According to our most recent survey of cataract surgeons, new technology like femtosecond cataract surgery is leveling out, while new techniques like the Yamane suturing technique are taking off. Surgeons also say toric intraocular lenses are tops when tackling cylinder, topical drops still rule for postop inflammation/infection control, and quadrant division is best for nucleofractis.
This month, 1,698 surgeons of the 11,524 who received the survey opened it (14.7 percent open rate) and, of those, 89 completed the survey. Read on to see how your approach compares to theirs.
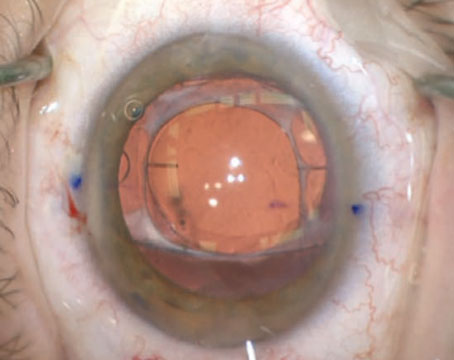
Managing Astigmatism
The surgeons say that toric IOLs are their preferred method for treating pre-existing astigmatism in their cataract patients, with this option chosen by 56 percent of the respondents. The next most popular option is a toric lens combined with placing the entry wound on the steep axis (15 percent). Manual limbal relaxing incisions were chosen by 8 percent. The remaining options were chosen by less than 8 percent of surgeons.
 |
“[Toric IOLs have a] broad range of astigmatism correction and are very accurate,” says ASCRS President Nick Mamalis, MD, of Salt Lake City. “It doesn’t affect the cornea.” Another surgeon agrees, saying that he prefers a toric lens because of “Predictability and less need for corneal manipulation.”
A surgeon from Iowa says that toric IOLs are ideal because of their “Consistently best results—a surgeon can use femtosecond or manual LRIs for smaller amounts of astigmatism not requiring a toric IOL.”
