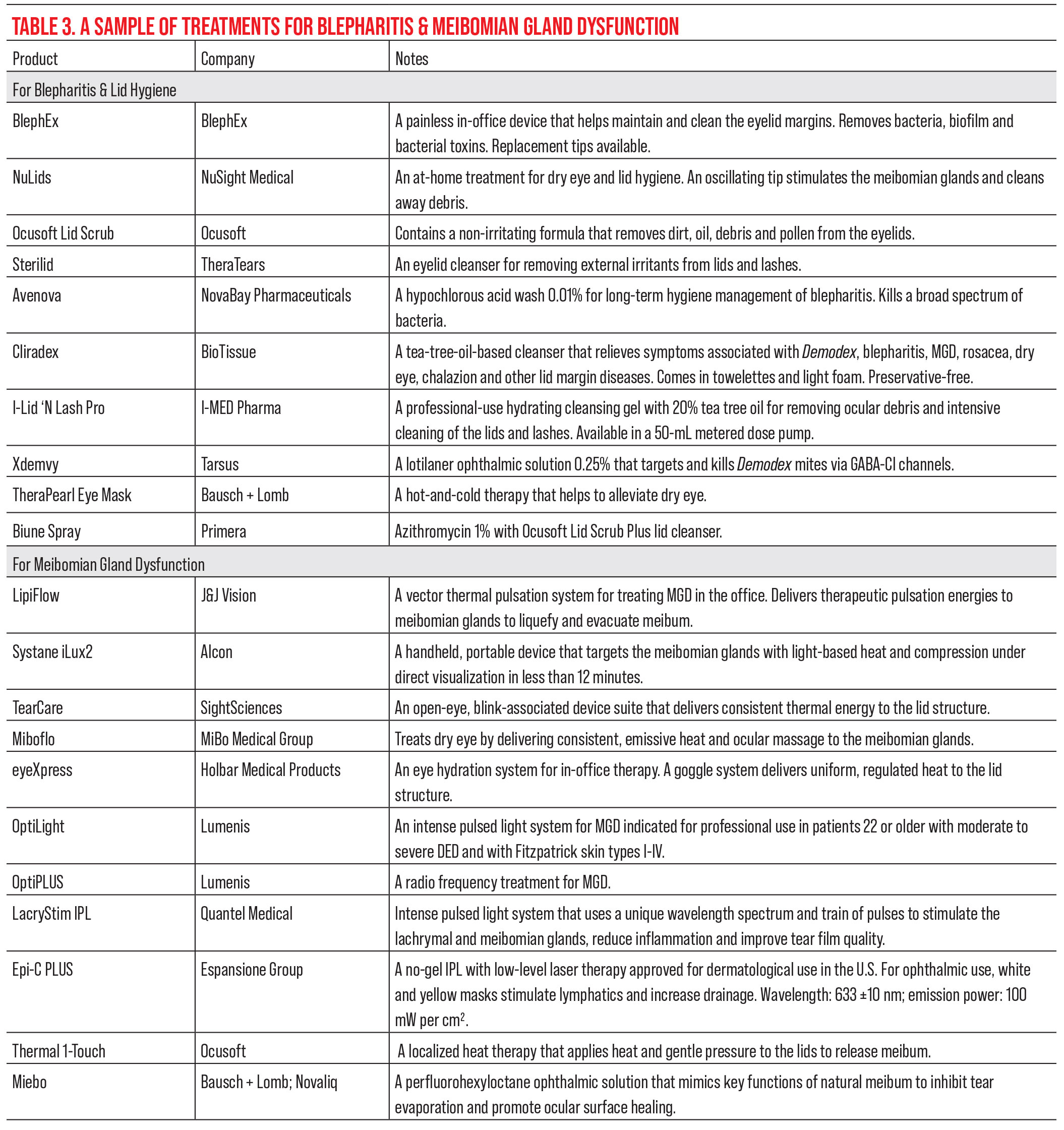
“The procedure I most commonly do for ocular rosacea patients is intense pulsed light therapy,” she continues. “It has been FDA approved for meibomian gland dysfunction as well. It’s very good at controlling these vicious inflammatory cycles—what happens in ocular rosacea is that the dilated blood vessels bring inflammatory mediators to the surface of the eye, which creates the vicious cycle. If I start patients on a topical anti-inflammatory, that’s not really treating the underlying cause. In order to achieve success with IPL, choose the right patient to do it on. It won’t treat dry eye caused by Sjögren’s disease because that’s a different pathophysiology.”
