To mitigate transmission of the coronavirus, practice social distancing and keep their practices afloat financially during the pandemic and subsequent business shutdown, some practices are turning to telemedicine to continue seeing patients and provide non-emergency care. Transitioning to telemedicine during this stressful time may not be ideal for every practice, but those who have added, or are considering adding telemedicine to their practices may find it a good long-term investment. Telemedicine can offer patients—especially the elderly—peace of mind during the quarantine, experts say. You may even identify an early case of coronavirus during your virtual visit. Here, we’ll discuss some of the logistics of telemedicine so you can decide if it’s right for your practice.
Feeling the Impact
No matter which steps practices take regarding coronavirus safety—whether it’s taking patients’ temperatures as they enter, spacing out patients in the waiting room, turning away those with suspected coronavirus symptoms, proceeding as usual in less-affected regions or following the AAO’s guidelines to stop all non-urgent, routine visits—they’re all feeling the financial effects of reduced patient volume. Many have had to lay off or furlough staff. In coronavirus hotspot areas, like New York City, some practices have closed their doors.
“Routine visits across the country for ophthalmology have largely come to a halt,” says Ingrid E. Zimmer-Galler, MD, associate professor of ophthalmology at Johns Hopkins and executive clinical director of the office of telemedicine. “That’s why everyone’s so interested in using telemedicine—we can reach out to patients that we otherwise can’t see in the office.”
Some telehealth companies are responding to the pandemic by offering their services to physicians free of charge. EHR tech company Modernizing Medicine has offered its platform, Modmed Telehealth, to current and future users,1 and ImprimisRx recently announced an exclusive partnership with Doxy.me, another telehealth platform.2
“The real-time audio/video capabilities of telemedicine allow doctors to keep their doors virtually open, even though their offices might be shuttered,” explains Nikola Ragusa, MD, FACS, an ophthalmologist at the Bronx Eye Center in New York and chief medical officer of the startup telemedicine app Pulse.
Dr. Ragusa says that interest in and use of telemedicine corresponds with the growing concern over the pandemic. Prior to the pandemic, he says, calls using his product ranged on average from about five to 10 per month per physician. Now, physicians are fielding about 30 calls per day. “This can generate close to $3,000 per practice per physician,” he says. “It’s probably not the typical revenue generated by patient visits, but it’s something to help keep businesses afloat.”
Paradigm Shifts
The pandemic will leave its mark on everyone around the country. One concern physicians have raised is the degree to which pandemic-era behavior and anxiety might impact future patient care. Kathryn Colby, MD, Louis Block professor and chair of the department of ophthalmology and visual science at the University of Chicago Medicine & Biological Sciences, notes that “Just this morning in a virtual meeting, someone brought up the question: What if patients don’t want to come back into the office after all this? After we say we’re open for business, please come back, what if patients don’t want to? Most ophthalmology patients are older and that would put them at a higher risk for infection. I think that once we have serological testing routinely available to demonstrate immunity, people will feel more comfortable resuming some of their daily activities.”
Visits from a Distance
Pandemic-era telemedicine focuses more on practice management and routine cases than typical ophthalmic telemedicine, which has traditionally focused on remote monitoring and portable imaging, often in underserved regions.
“I have a retina practice, so it’s very difficult for me to do my job with telemedicine visits when it comes to monitoring patients who have diabetic retinopathy or macular degeneration,” says Dr. Zimmer-Galler. “You can’t really do that with a simple video visit, but we can do a lot of follow-up on patients and determine who needs to come in.”
When patients do need to come into the office, experts say it’s a good idea to spread them out over the entire day, with just one patient in the office at a time. Using telemedicine for follow-up visits is another way to reduce patient volume.
 |
“One good thing to come out of this will be the use of telemedicine for a significant number of our postoperative exams,” says Alan Aker, MD, who runs the Aker-Kasten Eye Center with his wife, Ann Kasten, MD, in Boca Raton, Florida. “Because of the pandemic, we’ve been forced to provide these postop checks via telemedicine. We’ve realized that following uneventful, well-performed surgery, patients who are doing well after the initial one-day visit can be screened by phone at the one-week and later visits. Any patient wishing to be seen, or who seems to be having an issue, can be scheduled. Eliminating a great number of routine but often cumbersome visits for our staff and our patients will enable us to streamline our postop visits. Our staff and our doctors will have more time to spend with those few patients who are having issues following surgery.