Bernard Milstein, MD, of Houston, says he prefers to use a toric lens because you can “supplement it with a postop LASIK procedure; this is more predictable.”
For the surgeons who prefer to both insert a toric lens and also make their entry wounds on the steep axis, they prefer that approach for similar reasons.
“This approach works best in most cases and is the least invasive technique,” says George Walters, MD, of Beaumont, Texas. Charles Ahn, MD, of Lombard, Illinois, likes this technique due to the “better patient payment and comfort.”
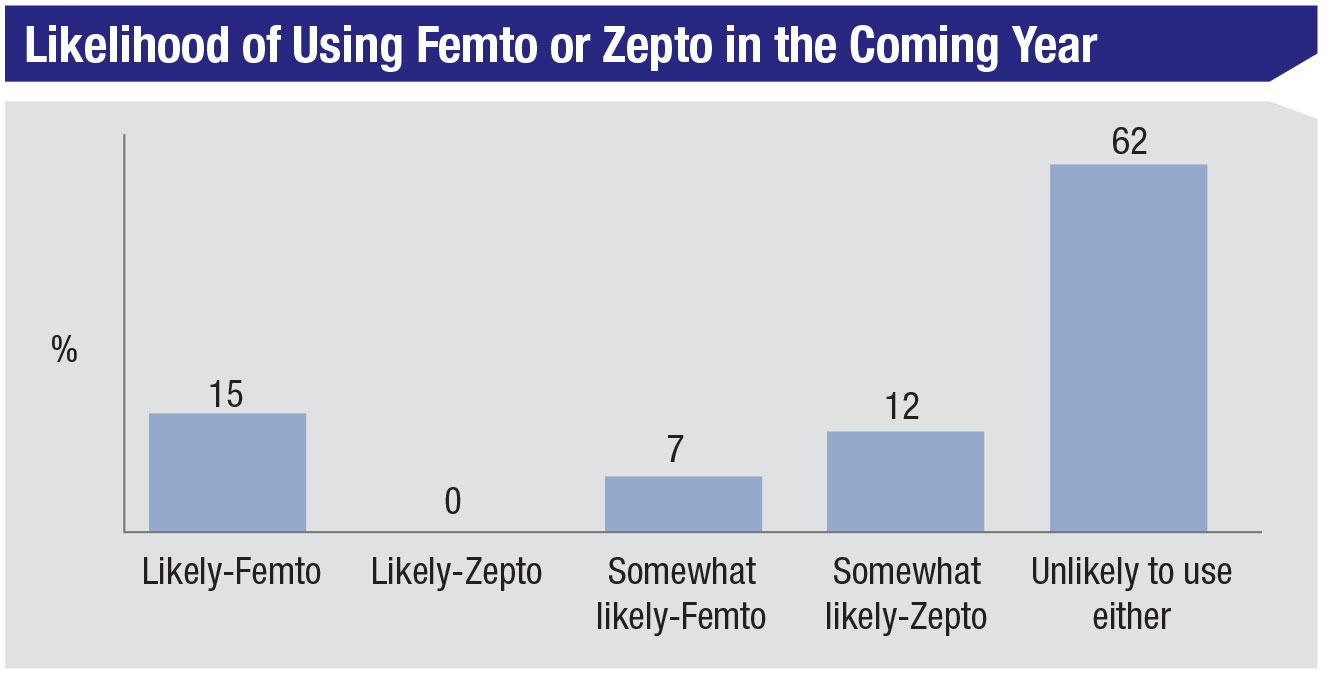 |
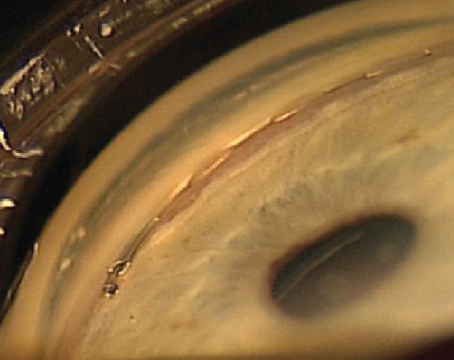
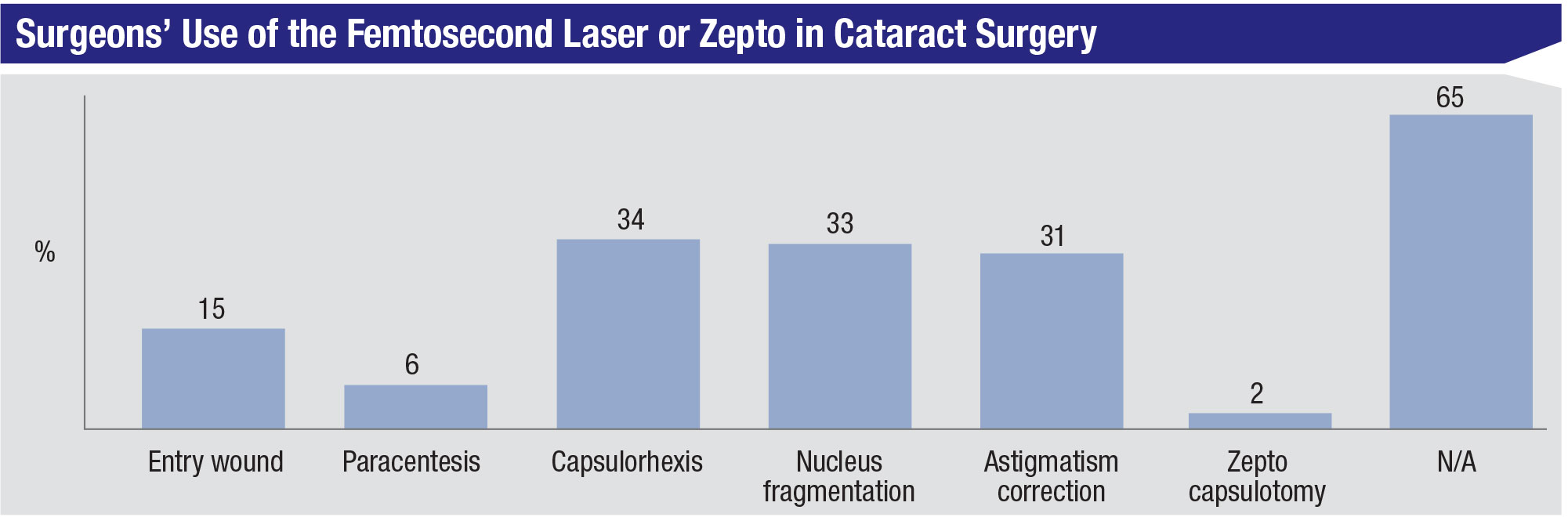
Femto Usage
For the past several years of our survey, surgeons who use either a femtosecond laser or the Zepto capsulorhexis device have hovered in the 33 to 36 percent range, and this year is no different, with 36 percent of the surgeons using one of them. The most popular usage for the femtosecond is capsulorhexis creation (34 percent), though nuclear fragmentation and femto AK incisions are close behind at 33 and 31 percent, respectively (2 percent say they use a Zepto to make the capsulorhexis). The next most popular applications for femto are the creation of the entry wound, at 15 percent, and creation of a paracentesis (6 percent). Twenty-two percent of the femto users say they’ll perform more femto cataract in the coming year, 9 percent will do less and 68 percent will do the same amount.
“Femto is accurate, safe and reproducible,” says Dallas surgeon Jeffrey Whitman. Another surgeon, from Minnesota, likes the Zepto technology, saying, “Zepto is ideal for mature, white cataracts; it makes them routine cases.”
