When patients ask about this, I tell them that there are quite a few lifestyle choices that may impact the development and/or modify the progression of glaucoma for better or worse. Below, I have listed a number of pro and con factors you might wish to share with your patients, when appropriate. (Of course, elevated IOP is the major known risk factor for glaucoma, so that’s the easiest issue to address; a number of the lifestyle choices listed below interact with the progression of glaucoma either by potentially raising or lowering IOP.)
Exercise and Glaucoma
If you want to decrease your IOP, aerobic exercise may help (although it’s important to make sure that any patient with cardiac issues has this activity approved by his cardiologist). Some of the relevant data:
• One study found that in non-smoking, healthy volunteers, aerobic exercise increased heart rate and systolic blood pressure while decreasing IOP and diastolic blood pressure.1
• A study of active college-age students found that dynamic resistance exercises lowered IOP.2
• A study of 20 young adult subjects found that IOP (as well as ocular pulse amplitude and axial length) decreased significantly after exercise (p<0.0001)3
• A study of 67 healthy patients under the age of 40 compared the impact of isometric and isokinetic exercises on IOP. Both types of exercise lowered IOP in direct proportion to exercise intensity, but the pressure-lowering effect of isokinetic exercise was more significant.4
The data is mixed regarding weightlifting. Some studies suggest that weightlifting may trigger the equivalent of the Valsalva maneuver, thereby raising IOP. On the other hand, the lifestyle consequences of exercise are generally positive, and weightlifting certainly is a form of exercise. (It’s worth noting one of the big problems with research into these possible associations: Most of these studies were done in young, healthy subjects, not in glaucoma patients.)
It is difficult to arrive at a clear conclusion regarding related considerations such as body mass index and its relation to glaucoma. For example, published data shows a positive relationship between BMI and IOP, but an inverse relationship between BMI and glaucoma.5,6
Of course, lifestyle choices, including exercise, can also play an important role in cardiac health, and there’s considerable evidence that cardiac health influences the development of glaucoma.7-12 Among other things, altered ocular blood flow may be a major factor in the pathogenesis of glaucomatous optic neuropathy.
Activities & Habits
• Cigarette smoking. I believe a majority of physicians agree that smoking has few, if any, health-related benefits, and may cause serious harm. In terms of glaucoma, one meta-analysis concluded that smokers are at a significantly increased risk of developing open-angle glaucoma13 but another study published in 2003 found no increased risk of glaucoma in smokers.14 On the other hand, cigarette smoking has been linked to macular degeneration and cataract, and in some studies it has been associated with modest IOP elevation.15
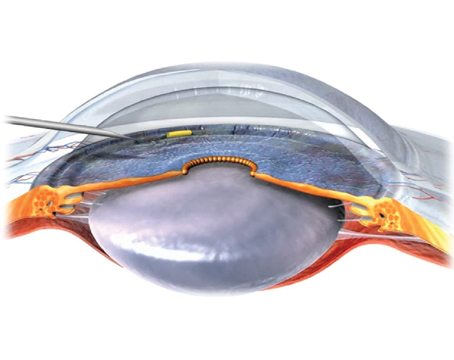
• Practicing yoga. I have encountered a number of patients with worsening glaucoma who, when questioned, explained that in an attempt to improve their overall health they had taken up practicing yoga.
|
Most people don’t realize that head-down positions (in yoga or with other activities) are generally bad for their glaucoma—and doctors seldom think to ask whether their patients are practicing these activities.
• Playing high-resistance wind instruments. In 2000, Joel S. Schuman, MD, and colleagues reported that musicians who play high-resistance wind instruments such as trumpet and oboe appear to be at increased risk of glaucomatous damage.17 The study found that IOP rose in proportion to the force of blowing, and total life hours of playing high-resistance wind instruments was significantly related to abnormal visual fields (p=0.03) and corrected pattern standard deviation scores (p=0.007). In fact, the latter increased by 0.011 units for every 1,000 hours of playing. (The authors of the study note that the resulting damage could be misdiagnosed as normal-tension glaucoma.)