She notes that there are several key limitations for IPL. “If a patient has active herpetic keratitis or any herpetic disease in the eye, I wouldn’t do IPL then,” she says. “Any active uveitis is also a contraindication. IPL is also suitable only for certain Fitzpatrick skin types. Patients with darker skin or more melanin in their skin aren’t good candidates. Radiofrequency treatments, which use a different method to heat up the oil glands to improve function and treat inflammation, is another option, but I don’t use that in my practice yet.”
For persistent, severe dry eye, amniotic membrane can help stave off some symptoms with the growth factors and stem cells they contain as well as their anti-inflammatory properties. “I’ve used [amniotic membrane] extensively in patients with non-healing corneal epithelial defects, Stevens Johnson Syndrome or burns, but recently I’ve started using it for some patients with dry-eye disease,” Dr. Lin says. “I probably wouldn’t bring up the option until a patient has failed multiple treatments. It’s important to tell patients it can be a bit uncomfortable for a few days and will blur vision significantly while it’s in. However, for the right patient, it can be a very effective treatment for decreasing dry-eye symptoms for several months.”
Making and Keeping Tears
For patients with evaporative dry eye, production of additional tears that remain on the ocular surface can help soothe symptoms. Tyrvaya activates the trigeminal parasympathetic pathway to stimulate basal tear production.
“I see many patients who’d rather not take drops or who have a hard time placing them,” Dr. Starr says. “Tyrvaya nasal spray is a much easier and preferred route of administration for these patients. It not only increases aqueous volume but also stimulates meibum and mucin secretions, making it a great first-line treatment for dry-eye disease, especially in those with an aversion to eyedrops.”
