It’s no secret that hospitals and other health-care clinics are short on personal protective equipment because of the COVID-19 pandemic. Out of necessity, organizations have now been forced to investigate different methods for sterilizing protective gear such as surgical masks that were designed and approved for single use only, thus allowing them to be used multiple times before disposal.
Because COVID-19 is an airborne pathogen, face masks such as the N-95 respirator are especially crucial for protecting health-care workers. For that reason, much attention has recently been paid to finding ways to eliminate or deactivate any virus on these masks without damaging the masks’ functionality. (In an effort to facilitate this process, the U.S. Food and Drug Administration recently granted several emergency use authorizations to allow decontamination and reuse of this type of mask.)
Methods that have been tried to date include using ultraviolet light, bleach, ethylene oxide gas, dry heat, vaporized hydrogen peroxide and even microwave radiation. (The latter was judged unsuitable early on because it damaged the masks.) Currently, the alternatives that appear most feasible are UV light and some form of vaporized hydrogen peroxide. Each can be applied in different ways, with different advantages and limitations. Here, health-care professionals share what they’ve learned from working with these two options.
Exploring the Possibilities
Robert C. Cohenour, MD, a neurologist in practice for more than 40 years in Northridge, California, is the CEO of two large, multispecialty surgical centers that are part of a series of group practices. About 45 ophthalmologists use the ophthalmological surgical center. “We’re adjacent to two hospitals in the San Fernando Valley, and part of the emergency service network in the community,” he says. “We have arrangements with those hospitals to accept overflow patients, so we’re not just doing elective cases.”
Dr. Cohenour notes that surgical centers don’t generally require N-95-grade masks. “We’re using the N-95 masks now primarily in the operating room area, and for any nurse that feels that he or she needs to have a respirator mask,” he explains. “Because of the pandemic, we’re using them more routinely, in addition to safety shields in some situations. We had to start recycling the masks because we didn’t have enough sources from which to buy them, and the cost was exorbitant, particularly at first. Luckily, a donor contributed a bunch of masks to each of our facilities.”
Once the need to reuse the N-95 masks became clear, they began investigating ways to sterilize the masks with minimum damage to the masks’ fit and filtration capacity. “We have a Sterrad sterilization system at one of our surgical centers,” he says. “It uses a combination of gas and hydrogen peroxide; it’s described as low-temperature sterilization, although it runs at about 160° Fahrenheit.
“The Sterrad system does sterilize effectively,” he continues. “However, it has several practical disadvantages if you want to use it for sterilizing disposable surgical masks like the N-95. First, the process takes several hours. Second, the time required to run the process forces us to sterilize multiple masks or other PPE at the same time, leading us to be concerned about cross-contamination. Third, the system is very expensive compared to a UV-C light system; it cost about $25,000 when we installed it. Perhaps most important, in our experience it causes more damage to the N-95 masks than sterilization using UV-C light.”
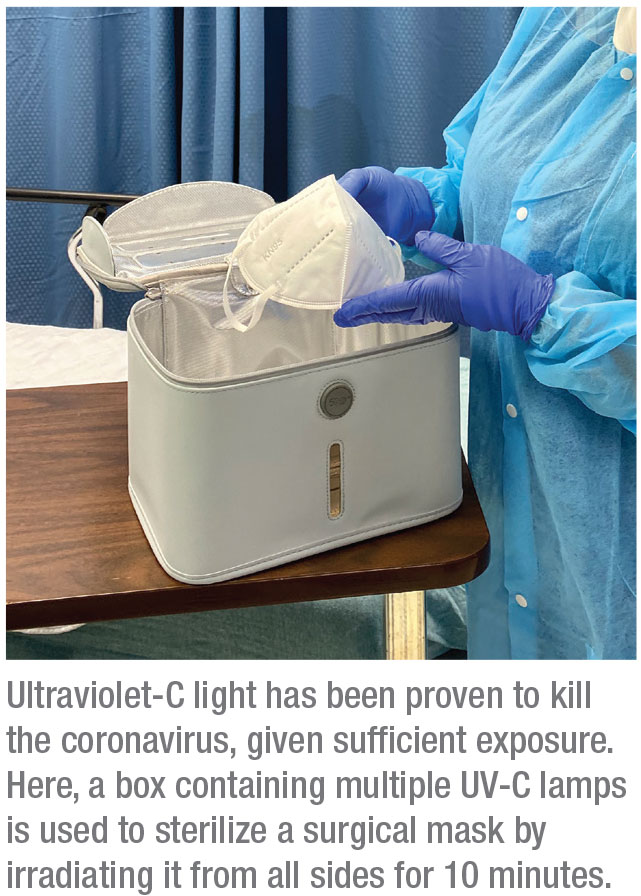
Dr. Cohenour says his practice is now using the 59S UVC-Portable UV Light Cleaner/Sterilizer Box P55 system, a small box with UV-C lights on all four of its internal sides. Masks are placed inside the box individually and irradiated for several minutes. “The multiple lights produce UV-C light throughout the container, not just on one side,” he points out. “It’s supposed to be a three-minute sterilization process, but we run it for 10 minutes as an additional safety precaution.