• Wearing tight neckties. Even in today’s increasingly casual workplace, many men still wear neckties. Wearing them too tight can lead to prolonged periods of elevated IOP.18
Dietary Choices
• Omega fats in the diet. While many general health studies suggest that omega-3 fatty acids may be better for us than omega-6 fatty acids, at least one study suggests that this may not be the case in relation to glaucoma. It found that a high ratio of omega-3 to omega-6 fatty acids in our diet may be associated with an increased risk of POAG, especially high-tension POAG.19 (A theory to explain a possible mechanism for this result has also been proposed.20)
• Alcohol consumption. Some evidence suggests that drinking a modest amount of alcohol may lower IOP a small degree (i.e., 1 mm).21,22 However, I don’t want to encourage alcohol consumption since the evidence is not clear cut. So if asked, I usually just tell patients that alcohol doesn’t have much effect on IOP. A majority of patients often believe the opposite; they think that consuming alcohol excessively may increase their IOP, and if they stop drinking alcohol their eye pressures will suddenly become much lower. This does not appear to be the case.
• Caffeine consumption. I tell my patients that a little coffee is fine; however, loading up on caffeinated coffee is not ideal for their glaucoma. Data from the Blue Mountains Eye Study showed that subjects with open-angle glaucoma who reported regular coffee drinking had significantly higher mean IOP than subjects who said they didn’t drink coffee (p=0.03). However, the association between coffee consumption and elevated IOP was not found in those with ocular hypertension or no open-angle glaucoma at all.23 In addition, Louis R. Pasquale, MD, and colleagues observed a positive association between heavier coffee consumption and increased risk of exfoliation glaucoma or becoming an exfoliation glaucoma suspect.24 Given this data, I tell my glaucoma patients that it’s probably not a good idea to routinely order a large double espresso.
• Magnesium. Several published papers have suggested that an adequate intake of dietary magnesium may be beneficial for patients with glaucoma; it appears that a deficiency interferes with a number of ocular processes.9,25,26 However, the Rotterdam Study, using data from 3,502 participants, suggested that a high intake of magnesium may be associated with an increased risk of open-angle glaucoma.27
• Ginkgo biloba. The use of ginkgo biloba is very controversial. When I visited South Korea recently, I was told by a glaucoma specialist that up to three-quarters of patients with normal-pressure glaucoma may be prescribed this supplement in addition to their IOP-lowering medications. (That’s anecdotal; I’m not aware of any reported data backing up that claim.) Nevertheless, studies have indeed found potential neuroprotection benefits from ginkgo;28 possible effects on blood flow;29 and short-term visual field improvements in patients with normal-tension glaucoma.30
In terms of other dietary factors, it’s quite difficult to separate truth from fiction. Some papers have suggested that consumables that reduce oxidative stress may be protective. These may include dark chocolate, ubiquinone, melatonin, bilberries (because of their anthocyanosides) and tea, coffee and red wine (because of their polyphenolic flavonoids).9,31 Anti-oxidants as a group have not shown a definitive risk impact on open-angle glaucoma.32
Other Health-related Issues
• Antihypertensive drugs at bedtime. Many elderly patients take antihypertensive drugs, but lowering blood pressure excessively at night can lead to a hypotensive crisis; blood pressure can dip too low to support ocular perfusion. If your glaucoma patient is taking this type of drug, he should talk to his internist to make sure he’s not becoming too hypotensive at night.
• Sleep apnea. Studies have shown that moderate to severe obstructive sleep apnea is linked to increased risk of glaucoma development and progression.33 If a patient is aware of snoring a lot at night and/or complains of being tired all the time, it’s worth suggesting that the patient talk to his or her internist about this possibility.
A potential downside here is that one of the ways of addressing sleep apnea is to have the patient use a continuous positive airway pressure machine at night. While it is often an effective non-surgical treatment for sleep apnea, CPAP therapy was recently shown to increase IOP, especially at night,34 so it’s important to consider whether the benefits of CPAP therapy will be worth its potential downside.
• Migraines. If one of your patients complains of migraine headaches, make sure the patient is discussing this issue with an internist/neurologist. Migraines can increase the risk of progression in patients who have normal-tension glaucoma.35
• Marijuana. While smoking marijuana has been demonstrated to lower IOP in both normal individuals and in those with glaucoma, its short duration of action (only three to four hours) and its deleterious mood-altering effects are less-widely appreciated, as noted in the American Glaucoma Society’s position statement on this topic.36
There is also the real possibility that marijuana’s systemic effect of lowering blood pressure might prove deleterious to the optic nerve in glaucoma by compromising blood flow. Thus, the AGS position statement concludes, “Although marijuana can lower the intraocular pressure, its side effects and short duration of action, coupled with a lack of evidence that its use alters the course of glaucoma, preclude recommending this drug in any form for the treatment of glaucoma at the present time.” (The position statement can also be viewed on the AGS website at http://www.americanglaucomasociety.net/professionals/policy_statements/marijuana_glaucoma.)