“Patients traveling long distances will benefit from this as well, saving travel time and the expense associated with that,” he continues. “I see this as a very significant and positive change we will institute once the pandemic has passed. In addition, I think we’ll begin to provide emergent telemedicine care for select patients. An example of this would be the patient who wakes with a subconjunctival hemorrhage and calls with great concern. These patients might prefer to be seen in person because of the concerns they have, but that could be handled on a case-by-case basis. As video is added to our systems for remote care, we can probably begin to provide more timely care and more compassionate care without the significant waits associated with being an ‘add on’ to our busy clinic schedules.”
Here are some at-a-glance ways that users say telemedicine can help your practice during the pandemic.
• Keep your patients safe. Slit lamp exams are hotbeds for viral transmission. Additionally, senior patients and those with underlying health conditions will benefit from not having to come into the office or health-care facility.
• Triage. Telemedicine can help you check in on your follow-up patients as well as screen patients who call with concerns. “One of the big things we’re trying to determine is who really does need to come in [to the office],” Dr. Zimmer-Galler says. “You want to make sure you’re not missing someone who’s had a change in vision and then their visit is postponed.”
• Lower overhead. Reducing costs during this time is important. Telemedicine requires only internet access. “One telemedicine visit costs a practice around $5, versus the typical overhead of anywhere from $50 to $75 per [office] visit,” says Dr. Ragusa.
• General exams. Telemedicine is more difficult for certain subspecialties, such as retina and glaucoma, but for less subspecialty-oriented issues that involve the front of the eye or the eyelids, televisits with video can be as effective as in-person exams. Dr. Zimmer-Galler says that benign problems such as a chalazion, sty, red eye and subconjunctival hemorrhage can be anxiety-provoking for patients, but adds that, “Those are things where you really could do as good an examination with a video visit as you can in person. Video visits add an extra element that you miss out on in a phone conversation, just by being able to see the patient.”
• Patients accept it. “They’re delighted with it,” Dr. Zimmer-Galler says. “They like being able to see their providers. Once providers are more comfortable with telemedicine, I think they’ll see that it’s really not a bad way to go. More and more patients are going to expect these types of services, so I think we need to embrace it in ophthalmology once we get past this emergency.”
Dr. Ragusa adds that patients also enjoy being able to communicate with their doctor from their homes. “When I sign patients up, it’s not like I’m getting non-stop calls,” he says. “They just like the comfort of knowing they can reach me, and I like having the comfort of knowing I can reach them and check in, especially during this time, since many of my patients are elderly.” Dr. Ragusa says he had a televisit with an elderly, febrile patient whom he suspected of having COVID-19. “She wasn’t sure if she should go to the ER,” he says, “but by the end of our call, she had significant shortness of breath and we decided she should go.” She ended up testing positive for COVID-19.
Temporary CMS Changes
The temporary changes made by the Centers for Medicare and Medicaid Services have relaxed several telemedicine regulations. These changes will make telemedicine easier to incorporate and use on short notice and during the COVID-19 emergency. “We can do much more from a billing standpoint with the CMS updates for telemedicine visits at home,” says Dr. Zimmer-Galler. “Prior to this emergency, CMS wasn’t allowing any telemedicine video visits with patients at home. That’s one of the big changes and what makes telemedicine more viable for ophthalmologists.”
She adds that, “in order to meet all of the billing requirements in ophthalmology, you have to look carefully at the elements needed for the exam. You also still need to do your documentation in your electronic record and obtain patient consent.”
Here are some important changes to health-care laws:
• 1135 Waiver. According to the CMS, under the 1135 waiver, Medicare will pay for office, hospital and other visits through telehealth.3 Clinicians can bill immediately for dates of services starting March 6, 2020.