“The box is large enough to do five or 10 masks at once, but because it doesn’t take long and we only have 31 employees here, we can sterilize one mask at a time and still get all of the masks sterilized every day,” he continues. “The light doesn’t disrupt the respirator filter or the metal stays that help the mask conform to the user’s face.”
Dr. Cohenour says the UV-C boxes are now used in both of their ASCs. “Our process is pretty straightforward,” he says. “Everyone’s mask has his or her name and the date first sterilized written on it. At the end of the day, each mask is sterilized in the UV-C box, and then placed in a paper bag with that person’s name on it.”
Lessons from Biocontainment
Michael Hartley, emergency manager for the University of Iowa hospitals and clinics and operations manager of their special pathogens unit, is well-acquainted with the issues surrounding decontamination. “Our biocontainment unit is a pod of four isolated rooms that have their own air-handling system,” he explains. “Although the pod is secure and has all the features of a modern biocontainment facility, most days it’s used as an intensive care unit taking care of trauma victims. If we need biocontainment, the unit is quickly converted to let us care for people carrying some of the most dangerous pathogens on the planet. Once those patients have been cared for, we have to turn that unit back into normal intensive-care rooms. That means we have to make sure those rooms are as aseptic, clean and disinfected as humanly possible.”
 |
Mr. Hartley has spent a lot of time searching for the safest and most effective ways to manage this. “A few years ago I ran across a technology called SteraMist, available from Tomi Environmental Solutions (Beverly Hills, California), that sterilizes with ionized hydrogen peroxide,” he says. “Previously, we were using UV-C light for room sterilization. We’d purchased six very powerful UV robots that roll into a room and blast it with UV-C light. But we quickly realized that this approach has some limitations, given that UV light travels in a straight line; it doesn’t go around corners, so areas in shadow might not be effectively sterilized.
“I wanted something that would get into every nook and cranny of a room, without harming surfaces or objects or sensitive electronics,” he continues. “Vaporized hydrogen peroxide looked interesting to me. However, some systems using this approach include antimicrobial additives such as silver in the vapor, and that concerned me. In addition, some of them use very high-concentration hydrogen peroxide. The hydrogen peroxide you buy in a drug store is about a 3% concentration. It’s safe; you can swish it in your mouth. But some of these systems use concentrations as high as 35%. That’s a hazardous material.”
Mr. Hartley explains that the SteraMist devices position electrodes in front of a pinhole nozzle that shoots a high-pressure stream of 7.8% hydrogen peroxide. “The mist passes through a 17,000-volt cold-plasma electric arc,” he says. “When the hydrogen peroxide mist hits the arc, the hydrogen peroxide molecules are split into hydroxyl radicals made up of one hydrogen and one oxygen atom. When these radicals hit the cell wall of a mold, virus, bacteria or fungus, they oxidize and destroy the cell wall, reportedly within about three seconds.
“We brought the SteraMist system in and tested it with help from our state hygienic public health laboratory,” he continues. “It produced a six-log kill; that means more than 99.9999 percent of the spores we used as test organisms were killed. Other research we reviewed revealed no documented harm to sensitive electronic equipment or surfaces or materials. Ultimately, we bought the system for fogging the biocontainment rooms after special pathogen care.”
Sterilizing Masks with Vapor
When the current crisis arose, Mr. Hartley realized he might be able to use the same technology to make disposable items such as masks reusable. “As it turned out, the manufacturer of the SteraMist system had already developed a protocol for this for hospitals in Hong Kong,” he says. “I decided to see if we could use it to disinfect masks such as N-95s on a large scale. To do this, we borrowed some logistical ideas from our friends at the University of Nebraska, who were already trying this using UV-C light.