Empowering Your Patients
Given this information, when patients ask what they can do on their own to minimize their chances of losing vision from glaucoma, I advise them to: Do some aerobic exercise; limit cigarette smoking; try to eat a diet high in antioxidants and low in fat; avoid excessive caffeine; avoid head-down positions, especially if doing yoga; and consider taking a magnesium supplement (if they’re not already taking one). I also ask whether they wear a necktie; play a wind instrument; take antihypertensive medications; have any symptoms that might indicate sleep apnea; or have a problem with migraines.
One of the worst parts of having a disease like glaucoma is feeling that you’re relatively powerless against it. Giving our patients some knowledge about lifestyle factors like the ones outlined above can help empower them—and that can improve their quality of life immediately. REVIEW
Dr. Tsai is the Delafield-Rodgers Professor and chair of the Department of Ophthalmology at the Icahn School of Medicine at Mount Sinai. He also serves as president of the New York Eye and Ear Infirmary of Mount Sinai.
1. Schmidt KG, Mittag TW, Pavlovic S, Hessemer V. Influence of physical exercise and nifedipine on ocular pulse amplitude. Graefes Arch Clin Exp Ophthalmol 1996;234:8:527-32.
2. Chromiak JA, Abadie BR, Braswell RA, Koh YS, Chilek DR. Resistance training exercises acutely reduce intraocular pressure in physically active men and women. J Strength Cond Res 2003;17:4:715-20.
3. Read SA, Collins MJ. The short-term influence of exercise on axial length and intraocular pressure. Eye (Lond) 2011;25:6:767-74. doi: 10.1038/eye.2011.54.
4. Avunduk AM, Yilmaz B, Sahin N, Kapicioglu Z, Dayanir V. The comparison of intraocular pressure reductions after isometric and isokinetic exercises in normal individuals. Ophthalmologica 1999;213:5:290-4.
5. Mori K, Ando F, Nomura H, Sato Y, Shimokata H. Relationship between intraocular pressure and obesity in Japan. Int J Epid 2000;29:4:661-66.
6. Gasser P, Stümpfig D, Schötzau A, Ackermann-Liebrich U, Flammer J. Body mass index in glaucoma. J Glaucoma 1999;8:1:8-11.
7. Grieshaber MC, Flammer J. Blood flow in glaucoma. Curr Opin Ophthalmol 2005;16:79-83.
8. Feke GT, Pasquale LR. Retinal blood flow response to posture change in glaucoma patients compared with healthy subjects. Ophthalmology 2008;115:246-52.
9. Mozaffarieh M, Flammer J. A novel perspective on natural therapeutic approaches in glaucoma therapy. Expert Opin Emerg Drugs 2007;12:2:195–198. doi: 10.1517/14728214.12.2.195.
10. Liu Q, Ju WK, et al. Oxidative stress is an early event in hydrostatic pressure induced retinal ganglion cell damage. Invest Ophthalmol Vis Sci 2007;48:4580-89.
11. Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B, BESs Study Group. Risk factors for incident open-angle glaucoma: the Barbados Eye Studies. Ophthalmology 2008;115:1:85-93.
12. Leske MC, Heijl A, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophth 2007;114:1965-72.
13. Bonovas S, Filioussi K, et al. Epidemiological association between cigarette smoking and primary open-angle glaucoma. Arch Ophthalmol 2003;121:1762-68.
14. Kang JH, Pasquale LR, Rosner BA, Willett WC, Egan KM, Faberowski N, Hankinson SE. Prospective study of cigarette smoking and the risk of primary open-angle glaucoma. Arch Ophthalmol 2003;121:12:1762-8.
15. Pasquale LR, Kang JH. Lifestyle, nutrition, and glaucoma. J Glaucoma 2009;18:6:423-8.
16. Baskaran M, Raman K, Ramani KK, Roy J, Vijaya L, Badrinath SS. Intraocular pressure changes and ocular biometry during Sirsasana (headstand posture) in yoga practitioners. Ophthalmology 2006;113:8:1327-32. Epub 2006 Jun 27.
17. Schuman JS, Massicotte EC, Connolly S, Hertzmark E, Mukherji B, Kunen MZ. Increased intraocular pressure and visual field defects in high resistance wind instrument players. Ophthalmology 2000;107:1:127-33.
