The large-scale, retrospective, consecutive case series included more than 13,500 patients undergoing elective office-based cataract surgery performed in minor procedure rooms (MPRs) of Kaiser Permanente health-care centers in Colorado.
Office-based cataract surgery was completed in 21,501 eyes (13,507 patients, age 72.6 ±9.6 years). Phacoemulsification was performed in 99.9 percent of cases, and manual extracapsular extraction was performed in 0.1 percent of cases. Systemic comorbidities included hypertension (53.5 percent), diabetes (22.3 percent) and chronic obstructive pulmonary disease (9.4 percent). Postoperative mean best-corrected visual acuity measured 0.14 ±0.26 logarithm of the minimum angle of resolution units. Intraoperative ocular AEs included 119 (0.55 percent) cases of capsular tear and 73 (0.34 percent) cases of vitreous loss. Postoperative AEs included iritis (n=330, 1.53 percent), corneal edema (n=110, 0.53 percent) and retinal tear or detachment (n=30, 0.14 percent). No endophthalmitis was reported. Second surgeries were performed in 0.70 percent of treated eyes within six months. There were no life- or vision-threatening intraoperative or perioperative AEs.
Ophthalmology 2016;123:723-8.
Ianchulev T, Litoff D, Ellinger D, Stiverson K, Packer M.
Five-Year Results of Four DME Treatment Options Compared
Researchers from the Wilmer Eye Institute, Baltimore, and several southeastern U.S. health centers compared long-term vision and anatomic effects of ranibizumab with prompt or deferred laser versus laser or triamcinolone + laser with very deferred ranibizumab in diabetic macular edema.
In their trial, 828 eyes with visual acuity 20/32 to 20/320 and DME involving the central macula were randomly assigned to intravitreous ranibizumab (0.5 mg) with either 1) prompt or 2) deferred laser; 3) sham injection + prompt laser; or 4) intravitreous triamcinolone (4 mg) + prompt laser. The latter two groups could initiate ranibizumab as early as 74 weeks from baseline, for persistent DME with vision impairment. The main outcome measures were visual acuity, optical coherence central subfield thickness, and number of injections through five years; 558 (67 percent) completed the five-year visit.
 |
At five years mean (± standard deviation) change in Early Treatment Diabetic Retinopathy Study visual acuity letter scores from baseline were: 10 ±13 letters in the ranibizumab + deferred laser group (n=111); 8 ±13 in the ranibizumab + prompt laser group (n=124); 5 ±14 in the laser/very deferred ranibizumab group (n=198); and 5 ±14 in the triamcinolone + laser/very deferred ranibizumab group(n=125). The difference (95 percent confidence interval) in mean change between ranibizumab + deferred laser and laser/very deferred ranibizumab and triamcinolone + laser/very deferred ranibizumab was 4.4 (1.2 to 7.6, p=.001) and 2.8 (-0.9 to 6.5, p=.067), respectively, at five years.
The authors recognize the limitations of follow-up available at five years, but conclude that eyes receiving initial ranibizumab therapy for center-involving DME likely have better long-term vision improvements than eyes managed with laser or triamcinolone + laser followed by very deferred ranibizumab for persistent thickening and vision impairment.
Am J Ophthalmol 2016 Apr;164:57-68.
Bressler SB, Glassman AR, Almukhtar T, Bressler NM, Ferris FL, Googe JM Jr, Gupta SK, Jampol LM, Melia M, Wells JA 3rd; Diabetic Retinopathy Clinical Research Network (DRCR.net).
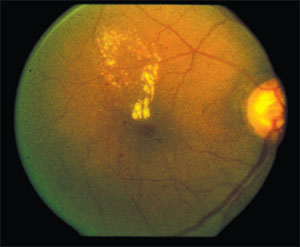
More Data on Sunlight, AMD
Researchers in Cologne, Germany, and Nijmegan, the Netherlands evaluated the effects of current and past sunlight exposure and iris color on early and late age-related macular degeneration. Previous studies, they note, suggested a connection between sunlight exposure and light iris color and greater risk for AMD, but with inconsistent results.
They reviewed 3,701 casers from the EUGENDA database; 752 (20.3 percent) showed early AMD; 1,179 (31.9 percent) late AMD; and 1,770 (47.8 percent) were controls. Information about current and past sunlight exposure, former occupation type, subdivided in indoor working and outdoor working, and iris color were obtained by standardized interviewer-assisted questionnaires. Associations between environmental factors adjusted for age, gender, and smoking and early and late AMD were performed by multivariate regression analysis.
Current sunlight exposure showed no association with early AMD or late AMD, but past sunlight exposure (≥eight hours outside daily) was significantly associated with early AMD (odds ratio: 5.54, 95 percent confidence interval 1.25 to 24.58, p=0.02) and late AMD (odds ratio: 2.77, 95 percent CI 1.25 to 6.16, p= 0.01). Outside working was found to be associated with late AMD (odds ratio: 2.57, 95 percent confidence interval 1.89 to 3.48, p=1.58 × 10). No association was observed between iris color and early or late AMD.
Sunlight exposure during working life is an important risk factor for AMD, they conclude, whereas sunlight exposure after retirement seems to have less influence on the disease development. Therefore, preventive measures such as wearing sunglasses to minimize sunlight exposure should start early to prevent development of AMD later in life.
Retina. 2016;36:787-90.
Schick T1, Ersoy L, Lechanteur YT, Saksens NT, Hoyng CB, den Hollander AI, Kirchhof B, Fauser S.