• HIPAA requirements have been waived. CMS has waived HIPAA and site-of-service requirements. No penalties will be imposed. This means doctors and patients can communicate over platforms such as Facebook Messenger, FaceTime, Zoom, Skype and Google Hangouts. Be sure to document your virtual visit carefully. (See sidebar below.) Though these options are available, experts recommend that if you’re looking to stay with telemedicine after the pandemic, it’s a good idea to use a HIPAA-compliant telemedicine service from the get-go. “What we don’t want is for providers to get so caught up in all of this that they then forget about the HIPAA requirements once the waiver expires,” says Dr. Zimmer-Galler. “Take up telemedicine now as if these relaxed regulations weren’t in place.”
• State parity laws. Telehealth services will be billed under the Physician Fee Schedule at the same rates as in-person services. Medicare coinsurance and deductibles will still apply for these services. Health-care providers may reduce or waive cost-sharing for telehealth visits paid by federal health-care programs.4
• Consulting across state lines. Licensure requirements have also been relaxed to allow telemedicine to span state lines.
• Accelerated and advance payments for Medicare. CMS also announced in late March an expansion of the accelerated and advance payments program for providers and suppliers during the pandemic. This means that practices can apply to their Medicare Administrative Contractors to receive their entire Medicare payment amount for a three-month period, calculated on historical payments. MACs will issue payment within seven days.5
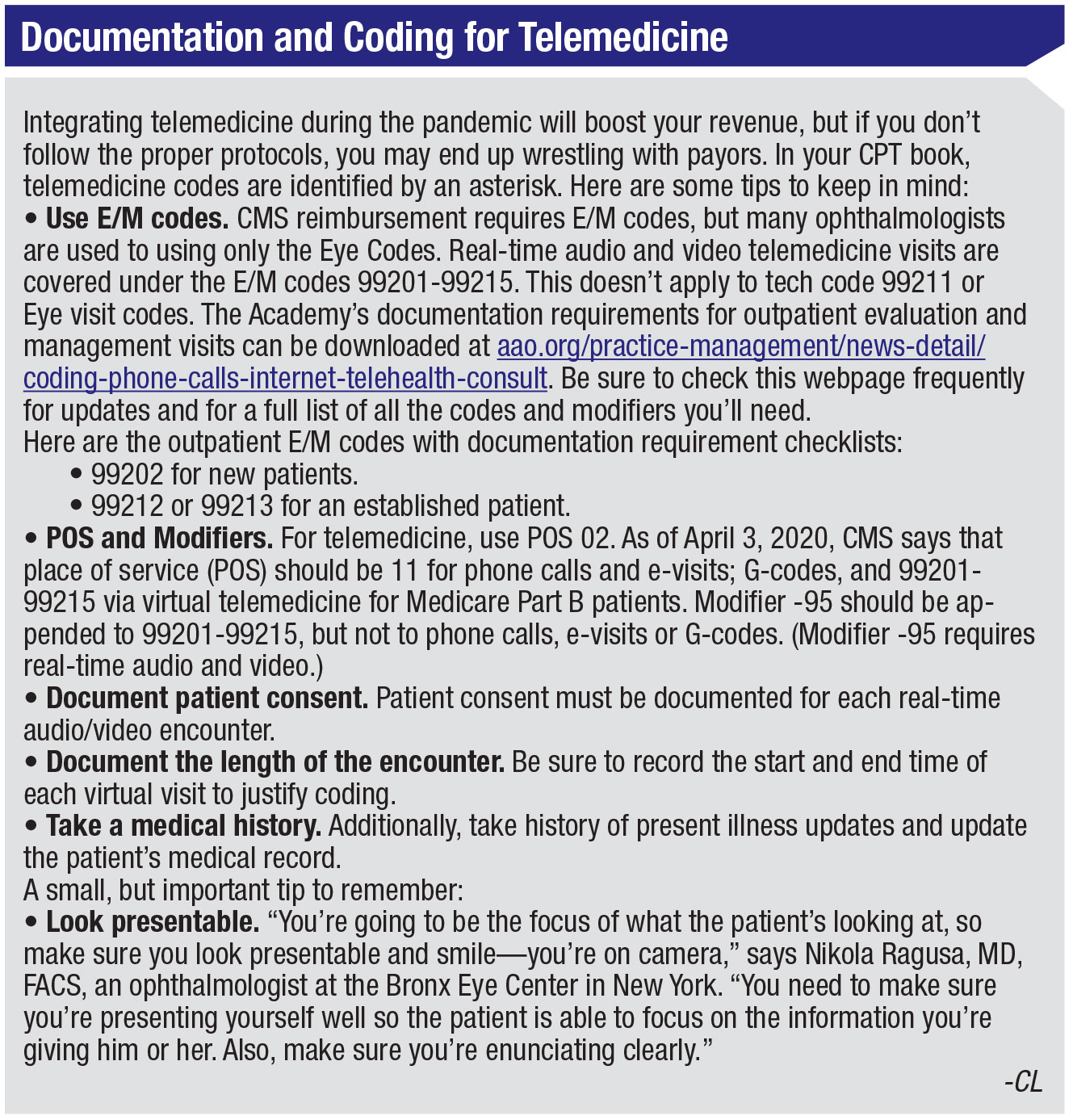 |
| www.aao.org/practice-management/news-detail/coding-phone-calls-internet-telehealth-consult |
Telemedicine and Patients
Today, almost all phones and tablets have high-quality cameras, which come in handy for virtual visits and examinations, but one concern some physicians have is the ability of their elderly patients to use technology for virtual visits. Dr. Ragusa finds that for the most part, the elderly aren’t technologically inept. “They’re used to FaceTiming with their grandchildren,” he points out. “Many elderly patients are perfectly capable of using telemedicine.”
Nevertheless, it’s a good idea to have your patient’s phone number on hand. “If you try to connect by video visit, but you’re not able to make the video visit work, you want to make sure you have the patient’s phone number so you can easily convert it to a phone visit,” says Dr. Zimmer-Galler. “Add Modifier -52 for a phone visit, and you can still get reimbursed for that.”