18. Teng C, Gurses-Ozden R, Liebmann JM, Tello C, Ritch R. Effect of a tight necktie on intraocular pressure. Br J Ophthalmol 2003;87:8:946-8.
19. Kang JH, Pasquale LR, Willett WC, Rosner BA, Egan KM, Faberowski N, Hankinson SE. Dietary fat consumption and primary open-angle glaucoma. Am J Clin Nutr 2004;79:5:755-64.
20. Desmettre T, Rouland JF. Hypothesis on the role of nutritional factors in ocular hypertension and glaucoma. [Article in French] J Fr Ophthalmol 2005;28:3:312-6.
21. Peczon JD, Grant WM. Sedatives, stimulants, and intraocular pressure in glaucoma. Arch Ophthalmol 1964;72:178-88.
22. Kang JH, Willett WC, Rosner BA, Hankinson SE, Pasquale LR. Prospective study of alcohol consumption and the risk of primary open-angle glaucoma. Ophthalmic Epidemiol 2007;14:3:141-7.
23. Chandrasekaran S, Rochtchina E, Mitchell P. Effects of caffeine on intraocular pressure: the Blue Mountains Eye Study. J Glaucoma 2005;14:6:504-7.
24. Pasquale LR, Wiggs JL, Willett WC, Kang JH. The relationship between caffeine and coffee consumption and exfoliation glaucoma or glaucoma suspect: A prospective study in two cohorts. Invest Ophthalmol Vis Sci 2012;53:6427-33.
25. Aydin B, Onol M, Hondur A, Kaya MG, Ozdemir H, Cengel A, Hasanreisoglu B. The effect of oral magnesium therapy on visual field and ocular blood flow in normotensive glaucoma. Eur J Ophthalmol 2010;20:1:131-5.
26. Gaspar AZ, Gasser P, Flammer J. The influence of magnesium on visual field and peripheral vasospasm in glaucoma. Ophthalmologica 1995;209:1:11-3.
27. Ramdas WD, Wolfs RC, Kiefte-de Jong JC, Hofman A, de Jong PT, Vingerling JR, Jansonius NM. Nutrient intake and risk of open-angle glaucoma: The Rotterdam Study. Eur J Epidemiol 2012;27:5:385-93. doi: 10.1007/s10654-012-9672-z.
28. Ahlemeyer B, Krieglstein J. Neuroprotective effects of Ginkgo biloba extract. Cell Mol Life Sci 2003;60:9:1779-92.
29. Wimpissinger B, Berisha F, Garhoefer G, Polak K, Schmetterer L. Influence of Ginkgo biloba on ocular blood flow. Acta Ophthalmol Scand 2007;85:4:445-9.
30. Quaranta L, Bettelli S, Uva MG, Semeraro F, Turano R, Gandolfo E. Effect of Ginkgo biloba extract on preexisting visual field damage in normal tension glaucoma. Ophthalmology 2003;110:2:359-62.
31. Mozaffarieh M, Fraenkl S, Konieczka K, Flammer J. Targeted preventive measures and advanced approaches in personalised treatment of glaucoma neuropathy. EPMA J 2010;1:2:229-35. doi: 10.1007/s13167-010-0018-1.
32. Kang JH, Pasquale LR, Willett W, Rosner B, Egan KM, Faberowski N, Hankinson SE. Antioxidant intake and primary open-angle glaucoma: A prospective study. Am J Epidemiol 2003;158:4:337-46.
33. Hashim SP, Al Mansouri FA, Farouk M, Al Hashemi AA, Singh R. Prevalence of glaucoma in patients with moderate to severe obstructive sleep apnea: ocular morbidity and outcomes in a 3 year follow-up study. Eye (Lond) 2014;28:11:1304-9. doi: 10.1038/eye.2014.195.
34. Kiekens S, De Groot V, Coeckelbergh T, et al. Continuous positive airway pressure therapy is associated with an increase in intraocular pressure in obstructive sleep apnea. Invest Ophthalmol Vis Sci 2008;49:934-40.
35. Drance S, Anderson DR, Schulzer M. Collaborative Normal-Tension Glaucoma Study Group. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol 2001;131:699-708.
36. Jampel H. American glaucoma society position statement: Marijuana and the treatment of glaucoma. J Glaucoma 2010;19:75-6.