Most of the other respondents, however, don’t appear to be sold on femto or Zepto’s attributes. “I used to perform FLACS but I felt patients didn’t benefit from the laser and it slowed everything down,” says Richard Wieder, MD, of St. Louis. John Willer, DO, of The Dalles, Oregon says, “Femto is a solution looking for a problem. Also, I feel the push towards femto is more financial than what is in the patient’s best interest … I can make my own rhexis and don’t need some overpriced gadget to do it for me.” A surgeon from Kentucky has no plans to use a femtosecond laser for his surgeries. “I don’t like femto because it is expensive,” he says. “It doesn’t improve safety or refractive results and it adds a lot of time.”
 |
Complicated Cases
Surgeons also weighed in on how they manage some sticky situations, such as their approach to fixating IOLs in cases of compromised capsular support and how they deal with small pupils.
For a lens in an eye with no capsular support, the largest proportion of respondents, 44 percent, prefer to use an anterior-chamber IOL. The next most popular option, chosen by 31 percent of surgeons, was the Yamane technique for scleral fixation, followed by scleral fixation by some other method. Iris fixation was chosen by 5 percent.
“The Yamane technique is reliable without significant long-term complications, such as suture erosion,” says a surgeon from New Jersey. A fellow New Jersey physician agrees, saying, “It makes physiological sense.”