“We had to be sure this process would work without harming the masks or reducing their ability to filter,” he continues. “Working with a neighboring NIOSH-funded environmental health and safety laboratory on our campus, we were able to test the masks after treatment. The tests showed that the treatment caused negligible filtering degradation. However, the lab said we shouldn’t use the process on a mask more than three or four times.
“It turned out there was a reason for this,” he explains. “Many people don’t realize that a key reason N-95 masks are so effective is that the material has an electrostatic charge, just like some furnace filters you can buy. When air is passing through the mask, it’s filtered not only by the size of the holes through which it passes, but also by the electrostatic charge pulling particles out of the air. Because of that, the mask can be just as effective as a heavier mask, without being as thick. That makes them easier to breathe through than, for example, a homemade mask.
“This turned out to be relevant, because the SteraMist system ionizes the hydrogen peroxide by passing the mist through a powerful 17,000-volt electric arc,” he says. “We realized that might be affecting the electrostatic charge of the mask material. So, we put greater distance between the device and the masks, and it made a difference; now we’re able to sterilize the masks six times without noticeable degradation. Although we can’t prove it, we hypothesize that the revised protocol doesn’t interfere with the electrostatic charge of the mask.”
 |
Practical Considerations
Mr. Hartley explains that when they spray masks with the mist or fog, the sterilizing effect is basically instantaneous. “However, the masks are then moist,” he notes. “They have to dry a little bit. We dry them in a special room that has a lot of air exchange, and the evaporating hydrogen peroxide is then vented to the outside. This takes about 20 minutes, so the entire process takes 45 minutes to an hour.
“With the current system we can do at least 1,200 masks a day,” he says. “This allows us to get people’s masks back to them the same day or the next day. We’ve done thousands, and we haven’t reached our full processing capability yet.”
Mr. Hartley admits that one practical problem with the SteraMist system is that it’s relatively expensive. “Most of the vaporized hydrogen peroxide technologies out there have a pretty steep price tag,” he says. “That’s a problem right now because money is tight as a result of the crisis. That’s why I think most hospitals are trying to find ways to sterilize masks using whatever sterilization technology they already have in-house. Some are trying to use the same sterilizers they use for surgical instruments; protocols have been developed for that. Many hospitals have already been using UV-C room-disinfecting devices, and you can purchase small devices that sterilize with UV-C light that are less expensive.”
Mr. Hartley says he’s published papers about using UV-C light sterilization, so he knows that it works against coronavirus. “My only concern is that you have to make sure the light is getting all the way through any folds or convolutions in the mask,” he says. “With a soft, porous, fibrous surface, that can be tricky. Our colleagues in Nebraska have come up with a good process using UV-C light; they use two light devices instead of one, and they shine intense light on both the inside and outside of the masks. Hitting it from both sides with an excessive dose of light is probably the best way to use this strategy.”
Mr. Hartley points out a helpful website that collates a lot of information about the sterilizing options. “Our protocol has been posted on the website N95decon.org,” he says. “That’s run by a not-for-profit consortium of medical professionals and academics who’ve looked at all the different ways people are trying to decontaminate PPE. They give a pretty nonbiased synopsis of all of the methods. They want to help people figure out how to accomplish this with whatever equipment they already have.”
What’s Next?
Given that constantly using and throwing away disposable, single-use items is arguably wasteful and harmful to the environment, it seems reasonable to wonder whether health care will return to that modality after the crisis ends. “If we can safely reprocess these one-time-use items, that’s logical during this crisis,” notes Mr. Hartley. “However, I suspect that when the crisis is over we’ll probably go back to using disposable equipment.
“In the past, hospitals used surgical gowns that could be laundered,” he recalls. “After each use they’d be laundered and sterilized and repackaged. The problem is, that’s a fairly expensive process compared to using cheap disposal gowns. It’s ironic that a large percentage of the disposable PPE is made in China and Asia where the outbreak started. It’s a worst-case scenario. Having an outbreak like this will interfere with the supply chain of the inexpensive things that we rely on, and that could have a big impact on what happens after the crisis ends.
“So, I don’t know if we’ll return to the disposable system after this ends,” he concludes. “Yes, cheap, disposable PPE is arguably wasteful. But if the cheap disposable stuff is back on the market and readily available, it may be too convenient to resist.” REVIEW
Mr. Hartley and Dr. Cohenour have no financial ties or relationships with any technology discussed in this article. You can learn more about the SteraMist technology by visiting tomimist.com.