“I like using the nasal spray in a lot of different patient populations,” says Dr. Meghpara. “It’s great for patients who don’t have the manual dexterity to put drops in or for contact lens users who may not be able to use certain medications while their contact lenses are in their eyes. Glaucoma patients also like Tyrvaya because it’s not another drop.”
Dr. Behshad says he doesn’t use Tyrvaya often because it’s difficult for patients to get coverage and is cost-prohibitive.
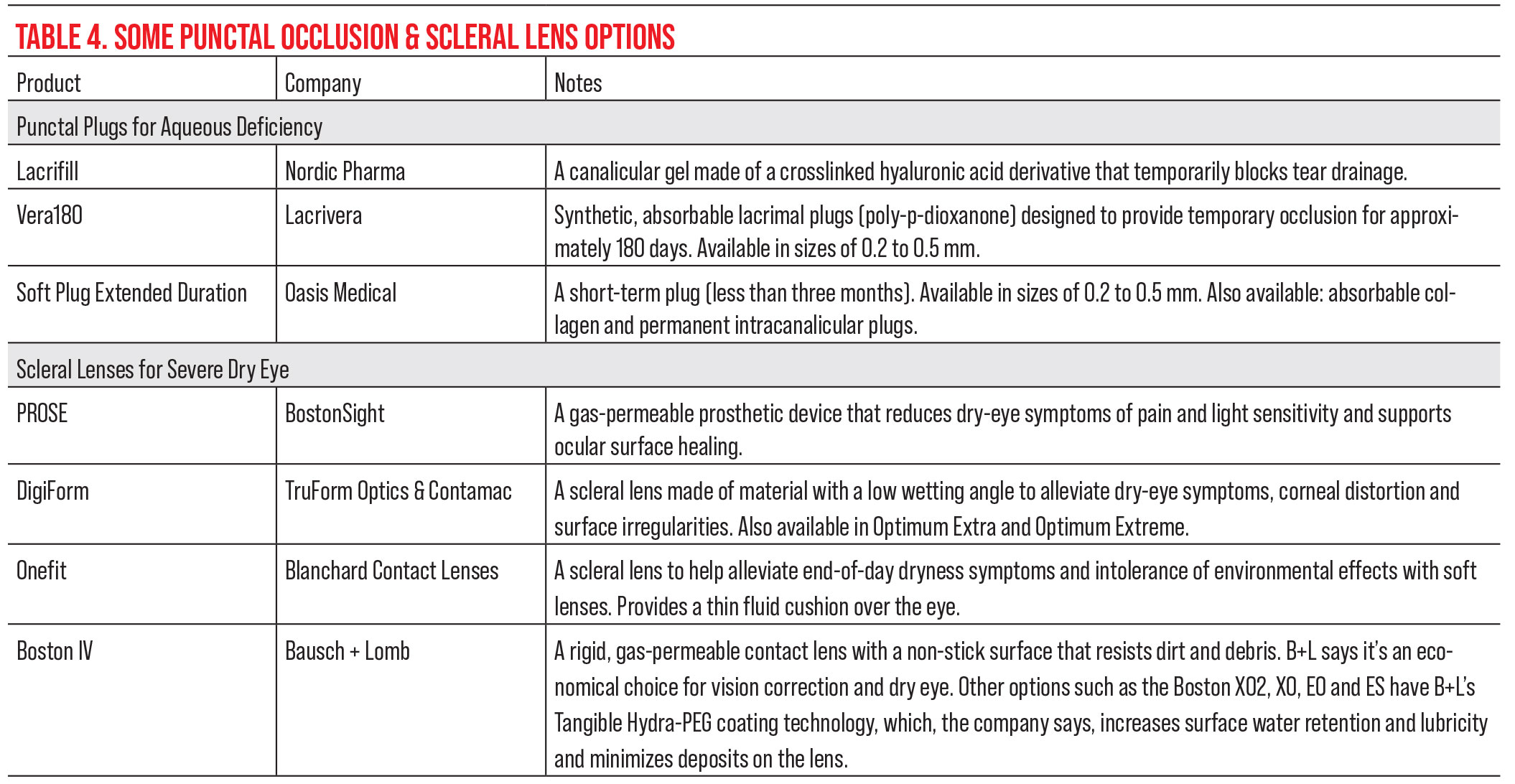
Punctal occlusion is a common approach to reducing tear outflow, often started after patients try artificial tears but need additional measures to combat dry eye. In addition to punctal plugs, clinicians can now use a cross-linked hyaluronic acid derivative canalicular gel called Lacrifill. Lacrifill molds to the patient’s canalicular system to create punctal occlusion and reduce tear outflow. Experts say it doesn’t seem to elicit as much of an inflammatory response as silicone plugs since nothing rubs on the conjunctiva or can get stuck in the ducts.
“I haven’t tried [Lacrifill] yet, but I think it could be an exciting alternative to plugs,” Dr. Lin says. “Lacrifill may be more cost-effective if used in all four puncta, because once you open it you can’t reuse it again. So, it may be best for patients who need all four puncta occluded.”
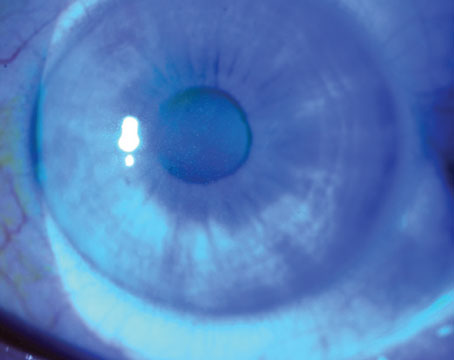
Scleral lenses are another option that can help soothe the ocular surface. “Scleral lenses can be very effective for symptoms because they are a fluid-filled reservoir that bathes the cornea constantly while the contact lens is in,” Dr. Lin says.
Might vs. Mite
Blepharitis is an umbrella term encompassing anterior and posterior subtypes and their respective signs and symptoms. For anterior blepharitis, warm compresses, daily lid scrubs and topical antibiotics can help relieve symptoms, expert say.