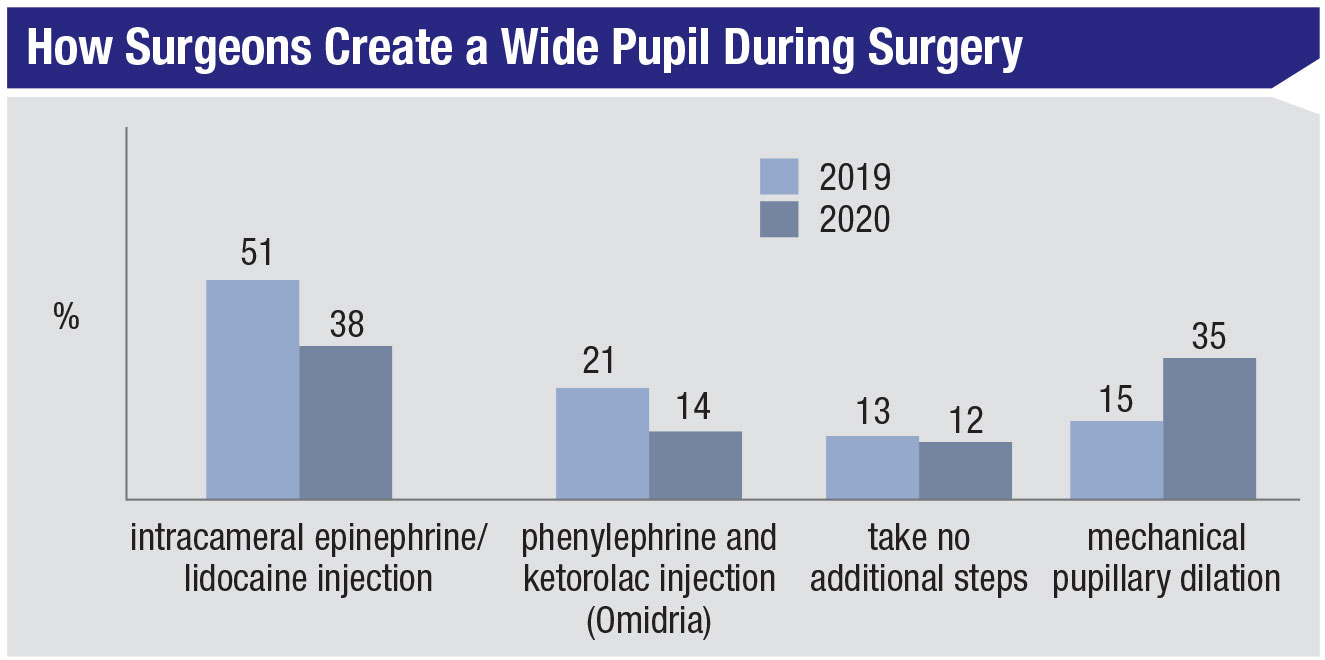
For cases of small pupils, mechanical dilation (mostly with the Malyugin ring) made a big jump this year, going from 15 percent last year to 35 percent. “If you’re thinking about using a Malyugin—use it!” states Inna Ozerov, MD, of Hollywood, Florida. The most popular option is still an intracameral injection of epinephrine and lidocaine (38 percent), followed by the use of Omidria (phenylephrine and ketorolac injection, Omeros), chosen by 14 percent. Twelve percent of the respondents say they take no additional steps in these patients.
 |
Points of Interest
Surgeons also discussed other aspects of surgery, including:
• Intraocular aberrometry. Only 38 percent of the respondents use this technology. Of the surgeons on the survey who do use it, 40 percent rate it as good, and 18 percent say it’s excellent. Twenty-two percent say it’s fair, and 18 percent deem it poor. “It’s great for post-refractive-surgery patients,” says Jonathan Rubenstein, MD, of Chicago. A surgeon from Minnesota agrees, adding that it’s ideal for “aligning the toric IOL axis and IOL power confirmation or adjustment.” Matthew Kruger, MD, of Denver says that though it’s good, “With newer lens formulas, the need for it is less. It takes more time than it’s worth now.”
Andrew F. Kolker, MD, is also less-than-enthused about the technology. “I find it useful [for post-LASIK patients],” he says. “Otherwise, I don’t find it helpful and in fact confusing for toric patients, and not useful in standard cases (it’s not helpful, takes longer and the machine is bulky).”
