When preparing the ocular surface for LASIK, one must make many considerations. Two of the most important factors to be aware of are the presence of ocular allergy and dry eye. Surgeons need to consider these conditions in order to create the healthiest scenario possible before surgery and to assure the best outcomes. Here, we'll discuss the prevalence of these conditions in LASIK patients, look at research into connections and devise the best approaches for dealing with such cases.
The Allergy and Dry-eye Overlap
• Allergy. Seasonal allergies may be perceived by patients as a nuisance, but not a significant threat to their sight. For those planning to undergo refractive surgery, though, it's time to think otherwise.
Allergic conjunctivitis affects over 50 million people in the United States. When combined with rhinitis and other forms of allergy, an estimated 30-40 percent of the population is affected.1 This staggering prevalence has dramatic consequences for economics, quality of life and health. Ocular allergy often aggravates dry eye, compromises contact lens wear, and can be present with glaucoma and other ocular diseases, necessitating multiple therapies. These therapies can lead to contact lens intolerance, irritation and even medicamentosa.
 |
| Detection of dry eye preop helps you get the best possible corneal surface. |
• Dry eye. The scenario with dry eye is similar to that of allergy in terms of patients undergoing LASIK. Dry eye can also make contact lens wear intolerable, leading patients to choose LASIK. Though, like allergy, dry eye can be erroneously perceived as a miscellaneous annoyance, it is, in fact, important when preparing the ocular surface for LASIK.
Symptoms of dry eye are prevalent, to some degree, in nearly everyone. Epidemiological studies have revealed clinically diagnosed dry eye in up to 28 percent of a general population.2 This number jumps to more than 75 percent when looking exclusively at a population planning to undergo LASIK. One study identified 35 percent of prospective LASIK patients as having "definite" dry eye, while an additional 41 percent had "probable" dry eye.3
Allergy, Dry Eye and Refractive Surgery
A handful of studies have been examining the possibility of the allergy-LASIK connection. Compromised visual outcome after refractive surgery is thought to be due to an overactive immune response to the corneal trauma inflicted. For instance, subepithelial corneal haze after PRK has long been considered an exaggerated healing response. Late-onset haze is a troublesome complication of PRK, as it's usually accompanied by a regression of effect.
In the quest for predictive factors for haze, clinicians suspected a correlation with allergic conjunctivitis. In one study, a significant correlation was observed between untreated allergic conjunctivitis and the development of late haze.
Patients had either no ocular allergy, were treated for ocular allergy, or had untreated ocular allergy for the entire 18-month follow-up period. Regression in visual outcome was remarkably greater in the allergic, non-treated patients: only 36.4 percent of patients in this group maintained their visual outcome compared to all of the normal subjects and 93.8 percent of treated allergic patients.4 The authors speculated that, in PRK, cytokines and growth factors are released from injured epithelial cells, activating stromal keratocytes to synthesize new collagen. This process is thought to cause myopic regression, astigmatism and haze, and is accentuated in the allergic patient in whom pro-inflammatory and hyperproliferative mediators are prominent.
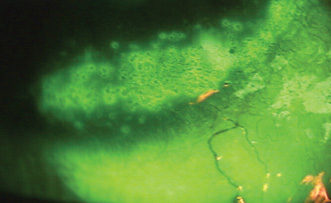
Today, the most common refractive surgery is LASIK. LASIK patients experience minimal postoperative pain and enjoy a quick visual rehabilitation. Postop inflammation and wound-healing responses tend to be minimal. While the chances of a stable visual outcome have greatly increased with today's technology and advanced surgical technique, LASIK still has the potential to be associated with diffuse lamellar keratitis, however. DLK can be observed soon after surgery, initially as a granular infiltrate along the stromal lamellar interface. This can either progress over the next few days and then resolve, or it can persist into more severe stages.
In 2001, research explored the correlation of allergic conjunctivitis with LASIK complications. These investigators found that complications, refraction and uncorrected visual acuity weren't different in the allergic and non-allergic groups.5 The follow-up period in this subsequent study, however, was only six months, and significant results may have occurred further out in time.
Challenging the conclusions of this paper is a more recent report published in 2003.6 By specifically identifying in 360 LASIK patients the presence of atopy of any type, and from other sites of origin such as asthma or rhinitis, researchers identified a statistically significant correlation of DLK with atopy.