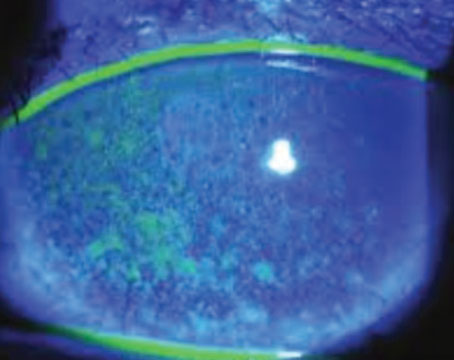
“Much of the time, when patients come in with a prior diagnosis of ‘blepharitis’ but are still suffering despite lid hygiene and warm compresses, Demodex blepharitis is the undiagnosed and untreated culprit,” Dr. Starr says. “The best way to identify that is to have the patient look down at the slit lamp and look for collarettes, cylindrical buildup of material at the base of the lashes, which is pathognomonic for Demodex blepharitis. Xdemvy, which is administered twice a day for six weeks, is a highly effective FDA-approved antiparasitic treatment for Demodex.
“Unlike some ocular surface treatments we start, such as artificial tears and immunomodulators, there’s a finite endpoint with Xdemvy for Demodex blepharitis,” he continues. “That’s new. When we put patients on cyclosporine or other immunomodulators, there’s no predefined endpoint—they’ll often need to use the medication indefinitely—but with Xdemvy, we are able to stop it at six weeks.”
 |
Along with Xdemvy, adjunctive use of microblepharoexfoliation with the BlephEx device to mechanically remove collarettes and biofilms at the lid margin is complementary and helps resolve the signs and symptoms of Demodex blepharitis faster, Dr. Starr says. “Many patients with Demodex folliculorum will also have Demodex brevis in the meibomian glands and significant MGD. Anything we can do to treat those simultaneously is an advantage. Thermal pulsation procedures like LipiFlow and light-based procedures like intense pulsed light therapy can also be effective and adjunctive to Xdemvy when Demodex is present. We know that a lot of Demodex comes from the cheeks and facial skin of patients with rosacea, and IPL can help to reduce the mite load on the skin.”
Dr. Mukhtar approaches Demodex in two ways, with a supportive approach and with Xdemvy. “The supportive way includes tea tree oil lid wipes, which are important because they sterilize the mites,” she explains. “I then ask patients to use a thick lubricating ointment such as Refresh nighttime ointment or Systane nighttime ointment on the base of their eyelashes. This suffocates the mites. They like to come out overnight. In the morning, I have patients use the lid wipes. The ointment application has two purposes: one is to suffocate the mites and the other is to ensure the patient uses the wipes in the morning, because now they have the ointment all over their eyes.”
Dr. Mukhtar points out to patients that the more conservative therapy is lifelong. “As soon as they stop, the mites will come back,” she says. “But with lotilaner, it’s basically one drop twice a day for six weeks, and studies show that the mite load is significantly decreased in all populations no matter the pre-treatment mite load. And if the mites come back, they come back at a lesser load than before treatment. Unfortunately, as a newly approved drug, cost is a huge issue for many of our patients. Secondly, we don’t yet know what the long-term side effects are.”
“Xdemvy is something that I go to as a first-line treatment for Demodex,” Dr. Meghpara says. “I don’t do blepharoexfoliation treatments like BlephEx in the office, but others do. Xdemvy by itself has shown impressive results in terms of collarette reduction. In the office, we’re seeing similar results. Patients respond really well.”
“This has been a game changer for patients with Demodex blepharitis,” says Dr. Behshad. “Prior to this we really didn’t have a great treatment option. The majority of my patients have their Demodex cleared by six weeks. I also notice improved MGD as patients continue to use this medication, which may be due to Xdemvy’s lipophilic component.”
Meibomian Gland Dysfunction
Common treatments for MGD include warm compresses, thermal pulsation treatments, mechanical expression of the glands, IPL therapy and anti-inflammatory medications. “If a patient has co-existing severe meibomian gland dysfunction, I might turn to oral doxycycline or a hypochlorous acid spray twice a day to control that,” says Dr. Lin.