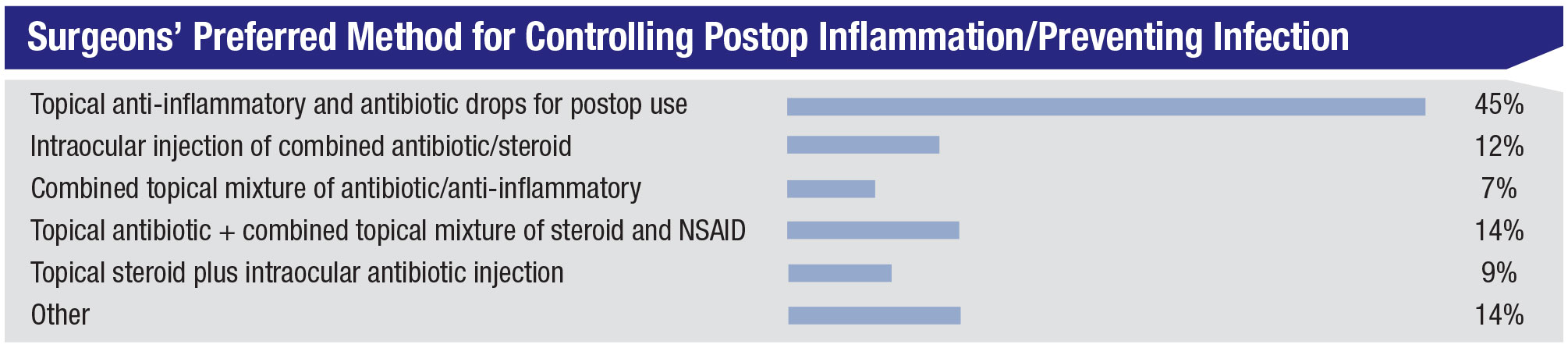
• Postop inflammation/infection control. The most popular approach to this is topical anti-inflammatory and antibiotic drops that the patient uses postop (45 percent). Fourteen percent of the surgeons give a topical antibiotic and a combined mixture of a topical steroid and an NSAID; 12 percent administer an intraocular injection of combined antibiotic/steroid. The rest of the results appear in the graph above. For surgeons who use another method (14 percent), some responses were: subconjunctival injection plus a topical anti-inflammatory; pre- and postop topical antibiotic; postop topical steroids with an antibiotic in the infusion; intraocular antibiotic injection and a sub-conjunctival Kenalog injection; and topical anti-inflammatory and intracameral moxifloxacin.
• Breaking up the nucleus. Thirty-seven percent of surgeons chose quadrant division as their preferred method for breaking up the nucleus, followed by stop-and-chop (21 percent) and horizontal phaco chop (12 percent). The rest of the options were chosen by less than 10 percent of respondents. “Quadrant division works for 90 percent of my cases and has the lowest capsular risk in my hands,” says a surgeon from Minnesota. “It’s safe and predictable,” says Houston’s Dr. Milstein.
The stop-and-chop proponents focus on efficiency and control. “It uses less energy and fluidics,” says a surgeon from Arkansas. Kerry Hunt, MD, in Raleigh, North Carolina, says he likes stop-and-chop because it “facilitates the initial chop.” The horizontal choppers, however, are also outspoken in their affinity for the technique. “It uses the least ultrasonic energy,” says a surgeon from New York. “There’s no peripheral sculpting required. It’s efficient and safe when done with the proper (blunt) instrumentation.” Dr. Kruger agrees, saying, “It works on everything from soft to very hard cataracts. It’s very safe and the surgeon never approaches the posterior capsule.”
• Surgical pearls. As they do every year, the surgeons in our cataract survey shared their best pearls:
• Spend plenty of time and effort with hydrodissection (Richard Wieder, MD, St. Louis);
• Maintain excellent visualization at all times;
• When checking the keratome incision for leakage don’t forgot to check the paracentesis, as this may leak at the end of surgery (Max Walsh, MD, Royal Oak, Michigan);
• Lift the iris off the lens for an overly deep chamber;
• Relax and keep your eyes open for subtle operative field changes;
• Use a corneal marker to ensure accurate reproducible rhexis size (Stewart Galloway, MD, Crossville, Tennessee);
• When sculpting, always start less deep centrally; you can always deepen your groove if you can’t crack it (Dr. Kolker); and
• When that voice in your head tells you that something isn’t right, listen to it and take precautions. Don’t plow ahead as usual. REVIEW