The study doctors recorded patients' allergies and any anti-allergy medications they were taking. A subgroup of atopic patients were taking the oral histamine H1 antagonist, loratadine (Claritin, Schering-Plough) or fexofenadine (Allegra, Aventis) at the time of surgery. Findings were dramatic: The risk of DLK among untreated atopic patients was five times greater than among non-atopic patients, while there were no differences between treated atopic patients and non-atopic patients. Thus, treatment of allergy significantly altered the risk of DLK. The surgeon may be able to decrease the risk for DLK further with the use of a topical anti-allergy agent.
It's interesting to note that these significant findings pertained to patients treated with systemic antihistamines. Yet, we know that use of these antihistamines, even the newest generation of them, is associated with drying of the ocular surface, an event that's counterproductive to corneal healing.7 In a study we conducted, loratadine increased keratitis by 122 percent, decreased Schirmer wetting by 6.5 mm, shortened tear breakup time by 53 percent and increased subjective symptoms of ocular discomfort.8 Consequently, the use of oral antihistamines that dry the eye shouldn't be recommended to a population already predisposed to chronic dry eye. This leads us to the discussion of dry eye and LASIK.
The strategy for dealing with pre-LASIK dry eye is similar to that used with allergy: Detection prior to the procedure is essential in preparing the healthiest possible ocular surface. Post-LASIK dry eye is an entirely different matter, however.
Most patients who undergo LASIK, regardless of their dry-eye status prior to surgery, do experience some dryness afterwards. Even in normal non-allergic LASIK patients not treated with antihistamines, one study reported as much as 85.4 percent of the population with dry-eye symptoms one week after surgery, and 43 percent of PRK patients and 48 percent of LASIK patients with symptoms six months postop.9,10 Additionally, there can be decreases in the lipid layer, goblet cell density, Schirmer measurements and tear-film breakup time.11-13
Studies have shown that the effect on existing dry-eye patients who have LASIK is more severe. One study evaluated 543 eyes that underwent LASIK; all patients were categorized as "definite," "probable" or "without" dry eye pre-LASIK. Upon examining the tear function of these groups after LASIK, it was found that the dry-eye group had the most compromised tear function. Specifically, this group had more staining, lower Schirmer scores and shorter tear-film breakup times.14
The driving force behind these events is the indisputable fact that LASIK involves the severing of corneal nerves, essentially creating surgically induced neurotrophic keratitis. This means corneal sensitivity is reduced, setting the stage for continued dry eye. The decrease in corneal sensitivity, along with the new interaction between ocular surface and lid, can cause changes in blink rate, decreased TFBUT, decreases in tear production, reflex tearing, and production of mucins by goblet cells that leave the ocular surface unprotected.
Prevention
One highly effective way to minimize the detrimental effects that allergy and dry eye can have on LASIK outcomes is to take preemptive steps. Getting patients into a routine that manages signs and symptoms of allergy or any existing discomfort due to dry eye is a valuable way to do this.
If you identify dry eye prior to LASIK, the primary goal leading up to surgery is to achieve as healthy an ocular surface as possible. An increased regimen of artificial tears will help and can be continued postop. Acclimating patients to this type of schedule as early as possible before surgery is helpful not only in preparing the ocular surface for LASIK, but in developing the habit of using the drops with enough frequency so as to prevent dry-eye symptoms from becoming a problem after LASIK.
It appears that the best approach for ocular allergic LASIK candidates is the same as that for all ocular allergic patients: local therapy. These patients can benefit substantially from a local ophthalmic preparation in the perioperative period. New generation anti-allergic agents prevent the release of histamine, cytokines and other pro-inflammatory and proliferative mediators such as those involved in corneal trauma and healing (IL-8, ICAM-1).15,7 As a rule, these patients are better treated with local anti-allergic agents such as mast-cell stabilizer/antihistaminic solutions that won't compromise, and may even enhance, corneal wound healing. For example, agents such as olopatadine have been shown to decrease the release of tryptase from mast cells in vitro. In human clinical study, these agents stabilize the conjunctival mast cells.16,17
Similar to the routine of artificial tears for dry eye, a regular regimen of anti-allergy eye drops before LASIK can get patients out of the habit of rubbing their eyes, decreasing the risk of their continuing to do so after LASIK and dislocating their flaps.