Miebo (perfluorohexyloctane) was recently approved for meibomian gland disease. Dr. Starr says Miebo is used four times a day and each drop can last for several hours. “When the meibomian glands are obliterated, it’s hard to revive them, so you have to replenish the missing lipid layer,” he says. “I’ve found that Miebo is a good way of doing that and is a compelling first-line treatment in these patients.”
“Miebo coats and lubricates the ocular surface to try to restore what a normal, healthy tear film would be like,” Dr. Meghapra says, adding that this medication doesn’t really have a category yet since it’s the first of its kind. “I use Miebo for evaporative dry-eye patients who’ve failed the more common treatments such as warm compresses, or they’re on anti-inflammatory medication already and supplementing with regular artificial tears and they’re still symptomatic. That’s when I reach for Miebo.”
Dr. Behshad says that Miebo has been a great first-line agent for his evaporative dry-eye patients and those with screen time-related dry eye. “Patients note the decreased symptoms and often describe how these drops last longer than previous lubricating drops they’ve tried,” he says. “There’s a steep learning curve for patients with the bottle and proper use, however. Many comment that they feel they waste a lot and finish their supply before they’re able to get a refill.”
“I tell my patients that [Miebo] isn’t really treating any underlying cause; it’s more supportive,” Dr. Mukhtar says. “Most of my patients still really love it and continue to use it, especially those who have meibomian gland atrophy. It’s a great option.”
When to Use Serum Tears
When traditional treatments aren’t enough to relieve the signs of dry eye and patients’ persistent symptoms, autologous serum tears may hold the answers. “I’ve tried them in patients with severe symptoms without many signs of dry eye, and I’ve had variable success,” Dr. Lin says. “For severe dry eye, autologous tears are very helpful.”
“Patients go to a lab and get their blood drawn,” Dr. Meghpara says. “The red blood cells are removed and what you’re left with is serum, a straw-colored liquid that has many different components including anti-inflammatory factors, nerve growth factor and epithelial growth factor. The serum is diluted to a certain concentration of these components that mimics the normal composition of a healthy tear film. It’s a very effective treatment. The downside is the inconvenience of it, the need for a special compounding pharmacy and the fact that the cost isn’t covered by insurance.”
Dry eye caused by Sjögren’s disease is tricky to address. “Not only are patients not making enough tears, but the tears they are making are very inflammatory,” Dr. Mukhtar says. “Even though there are treatments that stimulate tear production, such as varenicline, the tears aren’t good-quality tears. Patients end up having to be on a very extensive regimen, and it’s challenging to optimize their tear film and ocular surface.
“I love serum tears for these patients,” she continues. “In the Cornea Society, opinions on serum tears for Sjögren’s are split. Some feel that if a patient has a systemic inflammatory syndrome, you shouldn’t be using serum tears. Others feel that if it’s Sjögren’s type 1, it should be fine, but if it’s Sjögren’s type 2, you shouldn’t use them. My thought process is that we can try it, and if it works, great. I give patients a lot of anticipatory guidance to help them manage expectations.”
“The most difficult types of dry eye to treat are usually dry eye secondary to something else,” Dr. Meghpara says. “Graft versus host disease is one of the worst. It can lead to rapidly progressive dry eye. We had a patient who came in with a flare of graft versus host disease and they went through a number of treatment options, starting with steroid eye drops to control their inflammation, amniotic membrane placement to help heal the cornea and then an immunomodulator for long-term control. Despite all that, the patient still had a lot of dryness and staining on the cornea. They ended up needing to go on autologous serum tears and have now been stable for years.”
Dr. Meghpara is a consultant for Allergan, Sun Pharma, BioTissue and Tarsus.
Dr. Starr is a consultant for Novartis, Allergan/Abbvie, Trukera, Sun Pharma, Bruder, BlephEx, Kala, Quidel, Dompé, Johnson & Johnson Vision, Sight Sciences, Essiri LLC., Tarsus, Oyster Point, CSI Dry Eye, Aldeyra, Alcon, Versea, Bausch + Lomb, Novaliq, Lumenis, Théa, Glaukos, Amgen, Oculis, Eye Care International, Sofia Biologics, Azura and Allgenesis.
Dr. Behshad, Dr. Lin and Dr. Mukhtar have no relevant financial disclosures.