Other Procedures Catch On
"For the first time in the survey, phakic IOLs surpassed LASIK for a 30-year-old, 10-D myope," says Dr. Duffey. Twenty-seven percent of respondents say they'd prefer a lens for this type of patient, vs. 20 percent who would do LASIK. The single most popular option is waiting, at 35 percent. "As you get into the higher degrees of myopia, where there's a risk of ectasia from ablating too much corneal tissue, a phakic IOL probably becomes the safer option. Now, you're working on the inside of the eye, so you have a risk of retinal detachment, endophthalmitis, et cetera, but I think the trend will be for more people to go toward the phakic IOLs for the 10-D myope."
Four years ago LASIK was the predominant choice for the 45-year-old 3-D hyperope with 70 percent of the surgeons choosing it. That rate has dwindled to 45 percent in the latest survey. On the other hand, refractive lens exchange, at just below 10 percent in 2003 as the choice for the 3-D hyperope, is now up to 22 percent. "I'm kind of in the RLE category," says Dr. Duffey. "For a 45-year-old, it's a little bit of a tough call, because you're going to make him presbyopic with a refractive lens exchange, and you don't like to do that. But now that we have multifocal IOLs such as the ReSTOR and ReZoom, in my practice you'll see this type of patient getting a multifocal lens, while in the past I'd almost always have done LASIK."
In terms of sheer volume, surface procedures, specifically LASEK and epi-LASIK, have made great strides. In last year's survey, the respondents reported doing only about 45,000 cases of LASEK or epi-LASIK. This year, however, the number has jumped to 200,000 cases, accompanied by a decrease in LASIK volume from 930,000 to 860,000. PRK accounted for 150,000 procedures. "The bottom line is, we're seeing more surface ablation, and this is the first year where the data has pretty much supported that," says Dr. Duffey, who finds himself doing more surface procedures. "Today, if anyone has a funny topography I just tell him, 'In the past, I'd do LASIK on this, but I'm not going to do it anymore. We've got surface ablation techniques that work very well, but take a little bit longer to heal. But, when all is said and done, they will be safer for you.' "
Despite the surge of interest in diffractive and multifocal intraocular lenses for the presbyope, the most popular single surgical option for presbyopia is still monovision, being chosen by 39 percent of respondents. ReSTOR is preferred by 20 percent, ReZoom by 8 percent and the Crystalens by 4 percent. "It's interesting to me that monovision still wins out," muses Dr. Duffey. "But I think you'll see those ReSTOR and ReZoom numbers continue to climb. And, if we get a truly accommodative IOL, something that's an improvement over the Crystalens, I think you'll see the number of surgeons choosing an accommodative IOL increase as well." He says monovision is still tops because "a lot of people come in having done monovision with their contact lenses, and it's the least expensive modality."
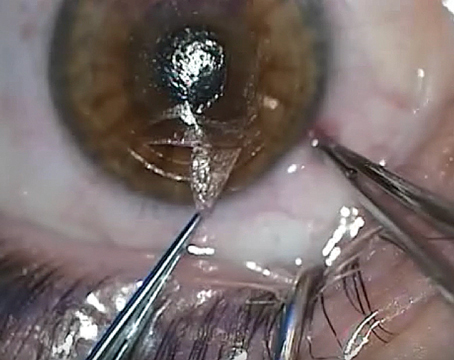
Flap Thickness and Ectasia
The fear of ectasia may be causing surgeons to perform more surface ablation or use thinner flaps, but Dr. Duffey says there's a glaring omission in the way surgeons try to minimize their ectasia risk.
"It still amazes me—intraoperatively measuring flap thickness is the simplest way we have to assure ourselves that we're not violating the 250-µm or 300–µm rule of leaving enough corneal tissue in the stromal bed to prevent ectasia, and yet 72 percent of us don't do it," he says. 
In terms of surgeons' preferred flap thickness, Dr. Duffey was surprised more surgeons aren't going for thinner flaps; 16 percent say 100 µm is their preferred thickness, 46 percent prefer 120 to 130 µm and 29 percent prefer 150 to 160 µm, with smaller numbers of outliers preferring thinner or thicker flaps than these ranges. "I thought more people would go to thinner flaps, because they're being pushed by Intralase, but only 16 percent prefer them," he says. Dr. Duffey says he routinely cuts 100-µm flaps with his LSK-One microkeratome. Sixty-one percent of surgeons say 250 µm is their minimum residual bed thickness, 21 percent prefer 275 µm and 13 percent like 300 µm.
As for the incidence of ectasia, the study extrapolated that it's about 1:11,500 cases. "I think we underestimate though, because people tend to underreport," says Dr. Duffey. "Personally, that number is pretty solidly scientific, but I'd be willing to bet it's more like 1:6,250; I think the numerator's higher and the denominator's lower."
Other Results
The questionnaire also turned up interesting findings in other surgical areas:
• Surgeons are becoming more comfortable with using mitomycin-c with their surface procedures. Last year, about 54 percent used it for treating or preventing haze; it's jumped to 67 percent this year. Those who never use it fell from 36 percent to 25 percent.
• Wavefront ablations are more common now than ever. Last year, 26 percent of surgeons said they never used them; just 10 percent say so in the current survey.
• Twenty-seven percent of the surgeons say they've had refractive surgery themselves, which Dr. Duffey says is four times the penetration rate of the general population. "In other words, the people that know the most about modern refractive surgery are having it done," says Dr. Duffey. "This isn't because it's cheaper for them. I think it's more the fact that they see all the surgeries and the patients and know that well-done refractive surgeries by good surgeons using good equipment on good candidates perform very well."