Careful identification of allergy and dry eye is naturally an important step in optimizing the success of LASIK. Specific medication history concerning the use of oral antihistamines, over-the-counter ocular allergy drops and/or nasal sprays is essential for identifying allergy. Assess the location and severity of allergy.
An accurate assessment of tear-film status may also be predictive for postop dry-eye symptoms. Since allergy and dry eye can sometimes be confused, this would allow for a precise differential diagnosis in ambiguous cases. You can optimize ocular surface health by discontinuing oral antihistamines in the preop period and by supplementing a typical LASIK medication regimen with potent topical anti-allergy therapy or artificial tears.
Recognition of allergy and dry eye as risk factors for LASIK complications is something that takes little time or effort, but has significant effects on the surgical outcome. It allows for the identification of a patient subset who may benefit from preop prophylactic therapy and closer postop observation. If in doubt, it's better to treat the eye than to not treat it and run the risk of complications.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Smith and Ms. Fink are research associates at Ophthalmic Research Associates in North Andover.
1. Bielory L. Update on ocular allergy treatment. Expert Opin Pharmacother. 2002;3:541-553.
2. Caffery BE, Richter D, Simpson T, Fonn D, et al. CANDEES: The Canadian dry eye epidemiology study. Adv Exp Med Biol. 1998;438:805-806.
3. Shimazaki J. Definition and criteria of dry eye. Ganka. 1995;37:765-770.
4. Yang H-Y, Fujishima H, Toda I, et al. Allergic conjunctivitis as a risk factor for regression and haze after photorefractive keratectomy. Am J Ophthalmol 1998;125:54-58.
5. Asano-Kato N, Toda I, Hori-Komai Y, Tsubota K. Allergic conjunctivitis as a risk factor for laser in situ keratomileusis. J Cataract Refract Surg 2001;27:1469-1472.
6. Boorstein SM, Henk HJ, Elner VM. Atopy: a patient specific risk factor for diffuse lamellar keratitis. Ophthalmology 2003;110:131-7.
7. Abelson MB. Evaluation of olopatadine, a new ophthalmic anti-allergic agent with dual activity, using the conjunctival allergen challenge model. Ann Allergy Asthma Immunol 1998;81:211-218.
8. Nevius JM, Abelson MB, Welch D. The ocular drying effect of oral antihistamines (loratadine) in the normal population—an evaluation. Invest Ophthalmol Vis Sci 1999;40:4:S549.
9. Yu EY, Leung A, Rao S, Lam DS. Effect of LASIK on tear stability. Ophthalmology 2000;107:2131.
10. Hovanesian JA, Shah SS, Maloney RK. Symptoms of dry eye and recurrent erosion syndrome after refractive surgery. J Cataract Refract Surg 2001;27:4:577-84.
11. Patel S, Perez-Santonja JJ, Alio JL, Murphy PJ. Corneal sensitivity and some properties of the tear film after laser in situ keratomileusis. J Refract Surg. 2001 Jan-Feb;17:1:17-24.
12. Albietz JM, Lenton LM, McLennan SG. Effect of laser in situ keratomileusis for hyperopia on tear film and ocular surface. J Refract Surg. 2002;18:2:113-23.
13. Battat L, Macri A, Dursun D, Pflugfelder SC. Effects of laser in situ keratomileusis on tear production, clearance and the ocular surface. Ophthalmology. 2001;108:7:1230-5.
14. Toda I, Asano-Kato N, Hori-Komai Y, Tsubota K. Arch Ophthalmol 2002;120:1024-1028
15. Yanni JM, Stephens DJ, Miller ST, et al. The in vitro and in vivo ocular pharmacology of olopatadine (AL-4943A) and effective anti-allergic/anti-histaminic agent. J Ocular Pharmacol 1996;12:389-400.
16. Sharif NA, Xu SX, Miller ST, Gamache DA, Yanni JM. Characterization of the ocular antiallergic and antihistaminic effects of olopatadine (AL-4943A), a novel drug for treating ocular allergic diseases. JPET 1996;278:3:1252-61.
17. Leonardi A, Abelson MB. Double-masked, randomized, placebo-controlled clinical study of the mast cell stabilizing effect of treatment with olopatadine in the conjunctival allergen challenge model in humans. Clin Ther 2003;25:10:2003: 2539-2552.