Dr. Zimmer-Galler says it’s important to choose a telemedicine service that’s easy for patients to use. Likewise, you want to start out with patients who are likely candidates for telemedicine. (Those who still use flip phones might not be the best choices when you’re still learning how to navigate the new system.) Many integrated EHRs have telemedicine platforms built into them—but while that’s easy on the provider’s side, it’s not so simple for many patients. “From the patient’s side, you have to first be activated on the patient portal, then go through various steps to test your device to make sure it works,” she says.
Additionally, it’s important to let patients know upfront that a telemedicine visit is a bit different from an in-person visit, but a visit nonetheless. “I can’t do all the things I would normally do,” Dr. Zimmer-Galler says, “but you want patients to understand and not be surprised that they’re getting a bill from a virtual visit. In medicine, we’ve traditionally provided so many services by phone for free that patients are used to us doing them for free. When you start billing for something that’s outside the office, you just want patients to realize that it’s really a visit.”
The Virtual Eye Exam
To assist with the exam, Dr. Ragusa says you may be able to coordinate the virtual visit with a person the patient feels comfortable with—such as a home-health aid or a spouse. The other person may help position the camera for viewing external structures, lifting eyelids or visualizing a red reflex.6
“It takes practice,” Dr. Ragusa says. “Doing an eye exam with a smartphone instead of a slit lamp is strange. You’ll probably fumble through the first few patients until you get an idea of how to do it. You have to be creative when checking vision, visual fields and obtaining pressure.”
The AAO recommends performing the external exam, pupils, eye movements and alignment and pen light anterior segment with a camera. Patient selfie images for documentation can also be shared, but aren’t separately billable. The AAO has printable instructions available online for patients testing their vision at home. Snellen charts for adults and children, as well as an Amsler grid, are available at aao.org/eye-health/tips-prevention/home-eye-test-children-adults.
For confrontation visual fields, Dr. Ragusa says he pulls back from the camera to demonstrate to the patient how to perform the test, so they can do it on themselves.
The biggest challenge by far is checking intraocular pressure. If patients are trained to use and have an iCare tonometer, at home, checking pressures is easy. If not, Dr. Ragusa asks patients to do rebound tonometry. “I ask if their eye feels soft like a grape, a little harder like a tomato or hard like an apple. Luckily, most patients say their eyes feel like grapes, which is about normal eye pressure. It’s not a perfect method, but you have to get creative.
“[Remote eye exams are] problematic for patients with retinal issues complaining of increased floaters or decreased vision from something in the posterior pole,” Dr. Ragusa admits. “They’ll likely need a fundus exam in the office. But the beauty of telemedicine is that you’re still able to triage them at home, offer them comfort and give patient education in these hard times.”
Some Telehealth Options
Incorporating telemedicine into your practice—especially during this time—can help keep your practice afloat, minimize the risk of exposure for your patients and staff and allow you to reach vulnerable patient populations who can’t make it to the office. Here are some telemedicine options:
• Modmed Telehealth is at the time of this writing, temporarily being offered at no charge, with all sign-up and utilization fees waived, to current and future users of Modernizing Medicine’s electronic health records system, EMA. Modmed Telehealth features high-resolution, real-time audio/visual chat. Doctors and patients can virtually attend scheduled appointments with a new version of the PocketPatient app. The app is available for both iPhone (iOS12 and above) and Android (v. 7.0 and above). For information, visit modmed.com/telehealth.
• Doxy.me is a free telemedicine service with audio, video and text communication capabilities. The service is internet-based, with no software to download. It’s compatible with Android and iOS and can be integrated with most EHRs or practice management software. Some of the features include a virtual waiting room, remote file sharing, image capture and prescription delivery through ImprimisRx’s mail-order pharmacy. ImprimisRx’s agreement with Doxy.me will provide all ImprimixRx ophthalmology, optometry and wellness practices with the clinic-level version of Doxy.me at no charge. Paid tiers offer additional security and encryption. The Professional tier is $35 per month, the Clinic tier is $50 per month, and the Basic tier is free. All tiers are HIPAA-compliant. For information, visit doxy.me.
• Pulse is a health-care startup telemedicine app designed specifically for private practices. The Pulse One app features HIPAA-compliant real-time audio/video chat and uses metadata to document patient consent, disclaimers and when the call took place, which is then compiled into a report for each visit. The developers say Pulse is designed to deploy in a few hours. For information, visit pulsett.com.
• Mend is a full-feature telemedicine suite with HIPAA-compliant audio and video aimed at increasing a practice’s efficiency and profitability by reducing the number of missed appointments. Some features include SMS appointment reminders, online forms, patient self-scheduling, video and voice calling, survey and review options and automated workflow processes. Mend claims that its AI program can also predict no-shows and cancellations, “days and weeks before they happen.” The program integrates with most EHR and practice management software. Monthly subscriptions per provider are $59; annual subscriptions, per provider per month, are $49. Custom quotes are also available. For information, visit mendfamily.com.
Though reaching for telemedicine at the current time may be motivated by panic about maintaining a semblance of normalcy during the maelstrom, physicians say that, in the calmer waters of the future, the habits practices develop now may carry forward. “I’m hopeful that once the emergency ends, we’ll continue to be able to use telemedicine in a variety of ways,” says Dr. Zimmer-Galler. REVIEW
1. Modernizing Medicine to launch telemedicine solution to provide real-time audio and video capabilities to help healthcare professionals care for patients. Modernizing Medicine. Press Release. March 16, 2020. https://www.modmed.com/press-release/video-telemedicine-solution/.
2. ImprimisRx announces exclusive agreement with Doxy.me to provide healthcare professionals with telemedicine services. Press Release. March 24, 2020. https://www.globenewswire.com/news-release/2020/03/24/2005411/0/en/ImprimisRx-Announces-Exclusive-Agreement-with-Doxy-me-to-Provide-Healthcare-Professionals-with-Telemedicine-Services.html.
3. Medicare telemedicine health care provider fact sheet. CMS. Accessed 30 March 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet.
4. President Trump expands telehealth benefits for Medicare beneficiaries during covid-19 outbreak. CMS. Accessed 30 March 2020. https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak.
5. Fact sheet: Expansion of the accelerated and advance payments program for providers and suppliers during the covid-19 emergency. CMS.gov. Accessed 30 March 2020. https://www.cms.gov/files/document/Accelerated-and-Advanced-Payments-Fact-Sheet.pdf.
6. Coding for phone calls, internet and telehealth consultations. AAO. Accessed 7 April 2020. https://www.aao.org/practice-management/news-detail/coding-phone-calls-internet-telehealth-consult.





